Three page application for the human use of radioactive material-clinical
advertisement

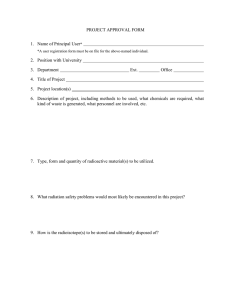
The University of Texas Health Science Center at San Antonio Environmental Health & Safety Department Radiation Safety Division APPLICATION FOR CLINICAL USE OF RADIOACTIVE MATERIAL AUTHORIZED USER Name Department Office Location Office Telephone E-Mail Address Emergency Contact Telephone AUTHORIZED USER QUALIFICATION Texas Medical License Number Board Certified: □ Yes (please attach) □ No (complete Supplement A & B, NRC Training & Experience and Preceptor Statement for each type of procedure) Board Certification Date: CLINICAL PROCEDURE (check all that apply) §289.256 (ff) & (gg)– Diagnostic Nuclear Medicine, Nuclear Cardiology Uptake, Dilution and Excretion Imaging and Localization – bone scans, heart scans, liver scans, etc. Sentinel Node Injections– breast imaging §289.256 (kk) - Unsealed Therapy, includes I-131, Sr-89/Sm-153/Y-90, Y-90 microspheres Unsealed Therapy, general I-131 < 33 mCi I-131 > 33 mCi Parenteral Unsealed Therapy (Sr-89, Sm-153, Y-90) Y-90 microsphere (attach manufacturer proctor training certificate) §289.256 (rr) – Manual Brachytherapy Manual Brachytherapy, includes I-125 permanent & temporary implants, Au-198 prostate implants Sr-90 Opthalmic §289.256 (bbb) – Sealed Sources for Diagnosis Sealed Sources for Diagnosis §289.256 (ddd) – High Dose Rate Brachytherapy Ir-192 High Dose Rate Bracytherapy Revision 6/25/2010 §289.256 – Emerging Technologies Intravascular Brachytherapy Other – Attach a complete description §289.256 – Other Radioactive Materials Radioactive Material Chemical/Physical Form Maximum Activity Type of Procedure PERSONNEL 1. Have the supervised individuals involved been trained for this procedure? □ Yes □ No (If yes, please provide documented training for the radiation safety or for the use of the device) 2. List all personnel who will be involved in the preparation, handling, and administration of radioactive materials. Please include each individual’s training and credentials: RADIATION SAFETY: □ Yes □ No 1. Will body fluids/excreta contain radioactive material? 2. Describe procedures for controlling the spread of radioactive contamination. Take into account the physical form (gas, liquid, solid) and list any specific requirements for controlling the contamination. 3. How will each patient be identified prior to administration or treatment? 4. How will the non-pregnant status of female subjects of childbearing potential be established and documented? 5. Will patients be inpatients or outpatients? □ Inpatients □ Outpatients 6. If inpatients, which nursing unit? 7. Attach copy of radiation safety instructions given to the nursing staff for therapy procedures. 8. Are there special radiation dose reductions required for personnel (ex: syringe shield)? 9. Dosimetry required for faculty/staff? □ Yes □ No 10. Is the facility adequate (lead shields in walls, etc)? □ Yes □ No 11. Describe any special precautions for handling radioactive waste. 12. Attach patient radiation exposure information (MIRD, ICRP, etc). Revision 6/25/2010 I certify that the material requested will be used in accordance with the Radiation Safety Regulations at this institution, with all requirements of the law, and with Regulation of the Texas Department of State Health Services, Bureau of Radiation Control. I certify that all information contained herein, including any supplements attached, is true and correct to the best of my knowledge. Authorized User Signature Date Department Chair Signature Date Revision 6/25/2010