Gadgets for good: How computer researchers can help save lives in poor countries
advertisement
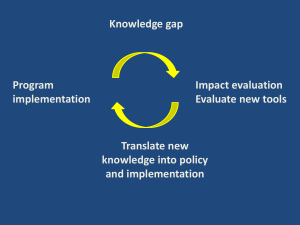
Gadgets for Good How Computer Innovation Can Help Save Lives in Low-Income Countries. Neal Lesh Harvard School of Public Health ~40 million HIV infected people ~3 million died in 2004 ~9 years on ave. to live w/o treatment ~6 million need treatment >75% unaware of status ~700,000 receiving treatment ARVs Samuel Morin, 2001, Haiti One year later, after treatment Clinical staff using Partners in Health’s EMR in Belladere, Haiti. Roadmap me the world international public health computers me My Background • Computer science experience: – 1991-1997: PhD in A.I. at U. Washington – 1997-1998: postdoc at U. Rochester – 1998-2004: research at MERL • Areas of work: – planning – story sharing – collaboration – optimization – data mining – engagement – indoor navigation – inference intention – probabilistic reasoning – information visualization – intelligent tutoring – data exploration Currently • Full-time student, masters of public health (MPH) – taking classing, field trip to India, starting some research projects. • Goals for this talk: – Give you flavor of the field – Generate excitement – Get invited back in a couple years Warning! • Many approximations: “There is a tendency for all knowledge, like all ignorance, to deviate from the truth in an opportunistic direction.”—Gunnar Myrdal. • Neglecting lots, e.g. – disadvantaged people in rich countries • Glossing over a lot of complexity • Assuming you know about what I did 1 year ago How are we doing? ~six billion people World Population Growth Population and year Time to add a billion 1 billion in 1804 2 billion in 1927 3 billion in 1960 4 billion in 1974 1,001,804 years 123 years 33 years 14 years 5 billion in 1987 6 billion in 1999 7 billion in 2012 13 years 12 years 13 years 8 billion in 2026 8.9 billion in 2050 14 years 26+ years How are we doing? How are we doing? one billion people in rich countries five billion people in middle- or low-income countries Poverty as a Risk Factor for surviving the Titanic. 70 % survived 60 50 40 30 20 10 0 1st 2nd class of service 3rd Poverty as a Risk Factor for dying young. Malawi U.S. Life expectancy at birth 38 yrs. 77 yrs. Prob. of dying before 5 years old. 18.3% .8% Prob. of dying before 40 year old. 49.8% 13% die before 60 yr. HIV rate among 18-49 year olds (2001) 15% .6% GDP per capita $585 $35,991 Roadmap me the world international public health computers me Unit of measurement • Need to quantify population health – measure success – allocate resources • Measure health by counting deaths? Canada Deaths per 1000 per year (2003 est.) 7.61 Mexico 4.97 (answer: Mexicans are younger than Canadians) Life Years Lost • Select a target/ideal length of life. – e.g., 80 years for men, 82 for women • For each death, calculate life years (LY) lost relative to target length. – E.g. death of a 40 year old woman = 82 – 40 = 42 LY lost How many Life Years lost? • Tsunami: deaths X LY per death (my guess) = 300,000 x 65 = 19,500,000 LY lost • Malawi: population X death rate X LY per death = 12,000,000 X .024 X 42 = 12,096,000 LY lost • Sub-Saharan Africa: 650,000,000 X .018 X 34 = 397,800,000 LY lost = 20 tsunami’s worth of LY lost per year DALYs: Disability Adjusted LY • Assign weights to health states: – E.g. “Give 1000 people a year of healthy life or 2000 people a year of paralyzed life?” • Assign weights years – E.g. 25th year worth more than 5th or 65th • Discount future years – E.g. 3% per year cause of lost DALYs 1 Lower respiratory infection 6.4% 2 Perinatal conditions 6.2% 3 HIV/AIDS 6.1% 4 Unipolar depression 4.4% 5 Diarrhoea 4.2% 6 Ischaemic heart 3.8% 7 Cerebrovascular 3.1% 8 Road traffic 2.8% 9 Malaria 2.7% 10 Tuberculosis 2.4% What can we do? Phys/Human Capital Income E.g. being pushed into poverty by medical expenses Demography and Health E.g. hard to learn when ill, or if working because parent is ill. Reducing Child Mortality HIV Prevention Roadmap me the world international public health computers me Information & Communication • Had another revolution in the last 10-15 years: – ease of communication – availability of information – tracking of objects • Many opportunities to address fatal information deficits in healthcare. But... Information Kiosk Less than $5 on her healthcare, annually Information Deficits for Medication • Tele-medicine • Electronic medical records (EMR) • Decision support • Intelligent tutoring • Sensor networks • Data mining and visualization • Connectivity for low-income regions • What’s in stock, expirations • Healthcare workers – medical expertise – patient’s medical history • Population/policy – Needs assessment – What’s working • Individual – When to seek care Tele-health • Addresses information deficits due to – unfortunate distribution of medical expertise – burden of travel • Many options – – – – doctor to patient, never meet doctor to patient, meet occasionally doctor to doctor doctor to data repository (HealthNet) • Technical challenges – sensors for health data – max. use of bandwidth – user interface Electronic Medical Records • Info. management in med. care: – – – – patient history at point-of-service drug inventory, and prediction decision support monitoring and evaluation • Challenges for computerization: – expense – electricity & connectivity – expertise Nurses in India, using EMR by Dimagi and AIIMS. Ca:sh (Community Access to Sustainable Health) • Handhelds for nurses • Targets antenatal care, immunization, disease management • 80,000 records since February 2002 • 25¢ per patient per year • Now using desktops & car batteries in clinics. • By Dimagi, AIIMS • Encode standard protocols to guide health workers • Working on HIV protocols • First target: filter out easy “no change needed” cases • Information periodically uploaded • Led by Marc Mitchell, Hilarie Cranmer Symptoms fever □ RR > 40/50 or chest indrawing □ diarrhea □ abd. pain □ rash □ next Need Research? "The task before us is very urgent, so we must slow down.” Analogy: 10/90 gap in medical research Behavior Change • Information deficits in caretakers of children: – keep children away from smoke – don’t withhold food from children w/ diarrhea – don’t rub dirt into umbilical cord • Possible tools: – interactive tutoring/testing – games, animation – virtual reality Cost Effectiveness • Behavior change system – laptops, PDA, phones, projectors, VR goggles, etc. – operated by one person • Cost – $1000 per year for equipment – $4000 per year operational • Reach – present to 10 people per day – 200 presentations saves a child’s life • Impact lower child mortality – $333 per life – ~$10 per DALY fertility –reduced World Bank says $150 per DALY is bettercost health & wealth effective Passive Surveillance Crisis Mapping • Field personnel register location of – physical resources (e.g., medicine) – activities (NGO’s) – situations (people, disease) • Upload to GIS system to improve – coordination of responders – cooperation between NGO’s “It's such an obvious idea that no one has done it. Go figure.” Related Challenges • Predicting path of fleeing refugees • Population counting for refugee camps Connectivity • Vehicle-mounted hubs (Pentland) • Boosting 802.11b (Brewer, Pentland) – many hardware/power issues – unconventional networking – specialized protocols • DVDs by Postal service (Wang) Parting thoughts the answer • Easy pickings for exciting ideas • Must work with people in field • Funding etc. a challenge • My next years: visit many sites and field-test variety of ideas. Inspiration • “We’re going to be a millionaire of a different sort. We’re going to try to affect the lives of a million people.” - Vikram Kumar, CEO of Dimagi. • The new abolitionist: someone working to eliminate extreme poverty this century. Thanks! To keep in touch, email me at neal@equalarea.com Age distribution Surveillance • Def: ongoing & standardized data collection • Crucial for: – Resource allocation – Evaluation – Outbreak detection • Currently inadequate: – Often rely on studies & models – Push for “evidence-based medicine” Road traffic safety Road traffic injuries expected to move to 3rd leading cause of DALY’s by 2020. Medical Records & Decision Support • Many of the world’s poor: – never see physician – not reached by standard treatment protocols, e.g., case management for diarrhea or measles – have no continuity of care • Computerization improves: – patient info. at point-of-service – decision support, latest protocols – collection of data Life-threatening shortages of... • Human expertise – 2 physicians per 100000 Malawians • Information – recently ‘found’ 250,000,000 cases of malaria • Efficiency – many drugs expire in rural clinics • Coordination/communication – tremendous overlap of activity in humanitarian efforts How and when to introduce technologies? Shortage Human Expertise Example 2 physicians per 100,000 Malawians Tools telemedicine HealthNet decision support intelligent training systems Information recently ‘found’ 250 passive sensing million cases of malaria standardized records pattern detection in health data Efficiency drugs expiring in clinics drug inventory in EMR path prediction of fleeing refugees Comm. & Coord. importance of email better connectivity Phys/Human Capital Income Demography and Health Applied computer science to make new tools for healthcare efforts Leading causes of DALYS Cause %Total DALYS (2002) 1 Lower respiratory infections 2 Perinatal conditions 3 HIV/AIDS 4 Unipolar depressive disorders 5 Diarrhoeal diseases 6 Ischaemic heart disease 7 Cerebrovascular disease 8 Road traffic accidents 9 Malaria 10 Tuberculosis 6.4% 6.2% 6.1% 4.4% 4.2% 3.8% 3.1% 2.8% 2.7% 2.4%