Reducing Harm in the MICUo
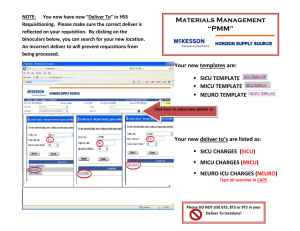
advertisement

Reducing Avoidable Harm in the MICU Reducing Avoidable Harm in the MICU November 4, 2010 Background • The incidence of Healthcare-associated infections (HAIs) is approximately 4.5 for every100 hospital admissions. • Health care-associated infections (HAIs) result in 1.7 million infections and 99,000 deaths each year. • The added financial burden attributable to HAIs is estimated to be between $35.7 billion to $45 billion for in-patient hospital services1. -CDC March 2009 Our Aim • Our aim at UT Southwestern is to address patient safety issues by reducing the number of safety related events by 50% by end of calendar year 2010. • The priority areas for this project are • Catheter –associated urinary tract infections (CAUTI) • Ventilator associated pneumonias (VAP) • Central line associated blood stream infections (CLABSI) • Patient falls Our 2009 MICU Baseline • 72 patients were harmed in our MICU in 2009 – 14 Patients with Ventilator Associated Pneumonia “VAP” – 23 Patients with Central Line Associated Blood Stream Infections “CALBSI” – 26 patients with Catheter Associated Urinary Tract Infections “CAUTI” – 9 Patient Falls Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? Act Plan Study Do Pareto Chart Avoidable Harm CVICU, MSICU, 7 West ICU CY 2009 30 100% 26 23 80% 17 17 60% 14 15 14 40% 9 20% CV VAP MS FALLS CV FALLS 7 MS VAP CV CALBSI CV CAUTI 5 MS CLABSI 10 MS CAUTI HAI TALLY 20 Cumulative % 25 0 0% HEALTHCARE ASSOCIATED HARM Vital Few Useful Many Cumulative% Cut Off % [42] Our Unit Comparison 2009 MICU = 72 CVICU = 55 CAUTI= 26 CLABSI = 23 VAP = 14 Falls = 9 CLABSI = 17 CAUTI = 17 Falls = 14 VAP = 7 Interventions All ICU VAP Bundle Compliance 100.0% 98.0% 96.0% 94.0% 92.0% % Compliance 90.0% All Bundle Elements 88.0% 86.0% 84.0% 82.0% 80.0% Feb-10 7 West ICU MSICU CVICU Feb-10 91.5% 93.0% 86.7% Mar-10 94.2% 95.1% 91.9% Mar-10 Apr-10 93.1% 97.7% 95.3% Apr-10 May-10 May-10 99.3% 97.1% 97.5% Jun-10 Jun-10 97.1% 97.0% 96.8% Jul-10 Jul-10 99.3% 97.6% 97.3% Aug-10 Aug-10 99.4% 97.5% 98.3% Sep-10 Sep-10 98.5% 98.2% 97.6% Avoidable Harm Tally MSICU & 7 West ICU 14 Harm Tally MICU 12 Started CS & E 10 8 Engaged the staff: re-educated and applied bundles 6 4 Joined CUSP Automated bundle compliance audits 2 Yellow Socks for ICU patients 0 MICU 2009 Harm Totals UCL +2 Sigma +1 Sigma Average -1 Sigma -2 Sigma LCL Process Map VTE Prophylaxis Process Map PUD Prophylaxis Process Map Indwelling Catheter Necessity Process Map Central Line Maintenance Fishbone Diagram Patient Falls People Processes Poor Vision Age Unsteady gait, weakness Slow response time Diarrhea Nurse doesn’t get there quick enough Non compliant Nurse doesn’t make it to room in time to assist to bathroom Confused Non skid slippers not in use Syncope Fall precaution not instituted Bed alarms not in use Left in bathroom alone Fall Risk Patient not informed of fall risk MI, PE Noted as fall risk but not treated as fall risk Urinary frequency Bed alarms not in use for fall risk Not wearing non slip socks Not clear who fall patients are. Lack of Patient doesn’t call communication Patient doesn’t want to burden staff by calling for help Falls SCDs IV Pumps Foley Oxygen tubing No BSC available Wound vac Room lighting. Rooms are dark at night Equipment Slip on wet floors Rooms far away from nurses station Cords Environment Process Diuretics, Lasix Laxative Pain Medications Shift Change P.T. evaluation not ordered Transfer at shift change or nurse not informed when patient arrives on unit Combined MICU Rate per 1000 pt days 22.00 20.00 MICU HAC Rate per 1000 pt days 18.00 16.00 Started CS & E 14.00 Automated bundle compliance audits 12.00 10.00 8.00 Engaged the staff: re-educated and applied bundles 6.00 Yellow Socks for ICU patients 4.00 Visual Cues for bundle compliance 2.00 0.00 Joined CUSP MICU HAC/ 1000 pt days UCL +2 Sigma +1 Sigma Average -1 Sigma -2 Sigma LCL Our Results 2009 Total & Q1-Q3 CY 2010 Comparison MICU Falls, CLABSI, CAUTI, VAP 80 75 72 70 Tally of Avoidable Harm 65 60 55 50 50 45 40 35 30 22 25 20 15 10 5 0 MICU & Avoidable Harm 2009 MICU Avoidable Harm Q1Q3 CY 2009 MICU Avoidable Harm Q1Q3 CY 2010 MICU Falls 2009 Total & Q1-Q3 Comparisons 10 9 Number of CLABSI Cases 9 8 7 6 6 5 4 3 2 2 1 0 Falls 2009 Falls Q1-Q3 CY 2009Falls Q1-Q3 CY 2010 MICU VAP 2009 Totals & Q1-Q3 Comparisons 16 Number of VAP Cases 14 14 12 10 8 8 6 4 3 2 0 MICU Total VAP 2009 VAP Q1-Q3 2009 VAP Q1-Q3 2010 MICU Central Line Associated BSI 2009 Total & Q1-Q3 Comparisons Number of CLABSI Cases 25 20 15 10 23 17 5 2 0 CLABSI MICU 2009 CLABSI Q1-Q3 CY 2009 CLABSI Q1-Q3 CY 2010 2009 Totals & Q1-Q3 CY2010 Comparison CVICU Falls, VAP, CAUTI, CLABSI 60 55 Tally of Avoidable Harm 55 50 45 40 38 35 30 25 23 20 15 10 5 0 CVICU Avoidable Harm CVICU Avoidable Harm CVICU Avoidable Harm 2009 Q1-Q3 CY 2009 Q1-Q3 CY 2010 CVICU Catheter Associated UTI 2009 Totals and Q1-Q3 Comparisons 18 17 16 Number of CAUTI Cases 14 11 12 10 7 8 6 4 2 - CVICU Total CAUTI 2009 CAUTI Q1-Q3 CY 2009 CAUTI Q1-Q3 CY 2010 MSICU, 7 West ICU, CVICU Combined Avoidable Harm 18.00 Avoidable Harm Tally 16.00 14.00 12.00 10.00 8.00 6.00 4.00 2.00 0.00 Harm / 1000 Pt Days UCL +2 Sigma +1 Sigma Average -1 Sigma -2 Sigma LCL 2009 Total & Q1-Q3 CY 2010 Comparisons Tally of Avoidable Harm Combined MICU & CVICU Falls, CLABSI, CAUTI, VAP 135 130 125 120 115 110 105 100 95 90 85 80 75 70 65 60 55 50 45 40 35 30 25 20 15 10 5 0 127 88 45 MICU & CVICU Avoidable Harm 2009 MICU & CVICU MICU & CVICU Avoidable Harm Q1-Q3 Avoidable Harm Q1-Q3 CY 2009 CY 2010 Estimated Avoidable Costs 2009 & Q1-Q3 Estimated Avoidable Costs* MICU VAP, CLABSI, CAUTI $1,200,000.00 $1,095,882.00 $1,000,000.00 $770,350.00 $800,000.00 $600,000.00 86.78 % Reduction $400,000.00 $200,000.00 $144,858.00 $0.00 Estimated Costs of HAI 2009 *Centers for Disease Control and Prevention. ( March 2009) Estimated Costs of HAI Q1- Estimated costs of HAI Q1Q3 2009 Q3 CY2010 2009 & Q1-Q3 Estimated Avoidable Costs* CVICU VAP, CLABSI, CAUTI $800,000.00 $712,327.00 $700,000.00 46.44% Reduction $600,000.00 $531,997.00 $500,000.00 $381,541.00 $400,000.00 $300,000.00 $200,000.00 $100,000.00 $0.00 Estimated Costs of HAI 2009 Estimated Costs of HAI Q1- Estimated costs of HAI Q1-Q3 Q3 2010 CY2010 *Centers for Disease Control and Prevention. ( March 2009) 2009 & Q1-Q3 Estimated Avoidable Costs* MICU & CVICU VAP, CLABSI, CAUTI $2,000,000.00 $1,808,209.00 $1,800,000.00 $1,600,000.00 $1,400,000.00 $1,302,347.00 69.11 % Reduction $1,200,000.00 $1,000,000.00 $800,000.00 $540,482.00 $600,000.00 $400,000.00 $200,000.00 $0.00 Estimated Costs of HAI 2009 *Centers for Disease Control and Prevention. ( March 2009) Estimated costs of HAI Q1- Estimated costs of HAI Q1Q3 2009 Q3 CY2010 Next Steps MICU Avoidable Harm Tally 14 12 MICU HAC Tally 10 ? 8 6 4 2 0 MICU 2009 Harm Totals UCL +2 Sigma +1 Sigma Average -1 Sigma -2 Sigma LCL CVICU Avoidable Harm Tally CVICU Avoidable Harm Tally 10 8 ? 6 4 2 0 Totals UCL +2 Sigma +1 Sigma Average -1 Sigma -2 Sigma LCL 7 West, MICU, & CVICU Combined Avoidable Harm 22 20 MICU HAC Rate per 1000 pt days 18 ? 16 14 12 10 8 6 4 2 0 J F M A M J J A S O N D J F M MICU HAC/ 1000 pt days UCL +2 Sigma +1 Sigma Average -1 Sigma -2 Sigma LCL A M J J A S Q1-Q3 CY2010 Avoidable Harm CVICU, 7 WEST ICU, MSICU 16 100% 15 14 80% 60% 7 6 6 40% 3 CV FALLS MS VAP CV VAP 2 CV CAUTI 4 CV CALBSI 3 0 2 2 MS FALLS 7 MS CLABSI 8 Cumulative % 10 MS CAUTI HAI TALLY 12 20% 0% HEALTHCARE ASSOCIATED HARM Vital Few Useful Many Cumulative% Cut Off % [42] Beyond the Bundles • Safety Debriefing – Allows us to study where our systems and processes failures – Involves the direct care-giver team in the unit, – We conduct the safety debriefing close to the time of occurrence – Helps quantify common causes for failures in order to systematically improve our processes Acknowledgement • Core Team: – Mike Mayo RN Manager MICU, – Chris Davis RN Clinical Coordinator 7 West ICU, – Pearl Kim RN Clinical Coordinator MSICU, – Pamela Woltjen AA • Nursing and Respiratory Therapy Staff MSICU, 7 West ICU, CVICU • Tammie OConnor RN CC CVICU • Internal Medicine Faculty and Fellows • Special Thanks to Dr. Gary Reed Reference 1. Centers for Disease Control and Prevention. ( March 2009) The Direct Medical costs of Healthcare-Associated Infections in U.S Hospitals and the Benefits of Prevention. Division of Healthcare Quality Promotion. National Center for Preparedness, Detection, and Control of Infectious Disease. Coordinating Center for Infectious Diseases