Partnering with a Medicare Advantage Plan to Enhance Value Added Patient and Family Centered Care Delivery
advertisement

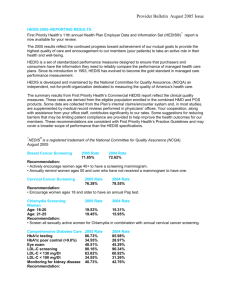
#63 PROJECT NAME: Partnering with a Medicare Advantage Plan to Enhance Value Added Patient and Family Centered Care Delivery Institution: UT Health Northeast Primary Author: Brenda Lee, MSN, RN Secondary Author: Dr. Jonathan MacClements Project Category: Medical Homes/Reform Purpose: Health Plans and Federal programs are progressively requiring evidence of quality performance with reimbursement tied to that evidence. The Triple Aim for the future of health care encompasses; improved health, improved care, and lower cost. “Integrators” of health will be the organizations which will move healthcare in the direction of this destination.”1 Three integrators are: Medicare Advantage, Medical Home, and Accountable Care Organizations. All three of these programs have a defined set of quality measures which are required in order to participate and in order to receive the maximum reimbursement. There is significant overlap to these requirements as evidenced in comparison of the measurement groups – HEDIS, Meaningful Use, PCMH, NQF, PQRS, etc. As our organization re-engineered for Patient Centered Medical Home designation, partnering with the Medicare Advantage (MA) plan representing our largest number of beneficiaries became a strategic tactic. Centers for Medicare and Medicaid (CMS) posts quality ratings of MA plans to provide beneficiaries with additional plan information. All MA plans are rated on a 1 to 5 star scale, with 1 star representing poor performance, 3 stars average, and 5 stars excellent. In 2012, MA plans began to receive bonus payments based on quality ratings. “The plans receiving bonus payments are required to use the additional dollars to provide “extra benefits” (such as eye glasses or transportation to and from the doctor) for the plans’ enrollees. “Therefore plans with higher quality ratings should be able to provide a more attractive set of benefits than their competitors, which in turn may lead to higher enrollment in plans with higher quality ratings.” 2 The bonus payments may affect market share if beneficiaries begin to shift to plans with higher ratings. “Medicare is accelerating plans to peg a portion of doctors’ pay to the quality of their care.”3 The federal health law requires large physician groups to start getting bonuses or penalties based on their performance by 2015 with all physicians treating Medicare patients by 2017. Groups are at risk for 1% of their pay in 2015, doubled to 2% in 2016 year under draft regulations. The bonuses and penalties would be calculated on their patients cost on average as well as the quality of care provided. Because the provider-performance-dependent metrics are HEDIS measures, the MA Star program metrics should have been readily accessible by our organization. However, HEDIS results were not being reported in a consistent, structured manner. We believe particular focus on the star rated subset of HEDIS measures will assist us in discerning where performance falls short and to implement improvement strategies. 2013 Deadlines for 4 Star Rates June 30 Diabetes Kidney Testing Diabetes A1c Testing Diabetes LDL Testing Diabetes Eye Exam Cardio LDL Testing September 30 BMI Assessment Glaucoma Testing SNP Med Review SNP Pain Screening SNP Functional Status October 31 Breast Cancer Screen Colorectal Cancer Screen Rheumatoid Arthritis Osteoporosis Management Aim: Achieve a 4 STAR rating on all CMS Medicare Advantage clinical measures by January 1, 2014. The key stakeholders are HealthSpring Key Council members. Our patients are to be considered stakeholders as this initiative meets the triple aim for improved population health, the right cost, and of high quality. Tools and Measurement: The table below was provided by HealthSpring in March, 3013. This would serve as baseline data and assist with targeting 5 of 13 HEDIS measures. All outstanding metrics would be eligible for a $100 incentive bonus if completed by June 30, 2013. The Diabetes related indicators would need to be completed by June 30, 2013 per the plan established deadline (table 1 above). After the June deadline, all metrics would be reduced to a $50 incentive bonus. HEALTHSPRING MEDICARE ADVANTAGE STAR PROGRAM LSS REPORTS MEDICARE ADVANTAGE PLAN Not receiving incentive $$ Inaccurate Low patient risk scores No process for completion of elements Missing Codes Not capturing all Dx codes Lack of education regarding plan elements Coding not reviewing clinic notes No ZYNX Upgrades Missing connection between contracting & clinical Physician Codes incomplete Over-Customized Build Clinical not involved in Contract negotiation Misunderstood consequences of customization Knowledge & time Missing labs results No reminders / alerts < 4 STAR RATING FOR HEALTHSPRING CLINICAL MEASURES No LOINC codes loaded Not built/activated/accurate Upgrade not taken Unaware of requirement timeline Misunderstood requirements Inexhaustible external & internal demands No priority plan LSS HEALTH MAINTENANCE HEDIS DATA A cause and effect diagram was used to identify root causes for not achieving a 4 or 5 star rating on HEDIS measures. Highlighted components were determined to be priority items for action planning. Non-highlighted items are related to EMR functional capability. The EMR Leadership team would be apprised and delegate(s) included on the HealthSpring Key Council. A current state value stream map was created which demonstrated the need for a future state value stream map which would enhance reliability of accomplishing whole person delivery of care. CURRENT STATE VALUE STREAM MAP Transfer to Scheduling Call main number for appointment ing erform RN p s vs. task ing teach Patient to Exam Room Registration Check In Clerk Delay Fills out history Insurance Verified Co-payment Exam Room RN/MA Assessment Delay Paged to booth Time for patient education/ teaching Checkout Provider Delay Checkout Clerk Delay Vitals taken Referral info Patient Assessment Verified meds Prescription info Treatment Question on any problems Discussion (Meds, etc.) Undress and gown No health maintenance alerts in EMR Next appointment scheduling Intervention and Improvement: 1) The organization began to partner with HealthSpring, a Medicare Advantage plan, to educate staff and physicians regarding the Star Rating Program. An in-service was provided to physicians, nursing and the entire coding department. A Key Council; comprised of UT Tyler PCP’s, HealthSpring representatives, senior leadership, one specialist, managed care contractor, and quality department was established. The council meeting is scheduled to meet ten times per year. The focus of the council meetings is to review the plan financial report and discuss specific requirements and barriers to implementation. There is on-going dialogue with HealthSpring clarify questions/concerns regarding reports. 2) We changed the hand delivery of “hot reports” by the HealthSpring representative from the contracting office to the Quality Department. The ‘hot reports” detail missing HEDIS measures. In addition to “hot reports”, a patient missing a Health Management Report (HMR) was included. The HMR is intended to support physicians in the management of their patients by alerting them to pertinent conditions diagnosed during the past two years. This prevented the information from literally being thrown away by providers or staff because they did not understand the value. 3) EMR issues were discussed with the Co-Chief Information officer and at a HealthSpring on-site meeting with laboratory representatives present. Missing LOINC codes were contributing to 1 (one) STAR HEDIS compliance. Iatric was contracted with to build LOINC code reporting for HealthSpring patients as an interim solution, pending an upgrade to the laboratory reporting system. 4) Health Maintenance issues identified; Glaucoma testing and Colon screening missing elements, lack of reminders or alerts, inaccurate reports, and not all HEDIS measures in active. These issues were addressed with the EMR Leadership committee. Corrective actions began in July and are to be completed by December 31, 2013. Thus, a manual process for capturing HEDIS and HMR requirements was implemented 5) The future state Value Stream Map was constructed. FUTURE STATE VALUE STREAM MAP Transfer to Scheduling Inaccurate reports Pre-Visit Patient to Exam Room Check In Clerk Delay Planning for upcoming visit: ft in not le EMR room exam Registration MA Delay Exam Room MA Delay Exam Room Provider Delay Paged to booth Fills out history Verified meds Insurance Verified Co-payment Question on any problems Patient Assessment Treatment Discussion (Meds, etc.) Education Self Management Support Managing Group Visits No health maintenance alerts in EMR Group visit process to be designed Between Visits Checkout Clerk Delay Undress and gown Protocols to be developed Checkout RN Delay Patient EMR opened on computer Vitals taken 1. Health Maintenance outstanding 2. Protocol ordering of “needed” care management Call main number for appointment Patient Delay Referral info Entry of Clinical Care labs/results Prescription info Next appointment scheduling Portal access for medications Management of disease Intervention Results: Breast Cancer Screening (HEDIS) **Colorectal Cancer Screening (HEDIS) **Cardio Care - LDL Screen (HEDIS) **Comprehensive Diabetes Care - LDL Screen (HEDIS) Glaucoma Testing (HEDIS) **Adult BMI Assessment (HEDIS) Osteoporosis Fracture Management (HEDIS) **Comprehensive Diabetes Care - Eye Exam (HEDIS) **Comprehensive Diabetes Care - Kidney Disease (HEDIS) **Comprehensive Diabetes Care (HBA1C < 9 (HEDIS) **Comprehensive Diabetes Care - LDL < 100mg/DL (HEDIS) Rheumatoid Arthritis Management (HEDIS) Plan all Cause Readmissions (HEDIS) 4 Star Rating Threshold 5 Star Rating Threshold Previous Rate Current Rate 74% 58% 85% 85% 70% 61% 60% 64% 83% 67% 91% 90% 78% 80% 67% 81% 50% 60% 100% 92% 86% 80% NA 62% 67% 55% 89% 100% 85% 85% NA 52% 85% 80% 90% 88% 92% 0% 86% 90% 53% 78% 11% 66% 86% 3% 0% 0% 0% 60% NA 28% 1) Key Council and ongoing dialogue has heightened awareness regarding the need to change our patient flow and related EMR functioning. Errors in both HealthSpring and internal reports are of high priority to resolve. Star Rating reports from HeatlhSpring do not match with internal manual audit metric scores. HealthSpring is addressing reliability of their reports. It is therefore, not realistic at this point in the project to determine if our aim has been met. 2) The HMR is a CMS driven manual paper process. Coding is aware of the low patient coding assigned risk score. HealthSpring’s coding representative will provide education regarding the HMR by end of August, 2013. Each coder assigned to a particular physician will then review the prepopulated HMR for accuracy. Deadline for all HMR review is December, 2013. 3) The Iatric HealthSpring interim report does not appear to be accurate in the July, 2013 report. A manual audit of “hot reports” demonstrated 85% - 90% compliance with HGA1c (diabetics) and LDL (cardio & diabetics) being obtained and in control. Manual audit will continue until the lab computer update in October, 2013, is completed. 4) Nurse Managers are actively involved in obtaining missing HEDIS measures and annual HMR’s. Going forward, all HealthSpring patients will be scheduled for visits in the first 90 days. The pre-visit work will accomplish as many of the HEDIS measures prior to the HMR office visit. Pre-authorization required items will be scheduled in advance of the HMR visit as pertinent. Coordination of measures will be accomplished by the RN/MA and scheduling. Protocols will allow for automatic ordering of HEDIS required measures during the pre-visit review. EMR decision support based alerts/needed items will be based on patient condition(s). 5) The future state Value Stream Map aligns with the Family Medicine Clinics’ PCMH model. The Internal Medicine Clinic began working toward PCMH in July. Observation will be performed on the new value stream map to further eliminate non-value steps and reduce waste. A3 methodology will then be utilized to address “red storm clouds” on the map. The most value added time to this new model depends on the patient time spent working toward their health. Revenue Enhancement /Cost Avoidance / Generalizability: HEALTHSPRING MEDICARE ADVANTAGE POTENTIAL REVENUE INCENTIVE PROGRAM HMR Physician MacClements Menard Davis Belt Karaki Holm Bosworth Powell Olusola Andrews Tompkins Shafer Total Eligible Patients 1st Qtr 16 7 26 30 67 22 14 15 7 32 19 32 287 3200.00 1400.00 5200.00 6000.00 13400.00 4400.00 2800.00 3000.00 1400.00 6400.00 3800.00 6400.00 57400.00 1st Qtr. Potential Revenue: 2nd Qtr. Potential Revienue: 3rd Qtr. Potential Revenue: 4th Qtr. Potential Revenue 2nd Qtr HEDIS MEASURES 3rd/4th Qtr 1600.00 1600.00 700.00 700.00 2600.00 2600.00 3000.00 3000.00 6700.00 6700.00 2200.00 2200.00 1400.00 1400.00 1500.00 1500.00 700.00 700.00 3200.00 3200.00 1900.00 1900.00 3200.00 3200.00 28700.00 28700.00 $64,500.00 $35,800.00 $32,250.00 $32,250.00 Eligible 3rd/4th 1st Qtr 2nd Qtr Patients Qtr 5 2 9 5 16 4 6 2 2 8 4 8 71 500.00 500.00 250.00 200.00 200.00 100.00 900.00 900.00 450.00 500.00 500.00 250.00 1600.00 1600.00 800.00 400.00 400.00 200.00 600.00 600.00 300.00 200.00 200.00 100.00 200.00 200.00 100.00 800.00 800.00 400.00 400.00 400.00 200.00 800.00 800.00 400.00 7100.00 7100.00 3550.00 AMT. RECEIVED Received Number Through Completed June 30 5 500.00 1 100.00 5 500.00 3 300.00 8 800.00 1 100.00 3 300.00 0 0.00 1 100.00 0 0.00 4 400.00 2 200.00 33 3300.00 Potential ROI $64,500 vs. Actual ROI $3,300 to date Lessons learned from this project are related to patient’s willingness to accomplish the requirements. This finding supports the future state value stream map of planned, coordinated pre-visits to accomplish as many items with the least amount of face time. As our Medicare Advantage patient base increases, the potential for lost revenue will increase. The loss of revenue may be tied to CMS revenue in the form of value based purchasing. Going forward, it will be essential to monitor whether quality ratings and bonus payments are associated with better care and improved health outcomes for MA enrollees. This project is applicable to all providers contracting with Medicare patients. REFERENCES 1. STARs Tutorial: Medicare Advantage Plan Star Ratings and Bonus Payments in 2012, A tutorial for utilizing SETMA’s Deployment of the STARS MA Program. 2. Jacobson G, Neuman T, Damico A, Huang J. Medicare Advantage Plan Star Ratings and Bonus Payments in 2012. November 2011 3. Rau J. Medicare Announces Plans to Accelerate Linking Doctor Pay to Quality. Kaiser Health News, July 20.