Addressing Health Care Access in Sonoma County -- 2007-08
advertisement

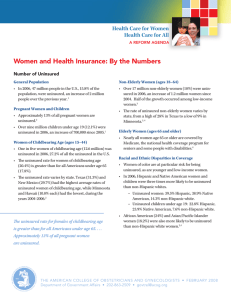
Addressing Health Care Access in Sonoma County-- 2007-08 Presentation at Sonoma State University: March 3, 2007 Gil Ojeda, Director CA Program on Access to Care University of California Office of the President Point of View 35 years in health care delivery and research Past national, state-level and community advocate Advisor to the Legislature and the University; past advisor to community groups and public HMO’s Analyst in the health sciences, public policy and the competitive marketplace Resident of Sonoma County since 1995 Elements of California’s Health Care Marketplace Regional market issues: “most health care is local & regional” Rural & urban imperatives: “most problems & their solutions are situational” Public & private sector roles: “there’s a fabric of relationships & conflicts; dialogue is key” Regulation vs. market competition: “continuum from the prison to the jungle to the game preserve” Delivery of care & the public’s health: “driven by demand, but limited by resources” Diversity & Age: “California’s minorities & the aged often generate program imperatives” The Art of Public Solutions Allocation of public resources : “driven by public budgets, private roles, profits & political advantage” Relative power of constituency groups: “health plans, providers, employers & healthcare advocates” The Governor & the Legislature: “the Governor is now the leading player since he has acted” Natural allies & strategic partners: “must be guided by common goals, opportunities, and intentionality” Federal Support: the Post Nov ‘06 Change in Posture to ABC: “Anything but California” Coming debates on Medicaid & Children’s Health Insurance (S-CHIP): “funding authorizations, overlapping mandates & a rush to reduce entitlements” Changes to Medicare: “proposed rate reductions, prescription drugs plans, & the shift to managed care” Access to care for underserved: “more community clinic support, higher likelihood of direct support for uninsured” The Coming Storm? California’s Leading Edge Healthcare Issues Increasing cost of employer based coverage: “increased premium inflation, economic slowdown, expanded self & temporary employment” 6.5 million uninsured: “is increasing again; public solutions being debated” Ethnicity and income-driven disparities: “California’s diversity & the unemployed as key factors in health outcomes” Managed care/HMO’s: “Many are doing well by avoiding risk & competition; in a balancing act for State collaboration and oversight” Physicians and hospitals-at-risk: “lower reimbursements, higher financial risks, system inefficiencies” Nursing and specialist shortages: “still out of control, worsened by recent policies; few short-term, some long-term solutions” State budget deficits: “last year & this year, may compromise efforts to expand coverage to millions of uninsured” Health Care Reforms: County Roles in Expanding Coverage Healthy Kids programs implemented throughout state including in this county Board appointed task force considering stand-alone or multi-county options for managing all Medi-Cal enrollees Sutter inpatient closure places current County indigent care arrangements in jeopardy. Can Memorial Hospital step up? Continued loss of physicians from county jeopardizes any efforts to preserve or expand health care coverage. State level, “shared pain”, effort to bring local low & middle income uninsured, including undocumented, under coverage has chance for passage in 2007-08. Will county's public and private sectors be ready? Cooperative dialogue among the various sectors, including Kaiser Health Plan, offers best hope for county's successful expansion under framework of new state reform plan Considerations as We Go Forward What part of the problem are we trying to fix OR do we think we can fix it all? Who are the natural institutional allies for health care reforms or are consumers, employers & other health care advocates ready to go it alone? What can we do locally in the short term? How can we leverage State & federally mandated changes?