The Role of AHRQ and the UT System
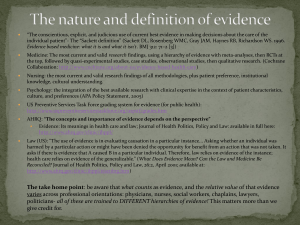
advertisement
Building a Bridge Over the Quality Chasm: The Role of AHRQ and the UT System Carolyn M. Clancy, MD Director Agency for Healthcare Research and Quality UT Clinical Safety and Effectiveness Inaugural Conference Austin, TX – October 15, 2009 The Fundamental Problem “The fundamental problem with the quality of American medicine is that we’ve failed to view delivery of health care as a science. … That’s a mistake, a huge mistake.” Peter Pronovost, MD Challenges Concerns about health spending – about $2.3 trillion per year in the U.S. and growing Pervasive problems with the quality of care that people receive Large variations and inequities in clinical care Uncertainty about best practices involving treatments and technologies Translating scientific advances into actual clinical practice and usable information both for clinicians and patients Building a Bridge at the Quality Chasm AHRQ’s Role The Quality Chasm Getting There from Here Q&A AHRQ’s Mission Improve the quality, safety, efficiency and effectiveness of health care for all Americans HHS Organizational Focus NIH CDC AHRQ Biomedical research to prevent, diagnose and treat diseases Population health and the role of community-based interventions to improve health Long-term and system-wide improvement of health care quality and effectiveness AHRQ Priorities Patient Safety Health IT Patient Safety Ambulatory Patient Safety Organizations New Patient Safety & Quality Measures, Safety Grants Drug Management and Patient-Centered Care Patient Safety Improvement Corps Medical Expenditure Panel Surveys Effective Health Care Program Comparative Effectiveness Reviews Comparative Effectiveness Research Clear Findings for Multiple Audiences Other Research & Dissemination Activities Visit-Level Information on Quality & Cost-Effectiveness, e.g. Medical Expenditures Annual Quality & Disparities Reports Prevention and Pharmaceutical Outcomes U.S. Preventive Services Task Force MRSA/HAIs AHRQ Roles and Resources Health IT Research Funding • Support advances that improve safety and quality • Continue work in hospital settings • Step up use of HIT to improve ambulatory care Develop Evidence Base for Best Practices • Patient-centered care • Medication management • Integration of decision support tools • Enabling quality measurement Promote Collaboration and Dissemination • Support efforts of other federal agencies (e.g., CMS, HRSA) • Build on public and private partnerships • Use web tools to share knowledge and expertise AHRQ FY 2009 Funding $372 million – $37 million more than FY 2008 – $46 million more than the president’s request FY 2009 appropriation includes: – $50 million for comparative effectiveness research, $20 million more than FY 2008 – $49 million for patient safety activities – $45 million for health IT Plus: significant ARRA funding (more on that later) Building a Bridge at the Quality Chasm AHRQ’s Role The Quality Chasm Getting There from Here Q&A The Quality Chasm: The STEEEP Challenge In 1999, in To Err is Human, Institute of Medicine estimated that 44,000 to 98,000 patients die each year in the United States as a result of medical error In 2001, IOM observed that a “quality chasm” exists between the care that should be provided and care that actually is provided IOM defined quality care as care that is safe, timely, effective, efficient, equitable, and patient centered 2008 Healthcare Quality Report Key Themes – Health care quality is suboptimal and improves at a slow pace (1.8% annually for core measures; 1.4% for all measures) – Reporting of hospital quality is spurring improvement, but patient safety is lagging – Health care quality measurement is evolving but much work remains 2008 Healthcare Disparities Report Key Themes: – Disparities persist in health care quality and access – Magnitude and pattern of disparities are different within subpopulations – Some disparities exist across multiple priority populations Texas: Dashboard on Overall Health Care Quality vs. All States Average Weak Strong Very Weak Very Strong Performance Meter: All Measures = Most Recent Year = Baseline Year 2008 National Healthcare Quality Report, State Snapshots Texas Snapshot Measure Performance % of hospital patients age 65 and over with pneumonia who received pneumococcal screening or vaccination Better than average % of hospital patients with heart attack who received aspirin within 24 hours of admission Average % of adult surgery patients who received Worse than appropriate timing of antibiotics average 2008 National Healthcare Quality Report, State Snapshots Tools to Address the Chasm Health IT (efficiency, timeliness) Comparative effectiveness research (safety, effectiveness) Direct engagement with consumers (equity, patientcenteredness) AHRQ Health IT Research Funding Long-term agency priority AHRQ has invested more than $260 million in contracts and grants More than 150 communities, hospitals, providers, and health care systems in 48 states AHRQ Health IT Investment: $260 Million AHRQ Health IT Initiative State and regional demonstrations Health IT grants Privacy and security solutions for interoperable health information exchange ASQ Initiative E-prescribing pilots CDS demonstrations Technical assistance for Medicaid and CHIP agencies AHRQ National Resource Center for Health IT Established in 2004 Central national source of information and assistance for advancing health IT goals Maintains operation of the AHRQ health IT Web site Direct technical assistance to AHRQ grantees Repository for lessons learned from AHRQ’s health IT initiative Health IT EPC Report First synthesis of existing evidence on factors influencing the usefulness, usability, barriers and drivers to use, and effectiveness of consumer applications The top factor associated with use by patients was the perception of a health benefit Patients prefer systems tailored to them that incorporate familiar devices AHRQ National Resource Center for Health IT Web Site http://healthit.ahrq.gov/ Features AHRQ’s portfolio of health IT projects Funding opportunities News releases Emerging lessons and best practices Meetings and events Ambulatory Safety and Quality (ASQ) Program Purpose: Improve safety and quality of ambulatory health care in the U.S. More than 60 grants Sample types of health IT used in projects: – PHRs – Clinical/medication reminders – Clinical decision support – Telehealth – Human/machine interface ASQ Grants: Texas Using Electronic Records To Detect and Learn From Ambulatory Diagnostic Errors – University of Texas Health Science Center at Houston – Type of Health IT: Operational decision support (quality of care) – Duration of Project: 9/30/2007 – 9/29/2009 Using Information Technology To Provide Measurement-Based Care for Chronic Illness – Texas Southwest Medical Center at Dallas – Type of Health IT: CDS (provider-focused) – Duration of project: 9/3-/2007 – 9/29/2010 What is Comparative Effectiveness Research? Essential Questions Posed by Comparative Effectiveness Essential Questions Posed by Comparative Effectiveness Is this treatment right? Is this treatment right for me? AHRQ Comparative Effectiveness Research http//:effectivehealthcare.ahrq.gov Effective Health Care Program A. Evidence synthesis (EPC program) – – Systematically reviewing, synthesizing, comparing existing evidence on treatment effectiveness Identifying relevant knowledge gaps B. Evidence generation (DEcIDE, CERTs) – – Development of new scientific knowledge to address knowledge gaps. Accelerate practical studies C. Evidence communication/translation (Eisenberg Center) – – Translate evidence into improvements Communication of scientific information in plain language to policymakers, patients, and providers AHRQ Priority Conditions Arthritis and non- traumatic joint disorders Cancer Cardiovascular disease, including stroke and hypertension Dementia, including Alzheimer Disease Depression and other mental health disorders Developmental delays, attention-deficit hyperactivity disorder and autism Diabetes Mellitus Functional limitations and disability Infectious diseases including HIV/AIDS Obesity Peptic ulcer disease and dyspepsia Pregnancy including pre-term birth Pulmonary disease/Asthma Substance abuse Comparative Effectiveness and the Recovery Act The American Recovery and Reinvestment Act of 2009 includes $1.1 billion for comparative effectiveness research: – AHRQ: $300 million – NIH: $400 million (appropriated to AHRQ and transferred to NIH) – Office of the Secretary: $400 million (allocated at the Secretary’s discretion) Funding for health IT, prevention and other areas have implications for the Agency Translating the Science into Real-World Applications Examples of Recovery Act-funded Evidence Generation projects: – Clinical and Health Outcomes Initiative in Comparative Effectiveness (CHOICE): First coordinated national effort to establish a series of pragmatic clinical comparative effectiveness studies ($100M) – Request for Registries: Up to five awards for the creation or enhancement of national patient registries, with a primary focus on the 14 priority conditions ($48M) – DEcIDE Consortium Support: Expansion of multi-center research system and funding for distributed data network models that use clinically rich data from electronic health records ($24M) The Bottom Line “Patients’ ratings of hospital care are of interest because they are, in many ways, “the bottom line.”’ New England Journal of Medicine Patients’ Perspectives of Care in the United States New England Journal of Medicine 359;18 www.nejm.org October 30, 2008 AHRQ Patient Engagement Campaigns Primary Campaign Spanish-Language Campaign Men’s Preventive Health Campaign PSA by Fran Drescher Plain Language Guides in English & Spanish Hispanic Elderly Initiative HHS pilot initiative aimed at improving the health and quality of life for Hispanic elders Eight metropolitan communities selected to participate in the pilot: Chicago, Houston, Los Angeles, McAllen, Miami, New York, San Antonio, and San Diego Medicare participation and diabetes care are target areas of work for each of the communities Building a Bridge at the Quality Chasm AHRQ’s Role The Quality Chasm Getting There from Here Q&A Future Challenges Downstream effects of policy applications Using technology, but not letting technology determine our priorities Care coordination: what can we learn from large integrated systems? Public-private funding and participation likely a necessity Patients should always be engaged as partners: it’s about them, not about you What Does It Mean to Be ‘Patient-Centric?’ Technology and Consumers We create tools that make care more efficient for clinicians Consumers already are comfortable with the technology; they’re leading us, not the other way around Consumers are demanding tools to make their care more about them; let’s satisfy the demand! 21st Century Health Care Using Information to Drive Improvement: Scientific Infrastructure to Support Reform Information-rich, patientfocused enterprises Evidence is continually refined as a by-product of care delivery 21st Century Health Care Information and evidence transform interactions from reactive to proactive (benefits and harms) Actionable information available – to clinicians AND patients – “just in time” According to Yogi Berra “If you don't know where you are going, you might wind up someplace else.” Yogi Berra Funding Opportunities Opportunities for the field to become involved are made available as soon as possible: – To sign up for updates, visit http://effectivehealthcare.ahrq.gov – To review AHRQ’s standing program and training award announcements http://www.ahrq.gov/fund/grantix.htm Building a Bridge at the Quality Chasm AHRQ’s Role The Quality Chasm Getting There from Here Q&A