NP and CNS Delegation Protocol BSWNTD
advertisement
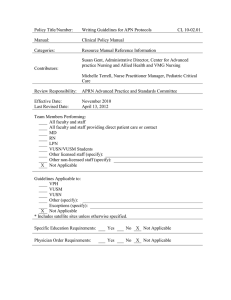
NP and CNS Delegation Protocol Explanation Page ***This page is not be included in your final agreement This template is for facility based APRNs only. For APRNs who are not considered facility based delegation must be thru a Prescriptive Authority Agreement (PAA). Please see the BS&W NTD Prescriptive Authority Agreement for Nurse Practitioners and Clinical Nurse Specialists if appropriate. Facility based APRNs may choose to use a PAA rather than a protocol for delegation but if they do so then all requirements of a PAA must be met. This includes the face to face monthly quality meetings with the delegating physician. For must facility based APRNs it is more appropriate to use this template. Delegation protocols are not to be confused with typical protocols used in the hospital that describe exact steps/care that is to be provided for a specific disease process. Delegation protocols do not need to describe exact steps that APRNs must take and should be written so APRNs may use their education and judgment in order to provide care for patients. This document is a template and should be used as starting point in developing a protocol that reflects the APRN(s)’ practice. All parties to the protocol should participate in the development. The delegating physician(s) must determine what medical acts he/she will delegate. The document should be reviewed, signed and dated at least annually. It may be done more frequently if needed. This template is specifically for nurse practitioners and clinical nurse specialists. CRNAs and midwives have other laws/regulations related to their practice which were not reviewed while constructing this document therefore not included. The material in the document that is italicized and highlighted in yellow is to provide clarification and direction. This material should not be included in the final agreement that will be signed by all participating parties. Please read the document carefully and use the material that is applicable to your practice. For instance there are some sections that have many options to choose from depending on what the delegating physician(s) chooses to delegate. Quality improvement for facility based APRNs is not dictated by law as it is of non-facility based APRNs. The delegating physician(s) is/are held responsible for providing adequate supervision that conforms to what a reasonable, prudent physician would provide. Quality improvement/supervision must meet the requirements of the facility bylaws and/or policies. The protocol must include: -medical aspects delegated by the physician -categories of dangerous drugs and controlled substances an APRN may or may not prescribe (include blood products) -limitations on dosage units and refills -instructions to patients for follow-up -reviewed and signed annually -may include other provisions that are not mandate Other Documents that should be reviewed by all APRNs - Quick facts for APRN Practice in Texas - Physician APRN Facts Other Documents that may or may not apply to your practice: - Consultation Agreement Template - Call Prescriptions on Behalf of APRN Template 0 Baylor Scott & White Health North Texas Division Delegation of Medical Acts and Prescriptive Authority Protocol for Nurse Practitioners and Clinical Nurse Specialists This delegation protocol, herein out referred to as protocol, is for the practice of Advanced Practice Registered Nurses (APRNs). The protocol is applicable to the practice of Nurse Practitioners and Clinical Nurse Specialists who are associated with or employees of The Baylor Scott & White Health North Texas Division Health Care System or applicable partners. Purpose [optional section] This protocol authorizes the APRN(s) to perform medical acts, including prescribing and ordering drugs and medical devices and receiving and distributing drug samples, in accordance with the Nursing Practice Act, §301.152, Texas Occupations Code and the Medical Practice Act, §157.051 – 157.060, Texas Occupations Code. This protocol delegates certain medical acts, as authorized or required by Texas law, and sets forth guidelines for collaboration between the delegating physician(s) and the APRN(s). This protocol is not intended to limit the healthcare services the APRN(s) shall provide under his or her scope of practice, based on the advanced practice role and specialty authorized by the Texas Board of Nursing (BON). Development, Revision, Review and Approval [optional section] The protocol is developed collaboratively by the APRN(s) and delegating physician(s). The protocol must be reviewed annually, dated, and signed by all the parties named in the protocol. Alternate physician(s), if designated, are not required to sign the document. The protocol may be revised more frequently as necessary. With the exception of amending the list of alternate physicians, if designated, amendments must be signed and dated by all parties. Any changes to documents referenced in the protocol, must also be approved by all parties to the agreement. Signing the “Statement of Approval” signifies the parties approve the protocol and all policies, protocols and/or procedures referenced in this document. The parties are entering into a collegial relationship in which each party understands and will fulfill his/her legal responsibilities under the terms of the protocol. APRNs and any delegating physicians who join the staff after approval or renewal of this protocol will also review and sign the protocol. APRNs must sign the protocol before prescribing or ordering any drugs or medical devices. Each APRN and physician must retain a signed copy of the protocol until the second anniversary after the delegating relationship is terminated. Requirements and Disclosures [optional section] The APRN must be licensed in good standing as a Registered Nurse and as an APRN with prescription authorization from the Texas Board of Nursing in a role and population focus area appropriate to the population of patients for whom the APRN will prescribe or order drugs and medical devices. APRNs shall not be a party to a protocol if under a Board Order prohibiting their participation. If prescriptive authority for controlled substances is delegated, the APRN must also have a Texas Department of Public Safety Controlled Substances Permit and a Drug Enforcement Agency (DEA) certificate. The APRN must also possess a valid Basic Life Support (BLS) and Advance Life Support Certificate (ACLS) in accordance with facility or practice policies in which they practice. Each delegating physician must hold a full and unencumbered Medical License issued by the Texas Medical Board. The physician is not limited in the number of Advanced Practice Professionals may delegate to at one facility but is limited to delegating at only one facility under the facility-based practice provision. This does not exclude the physician from also delegating thru a Prescriptive Authority Agreement under the non-facility 1 provision, which is limited to delegating to a total of no more than the full-time equivalent (1 FTE = 50 hours) of seven APRNs and physician assistants. Before executing this agreement, the physician and APRN must disclose to all other prospective parties any prior disciplinary action taken by the respective licensing board. Within 30 days of executing this agreement, the physician and APRN must complete the Texas Medical Board’s “Prescriptive Delegation Registration.” Any party to this agreement will notify the other parties immediately if, at any time while this protocol is in effect, a licensing board notifies the person he/she is under investigation. Nature of the Practice and Locations [optional section] The APRNs will treat [insert the type of practice and population of patients to be cared for by APRN, ex: adult and gerontological patients admitted to the xx service, patients of all ages in a facility based hospital emergency room] at the following practice site: Include facility name, complete address Name, Address and Professional License Numbers of Parties to the PAA [optional section] [Add as many rows to table as necessary, may include this information on signature page rather than place here. APRNs must list TX DPS and DEA numbers if physician is delegating prescriptive authority for controlled substances.] _____________________________________________________ Delegating Physician’s Name and Professional Title _____________________________________________________ Address _____________________________________________________ Delegating Physician’s Name and Professional Title _____________________________________________________ Address _____________________________________________________ APRN’s Name and Professional Titles _____________________________________________________ Address _____________________________________________________ APRN’s Name and Professional Titles _____________________________________________________ Address _____________ TMB License # _____________ TX DPS # _________________________ City _____________ TMB License # _________ State _____________ TX DPS # _________________________ City _________ State _____________ RN License # _____________ APRN License # _____________ TX DPS # _____________ DEA # _________________________ City _________ State _____________ RN License # _____________ APRN License # _____________ TX DPS # _____________ DEA # _________________________ City _________ State _____________ DEA # _________________ Zip Code _____________ DEA # _________________ Zip Code _____________ Rx Auth # _________________ Zip Code _____________ Rx Auth # _________________ Zip Code Delegation of Prescriptive Authority and Medical Acts [This section should be modified in accordance with medical acts being delegated] The APRN may establish medical diagnoses for patients who are within the APRN’s scope(s) of practice, and order or prescribe drugs. The APRN may order/prescribe medical devices, including medical supplies, durable medical equipment, prosthetics or orthotics as authorized by the Texas Board of Nursing and the Texas Medical Board rules and regulations. The APRN may also receive and distribute samples for drugs they are permitted to prescribe. These services/functions are not an exhaustive description of the APRN practice but rather illustrative of the types of medical aspects of care the APRN will perform. The APRN may perform medical 2 functions and procedures as privileged by the facility in which the APRN provides care. These functions include, but are not limited to, performing physical examinations and medical histories, ordering and interpreting laboratory tests and radiologic exams, providing health promotion and safety instructions, evaluation and management of acute episodic illnesses and stable chronic diseases, and referrals to other health care providers, as needed. A. Prescriptive Authority The APRN(s) may order or prescribe: [The law states that physicians may delegate ordering and prescribing nonprescription drugs but there is no requirement to further specify categories of these drugs. The PAA, however, must specify the drugs or categories of Dangerous drugs that may or may not be ordered or prescribed. If no limitations, specify that all categories of dangerous drugs are included, or if there are limitation, specify those limitations. Other options might include drugs that may or may not be generically substituted and the number of refills the APRN may prescribe. No limitations are required by law. The legal definition of “dangerous drugs” includes medical devices. Therefore, if there are any limitations of prescribing medical devices, also note that in this section and modify other suggested language, as necessary.] 1. Nonprescription and Dangerous Drugs (The term includes a device or a drug that bears or is required to bear the legend: "Caution: federal law prohibits dispensing without prescription" or "RX only" or another legend that complies with federal law) A [choose one statement] The APRN(s) may order and prescribe all categories of nonprescription drugs and dangerous drugs that are within the APRN’s scope of practice without limitations on dosage units or refills other than those listed elsewhere in this protocol. The APRN(s) may order and prescribe all categories nonprescription drugs and of dangerous drugs that are within the APRN’s scope of practice without limitation on dosage units or refills, except those listed elsewhere in this protocol and for the following: B When prescribing dangerous drugs, generic substitution for all drugs is permitted. C The APRN may prescribe investigational drugs as part of a research protocol as directed by his or her supervising physician D BON Rule 222.4 (e) limits the drugs APRNs may prescribe to those that are FDA approved unless part of a research protocol or the APRN can show evidence-based research that prescribing the drug is within the standard of care for the disease or condition being treated. 2. Controlled Substances, Schedules III - V [these limitations are required by law. May specify any other limitations the delegating physician places] A Limited to a 90-day supply or less B No new prescriptions or refills after the initial 90-day supply without prior consultation with the physician. C No prescription for children under 2 years of age without prior consultation with the physician. D Prior consultation must be noted in the patient’s record. E In accordance with §481.071, Health & Safety Code, an APRN may not prescribe an anabolic steroid or human growth hormone listed in Schedule III. 3. Controlled Substances, Schedule II APRNs may order and prescribe the following categories of Schedule II Controlled Substances for [choose applicable statement (s): hospice patients in any setting, patients in the hospital emergency room, and/or hospitalized inpatients with an intended length of stay greater than 24 hours]: 3 [examples below, change as appropriate] Opiates to manage pain Stimulants to manage fatigue Depressants to manage sleep disturbances 4. The APRN may prescribe all blood products as applicable for patient care. B. Drug Samples [optional section, however includes information that is difficult to obtain and the BON requires APRNs to maintain this documentation] The APRN(s) may accept, sign for and distribute prescription drug samples. The APRN(s) must retain any receipt they sign when receiving drug samples. In addition, the APRN must note in the patient’s chart any sample distributed and comply with Baylor Scott & White Health North Texas Division facility policy on the documentation and/or distribution of drug samples. The date, drug, dosage, frequency and duration of treatment must be noted in the patient’s chart and included on the sample distributed to the patient. The APRN may also wish to maintain a record of distribution that includes the date of distribution, the patient’s name, the name and strength of the drug, the lot number, and/or directions for use. C. Persons Who May Call Prescription to the Pharmacy as Directed by the APRN [optional section] The physician designates any licensed vocational nurse or registered nurse working or volunteering in this site as a person who may orally transmit a prescription into a pharmacy on behalf of the APRN(s). A list of the person authorized to orally communicate prescriptions to the pharmacy must be maintained at the practice site and will be made available to a pharmacist upon request. [Any such person(s) should be designated by name and can be listed here or elsewhere] D. Medical Procedures [optional section][this section is to identify medical procedures the APRN may perform that would not be within the APRN’s normal scope of practice. It should not include procedures that all RNs can perform and those commonly performed by this type of APRN. List procedures that require training beyond that usually taught in most educational programs for the APRN’s role and population focus. However if want to include it is acceptable to list procedures that are standard for APRNs practicing on a particular service or may refer to job description or privileging documents]. The APRN may perform medical procedures in accordance with their education and training as specified on facility privileging documents. E. Medical Verifications for Disabled Parking Placards [optional section, no need to include if this does not apply to the APRN’s practice. However delegation is required so if it is not included then the APRN is unable to sign verification for initial application of disabled parking placard] The APRN may sign a prescription or notarized statement for patients that meet the legal requirements for a temporary disabled parking placard. The APRN is limited to signing verifications that will accompany the initial application for patients. Subsequent renewals for temporary parking placards must be signed by the physician. Qualifying conditions: 1. Persons with a mobility problem that substantially impairs the ability to ambulate including: a. cannot walk 200 feet without stopping to rest b. cannot walk without the use of or assistance from an assistance device, including a brace, cane, a crutch, another person, or a prosthetic device c. cannot ambulate without a wheelchair or similar device 4 d. is restricted by lung disease to the extent that the person’s forced respiratory expiratory volume for one second, measured by spirometry, is less than one liter, or the aterial oxygen tension is less than 60 millimeters of mercury on room air at rest e. uses portable oxygen f. has a cardiac condition to the extent that the person’s functional limitations are classified in severity as class III or class IV according to standards set by the American Heart Association g. is severely limited in the ability to walk because of an arthritic, neurological or orthopedic condition 2) Persons with visual disabilities including: a. visual acuity of 20/200 or less in the better eye with correcting lenses b. a limited field of vision in which the widest diameter of the visual field subtends an angle of 20 degrees or less. F. Authorizing and Ordering Certain Services Reimbursed by the Texas Medicare Program, CHIP or Early Childhood Intervention (ECI) Programs. [Optional section, only include if applicable to your practice. The APRN would normally be able to order these services for patients of any age as part of their independent scope of practice. However, a Texas Medicare Rule states APRNs may order the services if the physician delegates that authority]. The APRN may determine medical necessity and sign any documentation related to providing the following services to persons insured by Texas Medicaid, CHIP or ECI who are age 20 years or younger: 1. 2. 3. 4. Private Duty Nursing Physical therapy Occupation therapy Speech therapy Instructions to Patients for Follow-up For patients the APRN discharges the APRN will provide instructions to patient regarding appropriate follow-up in accordance with patient condition and per hospital policy. Follow-up should be congruent to what a reasonable and prudent APRN would recommend. General Plan for Consultation and Referral: [optional section] [Law requires that the PAA include a “general plan for addressing consultation and referral.” There may be legal implications, so nothing specific should be included that does not always trigger consultation or referral. Goal of this is to clarify the relationship between the APRN and physician and avoid miscommunications. The APRN and physician should discuss and identify any situations in which consultation is expected. The delegating physician(s) (or designated physician(s)) are available for consultation at any time. However, the APRN may seek consultation and refer patients directly to the most appropriate health care provider to treat the patient’s condition when, in the APRN’s judgment, such steps are necessary for optimal resolution of the patient’s problem. Whenever a physician is consulted or patient referred, a notation to that effect, should be recorded in the patient’s medical record. Consultations and referrals may also be discussed at quality assurance and improvement meetings. Plan for Patient Emergencies [optional section] [this is an example of what might be included in the PAA. The plan should be specific to the type of patients in the practice and more detail may be added. The bracketed statements below are examples of reporting requirement that could be included. Additional detail might include any level of CPR certification the APRN is required to maintain and/or emergency drugs and medical devices required to be maintained on site]. 5 If the APRN determines that the immediate health and wellbeing of the patient is at risk, the APRN must take immediate steps to stabilize the patient while having a staff member initiate emergency protocols. This may include but is not limited to calling 911 for response by emergency medical services and transport to an emergency room or calling appropriate hospital code for response of emergency medical services. [As soon as possible, the APRN is to report any emergency situation of this nature to the delegating physician]. For emergencies that require immediate treatment, but the life of the patient is not in immediate danger, the APRN must take steps to assure the patient’s safety and comfort. If the patient’s condition is beyond the usual type of conditions treated by the APRN, h/she immediately consults the authorizing or alternate physician, or a physician specialist, as most appropriate. [If the authorizing physician was not notified, the APRN reports the emergency to the authorizing physician as soon as possible]. In case of an emergency in which serious permanent harm or aggravation of injury or disease is imminent, or in which the life of patient is in immediate danger, the APRN may provide care to stabilize a patient’s condition and/or prevent deterioration of a patient’s condition, to the degree authorized by the APRN’s licensure, registration or certification. This includes providing care to patients outside the type of practice and population listed in this protocol until another a physician or other appropriate profession is available. General Communication Process Concerning Patient Care and Treatment [optional section] The delegating physician will be available by telephone or email [add any other type of communication commonly used in this practice such as telemedicine or videoconferencing.] If discussions reveal the patient’s identity, HIPPA complaint forms of communication will be used. Daily communication between the APRN and the delegating physician is not required, but the physician will be available to discuss patient care and treatment upon the request of the APRN. At a minimum, at the quality assurance and improvement meetings specified below, the APRN and authorizing physician or if designated, an alternate physician will discuss patient care and treatment plans for patients with complex problems, or problems the APRN does not have experience treating. The physician or APRN will have additional meetings, when either party thinks patient care would benefit from more frequent communication and requests additional time to discuss patient care and treatment. Quality Assurance and Improvement (QAI) Plan [optional section] Evaluation of the APRN(s) will be provided in the following ways [below are examples only, change as related to your practice, in congruence with facility policy and procedure, and preference of delegating physician]: Informal evaluation during consultations and case review Weekly rounds Monthly department meetings, QI meetings Chart reviews Annual evaluation per hospital policy/procedure Medical Records [optional section] The APRN(s) is/are responsible for the complete, legible documentation of all patient encounters in a manner consistent with Baylor Scott & White North Texas Division facility policy as well as state and federal laws. Alternate Physicians [optional section] If the delegating physician is unavailable for any reason, alternate physician(s) may assume the consultation, supervisory and quality assurance and improvement responsibilities of the authorizing physician. The authorizing physician may amend this list by written notice to all parties. The following may serve as alternate physicians: [list the physicians and their contact information] 6 References Woolbert, L. (2013). Prescriptive authority agreement sample. Austin, TX: Coalition for Nurses in Advanced Practice. Texas Administrative Code, Title 22, Part 9. Texas Medical Board, Board Rule. Chapter 193. Standing Delegation Orders §193.1-193.20 Texas Administrative Code, Title 22, Part 11. Texas Board of Nursing Advanced Practice Nurses. Chapter 221. Definitions. §221.1. §221.2, §221.8, §221.11, §221.12, §221.13 Texas Administrative Code, Title 22, Part 11. Texas Board of Nursing Advanced Practice Nurse. Chapter 222. Prescriptive Authority. §222.1-§222.10 Woolbert, L. F., & Ziegler, B. (2013). A guide for APRN practice in Texas (4th ed.). Austin, TX: Coalition for Nurses in Advanced Practice and Texas Nurse Practitioners. 7 Delegation of Medical Acts & Prescriptive Authority Protocol Signature Page for [insert current year] I, one of the undersigned, affirm I reviewed and agree to the term of this Delegation Protocol. I agree to fulfill the responsibilities set forth in the document. I declare that I meet the requirements to be a party to this agreement and have disclosed any prior disciplinary actions taken by my licensing board. I will inform other parties to the agreement if I am notified my licensing board is investigating my practice while this protocol is in effect. _______________________________________________________ Authorizing Physician’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ Authorizing Physician’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date _______________________________________________________ APRN’s Signature __________________ Approval Date 8 Form #1: Record of Alternate Physician Supervision for Delegated Prescriptive Authority APRN’s Name ____________________________ License #_________ Rx# ________ Delegating Physician’s Name__________________________ License #__________ Dates of Supervision by an Alternate Physician Begin End Signature of Alternate Physician License # ___/___/___ ___/___/____ ________________________________________ __________ ___/___/___ ___/___/____ _________________________________________ _________ ___/___/___ ___/___/____ _________________________________________ _________ ___/___/___ ___/___/____ _________________________________________ _________ ___/___/___ ___/___/____ _________________________________________ _________ ___/___/___ ___/___/____ _________________________________________ _________ ___/___/___ ___/___/____ _________________________________________ _________ ___/___/___ ___/___/____ _________________________________________ _________ ___/___/___ ___/___/____ __________________________________________ _________ ___/___/___ ___/___/____ __________________________________________ _________ ___/___/___ ___/___/____ __________________________________________ _________ By signing this log sheet, I affirm that I served as the alternate physician for the purposes of supervising prescriptive authority of this APRN for the dates specified. I acknowledge my responsibility to consult with and perform quality assurance and improvement activities with this advanced practice registered nurse pursuant to the Delegation Protocol. 9 Form #2: Record of Chart review or Other QAI Activity Date Patient Name or Chart Number Chart Reviewed Consult ____/____/____ _________________________________________ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ___/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ ____/____/____ _________________________________________ □ □ □ □ □ Date of QAI Meeting: ____/____/____ Physician Signature APRN Signature Patient Referred □ Case Presented □ TX Plan Revised □ Beginning Time: _________ End Time: ________ Printed Name: Printed Name: 10 Form #3: Distribution Record for Drug Samples Date Distributed Patient’s Name Drug Lot # Strength Directions for Use Distributing Practitioner 11 Form #4: Record of Delegation of Prescriptive Authority and PAA Review APRN’s Name Name & Address of Practice Locations/s (if different than physician’s) Type of APRN Delegating Physician: ____________________________ Practice Designation/s Dates of Delegation Initiated: RN License # APRN License # Terminated: APRN Rx # DEA # DPS # Dates of PAA Approval/Review APRN’s Name Name & Address of Practice Locations/s (if different than physician’s) Type of APRN Practice Designation/s Dates of Delegation Initiated: RN License # APRN License # Terminated: APRN Rx # DEA # DPS # Dates of PAA Approval/Review 12 13