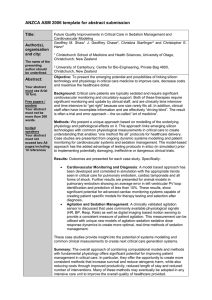
12601155_Visuals.ppt (15.29Mb)
advertisement

Don’t drive blind: Think smart
Future directions in medicine
15TH May 2006
Dr Geoff Shaw
Dept of Intensive Care Christchurch Hospital
Clin Sen Lecturer Dept of Medicine CSM&HS University of Otago, NZ
Senior Fellow Dept of Mechanical Engineering, University of Canterbury, NZ
Doctors aren’t so smart
Most treatments in medicine are delivered with
‘guess’ work
Sometimes you get lucky,
other times ….
Doctors aren’t so smart, and
patients aren’t so lucky
WHY?......
Students are not rewarded for their critical thinking;
good students are those that can reel off lists
and differential diagnoses
Most doctors had their mathematical skills
innovative ideas and beaten out of them at
medical school
Only use physics /math skills of year 8 students!!
Medical curriculum = do’s & don’ts
…1st law in
healthcare……
…2nd law in
healthcare…
How can I get out
of this jam?
Getting smart…
Agitation-sedation control
Blood glucose control
Dynamic models of renal failure
Lung disease models for improved ventilation
Cardiovascular models for diagnosis and treatment
Agitation control
Managing severe agitation is a nightmare
It’s “in your face”
It’s distressing
There’s no escape!
Therefore we “nail” the patient as quickly as
possible…..
A typical patient in our ICU….
“Hey! I think he just moved! Add one more!”
‘Nightmare on
ICU Street’
Re-enactment of
typical behaviour
Note level of force
needed to restrain
the ‘patient’
The impact….
Kress et al (N Engl J Med 2000;342:1471-7.)
Daily Interruption Of Sedative Infusions In Critically Ill
Patients Undergoing Mechanical Ventilation
Duration of mechanical ventilation:
4.9 days vs 7.3 days
Median length of stay:
6.4 days vs 9.9 days
The impact….
Brattebo et al (BMJ 2002;324:1386–9)
Effect of a scoring system and protocol for sedation on
duration of patients' need for ventilator support in a
surgical intensive care unit
Duration of mechanical ventilation:
5.3 days vs 7.4 days
Median length of stay:
8.3 days vs 9.3 days
Just imagine….
If poor sedation management contributes to 10%
extension in ICU length of stay:
In Aust /NZ….$50-100 million is wasted and 6-7000
patients denied intensive care annually
In the US…$1 B US wasted… ?
…100,000 patients denied intensive care..?
Yearly cost in US of sedatives & analgesics in ICU is
$0.8-1.2B US [Fraser and Riker, 2001]
Indeterminate number of patients are harmed or die
‘State of the art’; the problem of ‘control’
Each nurse is
different
Inconsistent
Nurse
Patient
Infusion Pump
Control changes
with nurse
Agitation and sedation assessments
are subjective….
Modified Riker Sedation-Agitation Scale (SAS)
SEDATION/AGITATION SCORE
DESCRIPTION
3
Dangerous agitation
Pulls at endotracheal tube (ET), Tries to remove
catheters, Climbs over bedrail, Strikes staff,
Thrashes from side to side
2
Very agitated
Does not calm, despite frequent verbal reminding of
limits, Requires physical constraints, Bites ET tube
1
Agitated
Anxious or mildly agitated, Attempts to sit up, Calms
down to verbal instructions
0
Calm and cooperative
Calms, awakens easily, Follows commands
-1
Sedated
Difficult to arouse, Awakens to verbal stimuli or gentle
shaking but drifts off again, Follows simple commands
-2
Very sedated
Arouses to physical stimuli but does not communicate or
follow commands, May move spontaneously
-3
Unarousable
Minimal or no response to noxious stimuli, Does not
communicate or follow commands
Sedation and
agitation are
linked – what if
you are difficult
to arouse and
agitated?
Descriptions are
vague and can
easily satisfy
more than one
Summary of ‘State of the Art’
Many ICU’s don’t even do
“over-customised care and over-sedation
this!
[Wiener-Kronish, 2001]
Longer
than
necessary
The result?? …
stay…in
hospitals
for many many days
… and many many $
Higher costs
Reduced
level
of
patient
… primarily due to a lack of a consistent
care
measure of agitation
Agitation
Sedation
Aims
To investigate a semi-automated method of
sedation that…
Allows rapid titration to measurements of agitation
Minimises over sedation
Has a simple user interface
Has minimal set of rules
Is acceptable by nursing staff
Stores data for clinical records and audit
-1
-1
-1
-1
-1
-1
-1
-1
+2
0
+3
+1
2
2
2
2
2
1+1+1
8
1+1+1+1
1
1
8
16
Development
Computerised paper sedation sheets:
n 1
1
y
[ y i xi ]
n
6 i n 4
yi = Background rate
xi = Bolus doses given for agitation
n = Number of hours
62 y female with multi-organ failure
17 y male with multi-trauma
30 nurses' ratings of the Infuse-Rite
Before using Infuse-Rite
After using Infuse-Rite
Highly
acceptable
10
9
8
7
6
5
4
3
2
Totally
unacceptable
1
Pain &
Agitation
Ease of
Personal
discomfort
control
Admin
safety
control Sedation
Time
Patient
Legal
control
efficiency
safety
safety
Sedation consumption & cost
Comparison of Christchurch vs Wellington sedation cost
from July 1, 2002 – Nov 30, 2003
Overall both units are estimated to have a similar case
mix, with slightly higher proportion of cardiac surgical
patients in Wellington, 40% vs 30%
The patients…
45.4
1419
1486
Christchurch Wellington
Patients
50.2
Christchurch
Wellington
Vent hours/ patient
Patient sedation dose
2413
145.4
69.0
496
Christchurch Wellington
Midazolam (mg)
Christchurch
Wellington
Propofol (mg)
Hourly dose
3.0
47.7
1.6
11.9
Christchurch
Wellington
Midazolam (mg) /vent-h
Christchurch
Wellington
Propofol (mg) /vent-h
Midazolam & Propofol
$113,175
$32,205
Christchurch
($) / year
$107.89
$32.15
Wellington
Christchurch
Wellington
($) /patient over 3.5 stays
Administration data from Infuse-Rite
3 years data from 1070 patients (Mar ‘02- Oct 05):
4,121,640 minutes of recorded data (7y 10m) total use
120,141 boluses / infusion rate changes
~36,000 additional boluses for procedures
>156,000 doses / infusion changes without error
Insights into agitation control…
We hypothesize that loss of agitation
control is a key driver of over sedation..
Period change
Morphine (mg)
First compute the mean,
the maximum and
minimum of the peak to
trough time period
t1 t 2 t 3 t 4 t 5 t 6
6
tmax t1, tmin t 3
t
A measure of stability is
then given by:
Time (days)
max{tmax t , t tmin}
Hurst Exponent
Measure of surface smoothness. 0<H<0.5 suggests a predictable oscillatory
pattern of sedation given for agitation. An increase in H suggests patient is
less responsive to sedation; extra doses are required and the system
becomes more chaotic Loss of control
Summary….
Minimised over sedation and eliminated drug error
Better consistency and control of agitation.
High degree of acceptance by nursing staff
Sedation cost by avoidance of expensive agents
Accurate medico-legal record for patient file
Data storage for research and audit
The Future…?
Pharmacokinetics
Concentration of drug
in Central compartment
Models kinetics of
drug infusion and
distribution
Models
transportation
to effect site,
and drug
elimination
U
Cc K1Cc
Vd
C p K3C p K2Cc
Concentration of drug in
Peripheral compartment
Standard twocompartment
Pharmacokinetics
Infusion rate
Volume of
distribution
Agitation Dynamics
Rate of change of
agitation depends
upon relative
magnitude of stimulus
compared to
cumulative effect of
Stimulus
sedation
Cumulative effect
of sedation
t
A w1S w2 KT C p ( )e
KT ( t )
0
Agitation Index
Drug Concentration in
Peripheral compartment
d
Patient+Nurse Simulator
Cc K1Cc
U
Vd
C p K3C p K2Cc
U K p A Kd A
t
A S C p ( )e K4 ( t ) d
0
Filters variability
of nurse input
Records infusion
data
What Data?
Recorded Data = Standard & Procedural Boluses+ Background rate
Modelled vs recorded data
Recorded
Simulated
Improvements…..
Morphine
Vc
Midazolam
dCc
( K CL K ce K cp )Cc PAU K ec Ce K pc C p
dt
Vp
Ve
dC p
dt
Vc
dCc
( K CL K ce )Cc PBU K ec Ce
dt
Ve
dCe
K ec Ce K ce Cc
dt
K pcC p K cp Cc
dCe
K ec Ce K ce Cc
dt
Pharmacokinetics
( )
UA
C e, morph
C50, morph
EComb
U A UB
U 50 ( )
E0 [ Emax ( ) E0 ]
( )
U A UB
1
U 50 ( )
UB
C e, midaz
C50, midaz
t
dA
w1S w2 KT EComb ( )e KT ( t )d
dt
0
Pharmacodynamics
Novel application of standard PK & PD
Novel Equation & Application
Morphine
Midazolam
3-Compartment
Model
2-Compartment
Model
Excretion
Infusion site
Infusion site
Blood flow
Blood flow
Peripheral
Pharmacokinetics
Brain
Effect site
Brain
• Response surface modeling [Minto et al, 2000]
• Dual sigmoid
• Incorporates effect saturation
EComb
• Captures synergism
• Non-linear representation of the
concentration-effect relationship
• Models the combined sedative effect of
the drugs on the brain
Morphine Effect-site
Concentration
Midazolam Effect-site
Concentration
Pharmacodynamics
Primary Equation
Cumulative effect of
current and prior sedation
Stimulus
t
dA
KT ( t )
w1S w2 KT EComb ( )e
d
dt
0
Agitation Index
Combined drug effect
Rate of change of agitation depends upon relative
magnitude of stimulus compared to cumulative effect
of sedation
Rudge, AD, Chase, JG, Shaw, GM and Lee, DS (2006). “Physiological Modelling of AgitationSedation Dynamics Including Endogenous Agitation Reduction,” Medical Engineering and
Physics, In Press
Quantification of Agitation
t
U K p A Kd A
dA
w1S w2 KT EComb ( )e KT ( t )d
dt
0
How can we measure agitation?
Use a wide variety of medical signals:
Heart rate
Respiratory rate
BP (systolic and diastolic)
Heart rate variability (HRV)
BP Variability
(BPV)
Patient Motion (MOV via webcam)
Use fuzzy mathematics to add in medical expertise and
organise a large amount of data into something
useful
HRV
Frequency Components
VLF: 0.0033 – 0.04
Hz
LF: 0.04 – 0.15 Hz
HF: 0.15 – 0.4 Hz
VLF/HF falls as variability drops
in agitated patients
BPV
HF/VLF falls as systolic BP variability
rises in agitated patients
ECG – HRV : Healthy Subjects
~20 min color word test CWT designed to
induce sympathetic responses similar to
agitated ICU patients
Red - the correct answer is “green”
VLF/HF ratio measured:
Under stress (agitation) HR rises; the heart beats more consistently (HF drops).
Therefore, rises in VLF/HF ratio indicate sympathetic responses akin to agitation.
ECG – HRV : ICU Patients
SAS = 1
SAS = 2
VLF/HF ratio measured:
100 minute sample shows two assessed times of significant agitation matched
by two peaks in the HRV VLF/HF ratio
BPV for an ICU patient
SAS
HF/VLF ratio measured:
Identifies agitation which correlates with nurse-assessed Riker SAS
(inverse to heart rate variability)
Quantifying Agitation – Fuzzy Systems
Fuzzy logic is good for modeling
uncertain system dynamics
Rules intuitive & based on medical
experience
Moving mean tracking over 1-20
minutes (can be tuned)
Rules tuned on healthy and then
applied to ICU
Fuzzy logic rules applied on measured data and result is a [0,100] output.
Quantify – Healthy & ICU subjects
4.4
input
signal: 4.2
HRV
HRV with fuzzy rules
HRV
4
(VLF/HF)
3.8
3.6
3.4
0
12.5
25
37.5
50
62.5
75
1
Agitation
level
0.8
HRV with fuzzy rules
BPV with fuzzy rules
0.6
Fuzzy
Rules
0.4
0.2
0
0
12.5
25
CWT START
37.5
50
62.5
CWT END
75
CP
Results are scaled [0, 1] for a simple comparison and metric
Digital imaging of motion with fuzzy rules
SAS
1
2
1
Chase JG, Agogue F, Starfinger, C, Lam Z, Shaw GM, Rudge AD, Sirisena H; Quantifying agitation
in sedated ICU patients using digital imaging. J of Computer Methods and Programs in
Biomechanics and Biomedical Engineering. 2004;76(2):131-141.
Combining
many metrics
How we might
do things
differently?
Tight glucose control
Hyperglycaemia is prevalent in critical care
Impaired endogenous insulin production
Increased effective insulin resistance
Average blood glucose values > 10mmol/L not uncommon in
some critical care units (over length of stay)
Stress of condition induces hyperglycaemia
Tight control better outcomes:
Reduced mortality 27-43% (6.1-7.75 mmol/L)
Reduced length of stay and length of mechanical ventilation
Active Insulin Control: Evolution
AIC 1 – 3 Development of Mathematical Model + 1st Trials
Insulin-only
AIC 4
Computerised Control Protocol
Insulin + Nutrition
AIC 5
New protocol with same (or better) control
Easy to implement in clinical environment
Comparison with international protocols
AIC1 AIC4: Prior Art
pG
SI
Gmeasured
t
+
• 4 years prior trials
and research
• Models mature
• Adaptive Control
• Short specific trials
Update parameters
u(t)
pG and SI
G pG G S I G Ge
Gmodelled
Q
1 GQ
P(t )
u (t )
I nI I b
V
Overall AIC control system concept is well established
The only ways to reduce glucose
levels are:
increase insulin (Q) which saturates
decrease feed (P)
G pG G S I G Ge
Glucose = G
Insulin = Q
Feed = P
Q
1 GQ
P(t )
Insulin-only (AIC3) control of a patient
Glucose level mmol/l
Tight control target = 4-6 mmol/l
Dextrose feed and Insulin input
Insulin boluses
Feed rate
Time (minutes)
Insulin-feed (AIC4) control of a patient
Glucose level mmol/l
Tight control target = 4-6 mmol/l
Dextrose feed and Insulin input
Feed rate
Insulin boluses
Time (minutes)
Patient 5 = textbook case
Wong, XW, Chase, JG, Shaw, GM, Hann, CE, Lotz, T, Lin, J, Singh-Levett, I, Hollingsworth, L,
Wong, OS and Andreassen, S (2006). “Model Predictive Glycaemic Regulation in Critical Illness
using Insulin and Nutrition Input: a Pilot Study,” Medical Engineering and Physics, In Press
SPRINT Specialised Relative Insulin and Nutrition Table
Optimises both insulin and nutrition rates to control
glycaemic levels
Developed through extensive computer simulation
Ensures safe protocol before clinical implementation
Simple interface for ease of use by nursing staff
Combines the very tight control of computerised
simulations with minimal implementation cost
(no bedside computer required…)
SPRINT Step 1 = Feed Rate Table
Requires current glucose
measurement and last
hour change in glucose
SPRINT Step 2 = Insulin Table
If feed rate = 0 use only insulin wheel
Requires current glucose
measurement, last hour
change and last hours
insulin bolus
Patient 5008
• Time = 163 hours
• Mean = 5.4 mmol/L
• 4-6.1 = 85%
• 4-7.75 = 97%
• Avg Feed = 85%
• Avg Insulin = 3.4 U/hr
Lonergan, T, LeCompte, A, Willacy, M, Chase, JG, Shaw, GM, Wong, XW, Lotz, T, Lin, J, and Hann,
CE (2006). “A Simple Insulin-Nutrition Protocol for Tight Glycemic Control in Critical Illness:
Development and Protocol Comparison,” Diabetes Technology & Therapeutics (DT&T), In Press
Results
Number of respondents
Nursing survey: SPRINT
15
Very Good
10
Good
Satisfactory
5
Poor
0
Ease of Use
Quality
Suitability
Results
16,063 hours of control on SPRINT; 11,249 measurements
118 admissions
Average APAPCHE II score = 21 (41% risk of death)
Too high
(hypoglycaemia)
(hyperglycaemia)
Number of
measurements
Too low
1500
2003 Retrospective Data (Doran, 2004)
Mean Glucose = 8.1
Lognormal = outliers to high side
Mean
1000
500
0
<4
4 to 6
6 to 8
8 to 10
10 to 12
2003
Numberofof
Number
measurements
measurements
3000
12 to 15
15 to 20
20 plus
Blood glucose [mmol/L]
SPRINT
Mean
2000
2000
Reduction in incidence
of high blood glucose
1000
1000
0
0
<3
<4
3 to
4
4 to 6
4 to 5 to
5
6
6 to
7
6 to 8
7 to
8
8 to 10
8 to
9 to
2005
9
10
10 to 12
10 to 11 to
11
12
Normal distribution -- 90% in desired band
12 to 15
15 to 20
20 plus
12 to 13 to 15 to 18 to
20
[mmol/L]
13
15
17 Blood
20 glucose plus
Tight control:
Tight control:
Tight control within
target bands
Areas under all fitted curves are equal
Poor control:
BG less than
2.5mmol/L =
harmful!!
3.5% of simulated van den Berghe measurements less than 2.5mmol/L
Poor control:
70% of simulated Krinsley
measurements > 7.75 mmol/L
10% of SPRINT ICU measurements
> 7.75 mmol/L
38% of simulated sliding scale
measurements > 7.75 mmol/L
Tight control
15.00
2003 retrospective data
Avg BG
Range
Retroavg
Retrorange
Flatter is better
Tighter is better
15.00
12.50
12.50
Blood 10.00
Glucose
Average
(mmol/l) 7.50
Blood 10.00
Glucose
Average
(mmol/l)
5.00
5.00
2005-06 SPRINT
Avg BG
Max
Retroavg
Retromax
Flatter is better
Tighter is better
7.50
R Sq Linear = 0.652
R Sq Linear = 0.283
R Sq Linear = 0.36
P < 0.05
P < 0.05
2.50
2.50
0.0
5.0
10.0
15.0
20.0
Blood Glucose Range (mmol/l)
5.0
10.0
15.0
20.0
Peak Blood Glucose (mmol/l)
SPRINT is flatter and tighter in both cases (P < 0.05)
R Sq Linear = 0.459
Outcomes:
Tightness of glucose control: the first 118 admissions
Average BG
Average time in 4 -6.1
Average time in 4 -7
Average time in 4 -7.75
Percentage of all measurements less than 4
Percentage of all measurements less than 2.5
Average insulin bolus
Average percentage of goal feed
Average feed rate
(assuming 1.06 cal/ml for feed)
5.9
60%
82%
90%
2.7%
0.1%
2.7
66%
51
1293
mmol/L
All performance indicators agree with
simulation and tight control!
Protocol is safe – no clinically significant
hypoglycaemia
U
Effective use of insulin and nutrition
ml/hr
cal/day
Improved patient outcome: LOS >3 days
.
30%
Mortality %
25%
SPRINT has decreased
mortality by 32%
20%
15%
10%
5%
44 deaths in
169 patients
23 deaths in
118 patients
0%
2004-05
SPRINT
P=0.04
Outcomes:
Tightness of glucose control*
SPRINT Mortality grouped by APACHE II
APACHE II
Number Mortality
0-14
20
5%
15-24
44
20%
25-34
23
26%
35+
6
67%
SPRINT Sepsis data
Total sepsis patients
Total sepsis LOS<3
Total sepsis LOS≥3
Mortality sepsis all
Mortality sepsis LOS<3
Mortality sepsis LOS≥ 3
*
Average APACHE II = 21
* Incomplete data
*
2004-05
Number
104
200
48
7
2004-05
21
3
18
4
1
3
49%
13%
25%
19%
33%
17%
35.0%
37.0%
34.0%
Mortality
1.9%
15.5%
45.8%
71.4%
(% change)
-46%
-10%
-51%
Average APACHE II =18.3
http:/www.geocities.com/active_insulin_control
Measuring Renal Function
Currently:
Creatine Creatinine
“Activity”
Another Way:
Both Cleared via Filtration
GFR
Urine
Gentamicin
Creatinine and Gentamicin can be measured in plasma and clearance estimated (AUC)
However, you need to know the production/input
Creatinine production is not known or well estimated
e.g. MDRD / Cockroft-Gault equation empirical models assume constant production and
steady state
Gentamicin doses are known and thus likely more reliable for AUC estimation
“Gold standard” = inulin or radioactive iodine compounds
Modeling Renal Function
C = concentration
2
uCreatinine
“Activity”
u
dC
kGFRC Creatinineor Gentamicin
dt
Vdistribution
GFR = KGFR*Vd
Urine
1
Gentamicin
kGFR
Steps:
1. Find kGFR clearance from Gentamicin measurements (AUC and model)
2.
Knowing kGFR find uCreatinine production
i.e. without guessing what it is!
3.
Knowing uCreatinine find Creatinine clearance (or just use Gentamicin clearance)
Cohort: n = 16 patients with both Gentamicin and Creatinine data from ICU
RESULTS: Model vs MDRD
“Easy” Patients : kGFR = time varying and uCreatinine = con
stant
“Easy” Patients:
uCreatinine = constant
kGFR not constant
GFR and u = patient specific
Cannot find uCreatinine and kGFR with
just Creatinine data alone.
i.e. over 50% of variation is not
explained by the MDRD model
Poor correlation too
much variation for good
diagnosis
“Hard” Patients:
uCreatinine NOT constant
kGFR not constant
Assumes measured Gentamicin clearance as a “gold standard”
MDRD steady state assumptions is not valid for ARF
Assuming constant Creatinine
production results in very large
errors (50+%) with measured data.
Conclusions
Creatinine production is not always constant
Limits its utility for measuring renal function
Constant Creatinine production is still patient specific requiring some
other form of measurement of renal function (which can be nonconstant)
Can get Creatinine production from Gentamicin clearance
But only works for “Easy” patients!
Going Forward…
An adaptive measure of renal function requires a substance in the
body with known constant production
Cystatin C? More constant, known production than Creatinine?
A larger set of trial data would enable more concrete conclusions
Modeling Lung Mechanics
Objective:
To develop a model of mechanics of ARDS
lung under mechanical ventilation to
determine the appropriate ventilator setting
in clinical situation.
Superimposed pressure
Model of the ARDS lung has up to 60,000 compartments which inflate
and deflate according to their threshold opening and closing pressures.
TOP’s, TCP’s are determined by the unit compliance and superimposed
pressure.
Opening
Pressure
(modified from Gattinoni)
Inflated
0
Small Airway
Collapse
10-20cmH2O
Alveolar Collapse
(Reabsorption)
40-60cmH2O
Consolidation
Model Components
Unit Compliance Curve
Based on Sigmoid Shape
Very little change in volume from alveoli
Threshold Pressure Distributions
Threshold Opening Pressure (TOP)
Threshold Closing pressure (TCP)
Normally distributed
Shifting distribution mean
Model Validation
Chase, JG, Yuta, T, Shaw, GM, Horn, B and Hann, CE (2005). “A Minimal Model of Mechanically Ventilated Lung
Mechanics to Optimize Ventilation Therapy in the Treatment of ARDS in Critical Care,” IFMBE Proceedings, 12th
Intl Conference on Biomedical Engineering (ICBME), Singapore, Dec 7-10, 4-pages, ISSN 1727-1983.
How does it work? – Step 1
Step 1
Obtain clinical data with
a few different PEEP
Step 2
Fit model
Step 3
Calculate parameters
Step 4
Simulate
Step 5
Determine optimal setting
How does it work? – Step 2
Step 1
Obtain clinical data with
a few different PEEP
Step 2
Fit model
Step 3
Calculate parameters
Step 4
Simulate
Step 5
Determine optimal
setting
How does it work? – Step 3
Threshold Pressure Distribution Mean Shift
4
TOP
3.5
3
Mean
Step 1
Obtain clinical data with
a few different PEEP
Step 2
Fit model
Step 3
Calculate parameters
Step 4
Simulate
Step 5
Determine optimal
setting
2.5
TCP
2
1.5
1
0.5
0
0
2
4
6
8
PEEP [cmH 2O]
10
12
14
How does it work? – Step 4
Step 1
Obtain clinical data with
a few different PEEP
Step 2
Fit model
Step 3
Calculate parameters
Step 4
Simulate
Step 5
Determine optimal
setting
How does it work? – Step 5
900
800
700
Tidal Volume [ml]
Step 1
Obtain clinical data with
a few different PEEP
Step 2
Fit model
Step 3
Calculate parameters
Step 4
Simulate
Step 5
Determine optimal setting
600
500
400
300
200
100
0
0
5
10
PEEP [cmH 2O]
15
20
‘Strengths’ in using this approach…..
Real time assessment of recruitment status which is
dependent on PEEP, ventilation strategy, and disease
Readily identifies TCP distributions
optimization of PEEP
Provides opportunity to simulate a ventilation strategy
before application.
TOP distribution characteristics
Prediction of “overstretch”. E.g. Δ recruitment < % max rate
? Correlated with E2% or CT scan
Limitations…
Although flow resistive forces through the endotracheal
tube are accounted for, the model assumes the pressure
at the carina will reflect what is happening to alveolar
units.
Unforeseen resistive changes (eg major bronchial airway
obstruction) could therefore lead to incorrect inferences
about recruitment status
Needs to be clinically validated
Minimal model of heart & circulation
Smith, B W, Chase, J G, Shaw, G M, Nokes, R and Wake, G C: Minimal Haemodynamic System
Model Including Ventricular Interaction and Valve Dynamics,Medical Eng and Physics, 2004;
26(2):131-139
Experimental pulmonary embolism in 8 pigs
Data kindly provided from a researchers in Belgium*
Pressure and volume in left ventricle
Pressure and volume in right ventricle
*Dr Thomas Desaive - Institute of Physics, University of Liège, Belgium
*Dr Alexandre Ghuysen - Hemodynamics Research Laboratory, University of Liège, Belgium
Experimental pulmonary embolism in pigs
Pressure and volume in left ventricle
Pressure and volume in right ventricle
Modelled cardiovascular dynamics
Provide rapid diagnosis in real time
optimised treatment
Simulation of interventions
removes guess work
Improved understanding
new paradigms and improved approach to the
haemodynamically unstable patient
Optimised therapeutics and
safer drug delivery …
....is out there …..
……It’s just a matter of seeing
where you are going!
Acknowledgements
AIC1
AIC2
Jessica Lin & AIC3
AIC V:
Cardiovascular Modelling:
Aaron Le Compte
Bram Smith
Jason Wong & AIC4
Dunedin
Tim Lonergan
Mike Willacy
Renal Function
Modelling:
Prof Zoltan Endre
Annie Jo
Assoc. Prof. Geoff
Chase
The Danes
Franck Agogue Thomas Lotz
Prof Steen
Andreassen
Christina Starfinger
Dr Kirsten
McAuley
& Zhewy Lam
Prof Jim Mann
Maths and Stats Gurus
Dr Dom Lee
Dr Bob
Broughton
Prof
Graeme Wake
Dr Chris Hann