Reducing Ventilator Days in the Medical Intensive Care Unit
advertisement

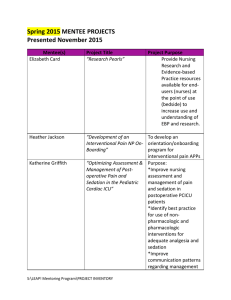
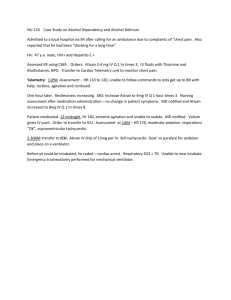
Clinical Safety & Effectiveness Decreasing Ventilator Days in the Medical Intensive Care Unit Department of Critical Care Medicine Prolonged Mechanical Ventilation A glimpse at the future… Zilberberg et al. Crit Care Med 2008. 36(5): 1451-1455 Projected Annual Hospitalization Days in 10-year Increments Spent by a Patient on Prolonged Acute Mechanical Ventilation (PAMV) in Various Strata of Hospital Care. ICU is intensive care unit. MV is mechanical ventilation. Y is year. Zilberberg et al. BMC Health Services Research 2008, 8:242 Prolonged Mechanical Ventilation in the United States On any given day, 7000 to 11,000 PMV patients… 300,000 patients per year Annual costs exceed 20 billion dollars $ Prolonged Mechanical Ventilation Ventilator Associated Pneumonia Deconditioning Airway Trauma Increased Mortality Aim statement “To decrease ventilator days in Medical Intensive Care Unit patients by 10%, by June 30th, 2011” Our baseline = 6.62 days/patient Brainstorming Involve everyone involved: Nurses, Nursing Leadership, Respiratory Therapists, Physicians, Mid-level providers, Pharmacists Ask the question: How can we work together to get patients off the ventilator sooner? Find the root cause: What are the barriers to achieving this goal? Ishikawa(Fishbone)Diagram Flow Chart of Weaning Process Sedation Holidays & Spontaneous Breathing Trials What is the evidence? •Nurse and RT driven •Significant decrease in: •Ventilator free days •Hospital length of stay “daily interruption of sedatives can reduce the duration of mechanical ventilation without compromising patient comfort or safety” •ICU length of stay (from 12.9 days to 9.1 days) •1 year mortality (from 58% to 44%) p=0.02 p=0.01 Our Current Sedation Protocol Baseline Data How were we doing in our Intensive Care Unit? Average Ventilator Days in the Medical Intensive Care Unit at the MD Anderson Cancer Center before our intervention… 6.62 days per patient Average Actual Performance for Sedation & Analgesia Holiday Pre-Intervention 100 90 80 Percent 70 60 50 40 36 30 30 20 10 0 Sedation Holiday Performed Analgesia Holiday Performed Process Map Baseline Average Richmond Agitation Sedation Scale (RASS) for intubated MICU patients between 7pm and 7 am +4 +3 +2 +1 0 -1 -2 -3 -4 -5 Combative Very Agitated Agitated Restless Alert and Calm Drowsy Light Sedation Moderate Sedation Deep Sedation Unarousable Target -3.5 (Our Average) Our Interventions starting February/March 2011 SBT & Sedation Holiday Educational Meetings “A Collaboration at Bedside” Mandatory for ICU RN’s & Therapists (days and nights) • When: 2/21 through 2/25 • Time: 7:00 AM (15mins) • Location: ICU Classroom Presented by: Dr. Rathi Refreshments will be served Improve Nursing Compliance with Automatic Sedation-Analgesia Holiday Protocols Measure of success: Automated individualized compliance reports through PICIS Pair Spontaneous Breathing Trials with Sedation-Analgesia Holidays RT-MD Rounds 8:30 am Improvement In RASS scores at night to an average goal of 0 to -2 30 minute goal to decision to extubate after SBT Communicate Individual MD rates of deferred extubation Improve Nursing and RT communication of SBT readiness Keeping the Momentum Going… Bedside quizzes with prizes Raffles Inservices (RT and RN) Emails/staff meetings WAKE UP and BREATHE Have you done your sedation/analgesia holiday today? How are we doing? Post Intervention Data Actual Performance for Sedation Holidays Sedation Holiday Performed Linear (Sedation Holiday Performed) 100 90 80 70 Intervention Percent 60 58 55 50 46 45 40 42 39 31 30 31 30 30 40 44 42 45 44 29 26 23 20 10 0 Jan Feb Mar Apr May Jun Jul 2010 Aug Sept Oct Nov Dec Jan Feb Mar Apr 2011 May June p = 0.116 Actual Performance for Analgesia Holidays Analgesic Holiday Performed Linear (Analgesic Holiday Performed) 100 90 80 Intervention 70 65 Percent 60 50 50 40 40 30 46 42 40 30 29 52 52 48 38 32 28 28 28 21 20 16 10 0 Jan Feb Mar Apr May Jun Jul 2010 Aug Sept Oct Nov Dec Jan Feb Mar Apr 2011 May June p = 0 .117 Improvement in RASS (sedation score) at night post-intervention +4 +3 +2 +1 0 -1 -2 -3 -4 -5 Combative Very Agitated Agitated Target Restless Alert and Calm Drowsy Light Sedation -1.2 Moderate Sedation Deep Sedation Unarousable -3.5 Baseline Average post intervention Respiratory Data Post-intervention DB I DC HC EG EH EM EN J ER K Provider Average Round Time March - June 2011 I, 9:38 ER 9:00 HC 8.4 EG 8:44 J 8:44 EM 8:37 DC 8.26 EH 8:25 DB 8:18 EN, 8:22 K 8:48 To Sleepy Thick Secretion Heme No Extubation Dialysis Today Apnea Unable to follow Commands tachycardia Getting Trach Anxiety/Precid ex Language Barrier Low MV Problem Waiting for PT Need Scan Tachycardia Poor Mechanics Too weak Questional Mental Status Intervention Baseline = 6.62 days/pt; Post intervention Average = 5.84 days/pt Ventilator Days Decreased by 0.78 or 12% Intervention Baseline = 9.46 days/pt; Post intervention Average = 8.22/pt MICU LOS Decreased by 1.24 days or 13% ACTUAL Return on Investment Costs of Project: Payroll + materials = $18,062.50 $$ ICU Costs: Cost of ICU/Day = $3872.00 Respiratory Costs/Day= $3133.00 Decrease in Average ICU LOS for ventilated patients since March 1st, 2011 = 1.24 days (13 % decrease) Decrease in Average ventilator days since March 1st, 2011 = 0.78 days (12 % decrease) March 1st to June 30th 2011: Savings in ICU LOS +Savings in Vent Days $782,608.64 $398,329.62 = $1,180,938.26 Costs of Project - 18,062.50 TOTAL NET COST SAVINGS = $1,162, 875.76 Potential Cost Savings… $3,488,627.28 per year Upcoming Challenges Maintain gains and continue improvements Ongoing education (new staff) Continue to improve practitioners’ variability Implement initiatives in the Surgical ICU Upcoming Challenges Maintain gains and continue improvements Ongoing education (new staff) Continue to improve practitioners’ variability Implement initiatives in the Surgical ICU p value 0.012 Actual Performance for Sedation Holidays 80 Intervention 70 60 58 55 53 Percent 50 46 45 40 30 42 39 31 31 30 26 30 40 42 44 45 55 51 44 29 23 20 10 0 Jan Feb Mar Apr May Jun Jul 2010 Aug Sept Oct Nov Dec Jan Feb Mar Apr May Jun 2011 Jul Aug Sept Actual Performance Analgesia Holidays 80 Intervention 70 65 60 57 Percent 50 50 40 30 40 29 56 48 42 40 30 52 52 48 55 38 32 28 28 28 21 20 16 10 0 Jan Feb Mar Apr May Jun Jul Aug Sept Oct Nov Dec Jan Feb Mar Apr May Jun 2010 2011 Jul Aug Sept The Wean Team • CS & E Class Participants – Nisha Rathi, MD. – Clarence Finch, MBA, MHA, RRT, FCCM – Estella Estrada, BS – Nathan Wright, MD – Wendi Jones, MSN, ACNP-BC • Facilitator and Sponsor – Joseph Nates, MD, MBA-HCA, FCCM • Additional Team Members – – – – – – – – – – – – – – – – – – – – Laura Withers, MBA, RRT, CPFT Quan Ngyuen, BS, RRT Mick Owen, BSN, RN James Darden, RN, BSN Enedra McBride, RN, BSN Mary Lou Warren, RN, CNS, CCRN, CCNS Rhea Herrington, RN, BSN, CCRN Natalie Clanton, RN Jennifer Harper, RN Fallon Benavides, RN, MSN Jeffrey Bruno, PharmD, BCNSP, BCPS Gregory Botz, MD, FCCM Sajid Haque, MD Hetal Brahmbhatt, MHA, CPhT Lora Washington, MHA, JD Andrew Dinh, BS Hollie Lampton, B.S. Rose Erfe, B.S. Dee Cano Edward Scott, B.S, 43