AMI Door Balloon Time
advertisement

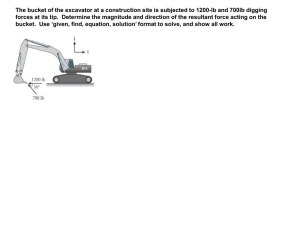
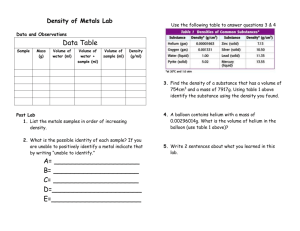
AMI Door to Balloon Time Overview • Primary entry for ST-Segment Elevation Myocardial Infarction (STEMI) patients is through our emergency room. • Improvement focus was in ED with collaboration with Cathertization Laboratory Services and Rapid Assessment Team personnel. • Facility is a tertiary-care 672 bed county teaching hospital • Over 108,000 annual ED visits, over 400 a day, projected to reach almost 200,000 for 2010. • Changes needed to improve patient care and meet organizational defined quality measure performance standards. Alignment with organizational goals to produce leading patient outcomes through our patients obtaining the right care, in the right setting, by the right providers at the right time. The Team Team Lead: Ellen O’Connell, MD Robert Madris, RN, MSN, Assistant Professor, Emergency Services AMI Core Measure Analyst Project Manager: Margie Roche, MS Performance Improvement Project Manager Facilitator: Peter Hoffman, SVP & Chief Quality Officer Rusty Genzel, RN CCRN Physician Champion: Ellen O’Connell, MD Emergency Department Service Manager Assistant Professor, Emergency Services Tayo Addo, MD Executive Sponsors: Assistant Professor, Internal Medicine Cardiology, Cardiac Catheterization Service Bradley Simmons, SVP Surgical Services Josh Floren, SVP Medicine Services Jana Seale, RN III, Cardiac Catheterization Service Maury Belino, RN, PM Staff Nurse, Emergency Department Landon Sweeny, RN, AM Staff Nurse, Emergency Department CS&E Participants What We Are Trying to Accomplish? AIM STATEMENT Timely identification of STEMI and opening of blocked coronary arteries (Door to Balloon) improves patient outcomes. Quality measure guidelines define effective door to balloon time as less than 90 minutes from arrival at hospital until the balloon is up. Historically, from October 2008 through December 2009, an average of 54% STEMI patients achieved a door to balloon time of less than 90 minutes. The goal of this project is to achieve door to balloon time of less than 90 minutes in over 95% of patients with STEMI. How Will We Know That a Change is an Improvement? Type of Measures Target for Measures Door to Balloon Time ≤ 90 minutes for ≥ 95% of STEMI Patients Door to EKG Time ≤ 10 minutes Arrival to ED Departure Time ≤ 30 minutes Arrival to Balloon Up ≤ 90 minutes How will you Measure? • All measurements will be collected through use of existing systems in ED, Cath Lab, and Cardiology (i.e., EPIC, Cardiology Systems, MUSE). • Reported Core Measure data will also be used. Baseline Data Mean Door to Balloon in Minutes x x-bar = 66 Min LCL UCL Target= <90 Min 200 180 160 140 Minutes 120 100 80 60 40 20 PODS Live ASAP Live Staffing to Volume New Residents 0 1 3 Q4 '08 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 53 55 57 59 61 63 65 Q1 '09 Q2 '09 Q3 '09 Q4 '09 Q1 '10 Baseline Data AMI 8a - Door to Balloon Percent of Cases ≤ 90 Minutes Target is ≥ 95% P UCL Average LCL Target 100% 95% 90% Percent of Cases ≤ 90 Minutes 80% 70% 60% 50% 40% 30% 20% 10% 0% Data as reported to UHC Core Measures and from Cases that Met Criteria Baseline Process Analysis Tools Plan Activity Who When Team Charter Developed – Board Directed Dr. Hoffman 3/28/2010 Describe Current Process •Process Flow Chart Team 4/2010 Team 5/2010 Ongoing Ongoing Team 4/2010 – 6/2010 Measure & Analyze Data • Core Measure Knowledge Survey • Core Measure Quarterly Data • Chart Reviews Identify Improvement Opportunities •Brainstorming •Survey Results – Open Ended Analysis •Chart Review Identify Root Causes of Problem •Specific Root Cause Not Identifiable •Several Small Areas of Possibility Generate & Choose Solutions •Process Flow Chart – Future State •Critical Path Exercise •Brainstorming & Consensus 4/2010 – 6/2010 Team Team 6/2010 – 7/2010 Baseline Process Analysis Tools Selected Decision Making Tools Chart Review Trending Information for Outliers 10 Selected Decision Making Tools 11 Selected Decision Making Tools Team Focus DO Plan included 3-key areas: • Earlier identification and treatment of STEMI patients • Faster movement of patient from ED to Cath Lab • Education of Staff on performance measures and changes Implementing Change • Earlier Identification of STEMI • Nurse driven Walk Back Chest Pain Order Set – Triage Lead • Revised ED Chest Pain directive procedure • Faster movement from ED to Cath Lab • Standardized Patient Prep Order Set • After Hours RAT nurse straight to Cath Lab • Cath Lab Notification of Patient Arrival Time » Arrival time added to Cath Lab activation page » Arrival time to be placed on colored arm band • Clock Synchronization » Synchronize ED, Cath Lab and EKG machines to all be on EPIC (EMR) time • Physician Education of STEMI Identification • Review EKGs of Cath Lab Activation cases with ED Physicians • Survey personnel involved in STEMI Case next business day • Monthly case review – cross-functional team Future State Process Future State Process Future State Process Results/Impact Check Activity Date Data Collection (Preliminary Data) August 16 – September 17, 2010 Data Analysis September 18 – September 24, 2010 3rd QTR Data (Preliminary) October 30, 2010 Results/Impact Interventions in ED triage and Cath Lab activation processes have: • Decreased overall mean time from 123.4 minutes to 56.1 minutes. • Increased overall performance from 57% to 90% of cases having door to balloon time of less than 90 minutes. Interventions April 1, 2010 August 31, 2010 STEMI Patient Door to Balloon Time Total Time in minutes UCL Average LCL Target ≤ 90 600 500 Total Time in minutes UCL 400 300 Triage Process Change: Triage Lead Order EKG RAT/CATH Nurse call ready for patient to ED Charge Nurse instead of coming to ED 200 FEB Patient EPIC arrival time added to Cath Lab Activation STAT Page 123.4 MAR 100 JAN MAY JUN JUL 56.1 77.2 Baseline Data 90 AUG 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 January 1, 2010 through August 31, 2010 April through August data is not final. Interventions: Overall Performance AMI 8a - Door to Balloon Percent of Cases ≤ 90 Minutes Target is ≥ 95% P 100% UCL Average UCL 2(2) 1(1) Target ≥ 95 LCL 2(2) 4(4) 5(5) 9(10) Percent of Cases ≤ 90 Minutes 90% 5(6) 80% 70% 60% 50% 2(3) 3(5) CL 2(4) 57% 1(2) 40% 5(6) 4(5) 2(3) 90% 1(2) 2(5) 1(2) 1(2) 3(7) 2(6) 30% 1(4) 1(4) 20% Inter ventions 10% 0% 0(2) Data as reported to UHC Core Measures and from Cases that Met Criteria April-10 through Aug-10 preliminary - not final x(x)₌ successful case (total cases meeting core measure criteria) Expansion of Our Implementation Act Activity Date Handoff October 2010 (TBD) Maintain Gain •Follow Up Surveys •Case Reviews •CM Reports Ongoing Monthly Sessions Quarterly Monitoring Cases •Physician Quality Conference Monthly Lessons Learned • There was not one single root cause for prolonged door to balloon time. • Multiple factors such as atypical presentation, awareness of core measures by staff, delay in EKGs and other contributed to performance less than target. • Importance of having representation from all disciplines was crucial to implementing changes. • Physician understanding of reporting requirements for core measures and how important documentation is for reporting was crucial to change. • Do not have meetings on Monday’s – multiple holidays caused some missed meeting days. At time of team start up identify alternate days for holidays. Conclusions Current results are preliminary and data will not be finalized until December 2010. However, early results indicate that initial interventions have had a positive effect on door to balloon time. Short Term Steps: • Refinement of Interventions • Development of ongoing education for nurses and physicians • Improving communication between ED physicians and Cath Lab physicians • Updating Equipment (i.e., EKG machines and Fax/Scanners) Long Term Steps: • Analysis of return on investment related to decreased length of stay and decreased morbidity in patients experiencing door to balloon time of <90 minutes. • Research and possible use of field activation of Cath Lab by paramedics and EMS personnel • Feasibility study of 24/7 Cath Lab Staffing Acknowledgments Thank you for the guidance and information sharing throughout the process of our program. – Peter Hoffman, MD • Senior Vice-President and Chief Quality Officer – Marisa Valdes, RN • Interim Director of Performance Improvement Thank you!