Supplementary Material GFR estimating equations referred to in the text
advertisement

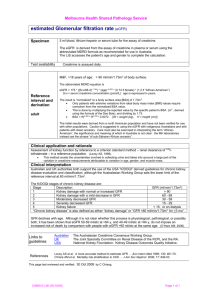
1(16) Supplementary Material GFR estimating equations referred to in the text In all equations p-creatinine (pCr) is expressed in mol/L, p-cystatin C (pCysC) in mg/L, age in years, weight in kilograms, height in centimetres and body surface area (BSA) in square meters. ln = natural logarithm. All creatinine equations except Cockcroft-Gault are based on IDMS-traceable creatinine assays. All cystatin C equations are based on assays calibrated against the internationally certified reference material ERM-DA471/IFCC [1]. All equations were developed based on Caucasian populations and include a factor for African Americans in the MDRD and CKD-EPI creatinine equations and in the CKD-EPI combined creatinine and cystatin C equation. The CAPA cystatin C equation were also based on an adult Asian population. Cockcroft-Gault and the Lund-Malmö equation with lean body mass (LM-LBMCREA) primarily express eGFR in absolute values in mL/min, while remaining equations primarily express relative GFR in mL/min/1.73 m2. Body surface area (BSA) according to DuBois & Dubois [2] BSA (m2) = (weight0.425 × height0.725) × 0.007184 Non-standardized creatinine equation for adults Cockcroft Gault [3] eGFR (mL/min) = 1.23 × [(140 – age) × weight/pCr] × 0.85 (if female). Standardized creatinine equations for adults Absolute Lund-Malmö with lean body mass (LM-LBMCREA) [4] eGFR (mL/min) = eX - 0.0128 × age + 0.387 × ln(age) + 1.10 × ln(LBM) X = –0.0111 × pCr (if pCr < 150 mol/L) X = 3.55 + 0.0004 × pCr - 1.07 × ln(pCr) (if pCr 150 mol/L) Lean body mass [5] Women: 1.07 × weight – 148 × (weight/height)2 Men: 1.10 × weight – 128 × (weight/height)2 2(16) Revised Lund-Malmö (LM-REVCREA) [6] eGFR (mL/min/1.73 m2) = eX – 0.0158 Age + 0.438 ln(Age) Female pCr < 150 mol/L: X = 2.50 + 0.0121 (150 - pCr) Female pCr 150 mol/L: X = 2.50 - 0.926 ln(pCr / 150) Male pCr < 180 mol/L: X = 2.56 + 0.00968 (180 - pCr) Male pCr 180 mol/L: X = 2.56 - 0.926 ln(pCr / 180) MDRDCREA [7] eGFR (mL/min/1.73 m2) = 175 × (pCr / 88.4)-1.154 × age-0.203 × 0.742 (if female) × × 1.210 (if African American) CKD-EPICREA [8] eGFR (mL/min/1.73 m2) = Female pCr ≤ 62 mol/L: 144 (pCr / 62)-0.329 0.993Age Female pCr > 62 mol/L: 144 (pCr / 62)-1.209 0.993Age Male pCr ≤ 80 mol/L: 141 (pCr / 80)-0.411 0.993Age Male pCr > 80mol/L: 141 (pCr / 80)-1.209 0.993Age All expressions multiplied with 1.159 if African American. Standardized creatinine equations for children SchwartzCREA [9] eGFR (mL/min/1.73 m2) = 36.5 × height (cm) / pCr GaoCREA [10] eGFR (mL/min/1.73 m2) = 60 × (height / pCr) - 6.25 × (height / pCr)2 + 0.48 × age – K (K = 25.68 for females and 21.53 for males). Standardized cystatin C equation for adults and children CAPACYSC [11] eGFR (mL/min/1.73 m2) = 130 × pCysC-1.069 × Age-0.117 – 7 3(16) Standardized cystatin C equation for adults CKD-EPICYSC [12] eGFR (mL/min/1.73 m2) = pCysC ≤ 0.8 mg/L: 133 (pCysC / 0.8)-0.499 0.996Age 0.932 (if female) pCysC > 0.8 mg/L: 133 (pCysC / 0.8)-1.328 0.996Age 0.932 (if female) Standardized combined creatinine and cystatin C equation for adults CKD-EPICREA+CYSC [12] eGFR (mL/min/1.73 m2) = Female pCr ≤ 62 Female pCr ≤ 62 Male Male pCr ≤ 80 pCr ≤ 80 pCysC ≤ 0.8 130 × (pCr / 62)−0.248 × (pCysC / 0.8)−0.375 × 0.995Age pCysC > 0.8 130 × (pCr / 62)−0.248 × (pCysC / 0.8)−0.711 × 0.995Age pCysC ≤ 0.8 130 × (pCr / 62)−0.601 × (pCysC / 0.8)−0.375 × 0.995Age pCysC > 0.8 130 × (pCr / 62)−0.601 × (pCysC / 0.8)−0.711 × 0.995Age pCysC ≤ 0.8 135 × (pCr / 80)−0.207 × (pCysC / 0.8)−0.375 × 0.995Age pCysC > 0.8 135 × (pCr / 80)−0.207 × (pCysC / 0.8)−0.711 × 0.995Age pCysC ≤ 0.8 135 × (pCr / 80)−0.601 × (pCysC / 0.8)−0.375 × 0.995Age pCysC > 0.8 135 × (pCr / 80)−0.601 × (pCysC / 0.8)−0.711 × 0.995Age Standardized combined creatinine and cystatin C equation for children ChehadeCREA+CYSC [13] eGFR (mL/min/1.73 m2) = 0.42 × [height (cm) / (pCr / 88.4)] – 0.0004 × [height (cm) / / (pCr/88.4)]2 – 14.5 × cystatin C + 0.69 × age + K (K = 18.25 for females and 21.88 for males). GFR calculators Easy available calculators exist for LM-REVCREA, CAPACYSC and their arithmetic mean MEANLMREV+CAPA (egfr.se/eGFRen.html) as well as for the CKD-EPI equations (www.kidney.org/professionals/kdoqi/gfr_calculator.cfm) and give the results for both single and combined marker equations. 4(16) Methods to Estimate and Measure Renal Function (Glomerular Filtration Rate). Chapter 3.2, Validation of GFR estimating equations in large patient groups. A systematic review by the Swedish Council on Health Technology Assessment, Available at www.sbu.se/214, Accessed March 1, 2015. Summary and conclusions in English is available at http://www.sbu.se/en/Published/Yellow/Methods-to-Estimate-and-Measure-Renal-FunctionGlomerular-Filtration-Rate/, Accessed March 1, 2015. The systematic search for studies ended in October 25, 2011. Overall aim The overall aim of Chapter 3.2. was to assess how accurate equations based on creatinine, cystatin C or the combination of the two analytes estimate GFR. Using the PICO terminology, the overall aim can be represented as: P Population Large patient groups who had undergone GFR measurements I Index test Estimated GFR based creatinine, cystatin C or equation combing the two analytes. C Reference test (Control) Renal clearance of inulin or another accepted clearance method according to Chapter 3.1. O Outcome Systematic error (bias), accuracy and classification ability. Specific questions 1. Which creatinine equation yields the most accurate estimate of GFR in large groups of adult and child patients? 2. Do cystatin C equations yield more accurate estimates of GFR than equations based on creatinine? 3. Do equations combining creatinine and cystatin C yield more accurate estimates than equations based on the individual markers separately? 4. How accurately is GFR estimated in subgroups divided according to kidney function, age, sex, ethnicity, and BMI? 5. How accurately is GFR estimated in populations that differ ethnically from the Swedish? 5(16) Inclusion criteria Population Large groups of patients (adults and children), patients with chronic kidney disease, kidney donors before and after donation, general populations and elderly who all had undergone GFR measurements Studies with at least 100 individuals or GFR measurements or at least 20 individuals or GFR measurements in subgroups, e.g. elderly and children Comparisons between creatinine and cystatin C equations and equations combining the two analytes including stratification for kidney function, age, gender and BMI limited to Caucasians Index test GFR estimating equations based on creatinine, cystatin C or combinations of the analytes Creatinine assays used in development and validation should be traceable to isotope dilution mass spectrometry (IDMS) or calibrated against the method used at the laboratory (Cleveland Clinic) where the original four-variable MDRD equation (MDRD-original) was developed. Roche creatinine assays (Jaffe and enzymatic) are IDMS-traceable from year 2002 according to the company and has been accepted for inclusion. o For MDRD-original results are only accepted if the creatinine assays were calibrated against the method used at Cleveland Clinic o For MDRD-IDMS results are only accepted if the creatinine assays were IDMS-traceable o Cockcroft-Gaults equation for adults and Schwartz original equation for children, both from 1976, were included since they are still used in clinical routine, though they are not based on today’s creatinine assays Cystatin C equations were accepted for analysis only if the cystatin C assay was analyzed at the same laboratory where the equation was developed due to lack of an international standard. This implies that only results of internal validation (for definition see below) will be available. Studies of cystatin C equations were included only if there were comparisons with creatinine based equations or equations combining creatinine and cystatin C In comparative studies of creatinine and cystatin C equations, non-standardized creatinine assays are accepted if the same laboratory and assay has been used for development and validation The time between the index (creatinine or cystatin C) and reference test (clearance measurement) should have been performed within 24 hours 6(16) Reference test Renal clearance of inulin or other external clearance markers with sufficient accuracy (renal clearance of iothalamate, iohexol, DTPA or 51Cr-EDTA, or plasma clearance of inulin, iohexol or 51Cr-EDTA); see Table 1 in English summary or reference [14] Outcome Bias (systematic error) and accuracy (incorporates both bias and precision) in terms of percentage of GFR estimates within 30% of measured GFR (P30) and classification ability of different stages of chronic kidney disease Exclusion criteria Population Specific disease groups. However, results concerning diabetes and organ transplants were included if they were reported separately in studies of large groups of patients. Patients undergoing dialysis treatment For question 1-4 above only studies of populations that ethnically resemble a Swedish population were included. For question 5 studies from all over the world were taken into account. Index test GFR equations based on other biomarkers than creatinine and cystatin C GFR equations based on bioimpedance for evaluation of lean body mass Nomograms to estimate GFR Creatinine assays where traceability is unclear or not described Studies based on inhibition of tubular secretion of creatinine based on cimetidine Studies on intra-individual variations, variation over time and reproducibility in estimated GFR GFR equations ability to predict changes in renal function over time, morbidity, mortality or other outcomes Reference test Not accepted reference test according to Chapter 3.1. (i.e. plasma clearance of iothalamate and DTPA, and endogenous creatinine clearance); see Table 1 in English summary or reference [14] 7(16) Outcome Systematic errors and accuracy only presented in diagrams Classification ability based ROC-area without presentation of correctly classified estimated GFR Development validations, i.e. results based on the same cohort of patients without separation in a development and test cohort Quality assessment of included studies The quality assessment of included studies was based on three different aspects: 1) type of validation (see next paragraph), 2) number of measurements, 3) study quality according to a modified QUADAS template with 11 items (Quality Assessment of Diagnostic Accuracy Studies) [15, 16]. The quality was classified as high, moderate or low according to the following criteria: High quality External validation of at least 500 clearance measurements (≥ 100 measurements in subgroups) and at least seven out of eleven quality points. Moderate quality At least 100 clearance measurements (≥ 40 measurements in subgroups) and at least four out of eleven quality points. Low quality Studies that does not fulfil the criteria of moderate or high quality. Requirements of bias and accuracy Bias was considered acceptable if it was less than 10% in mean or median [17]. Accuracy was regarded sufficient if at least 75% of the GFR estimates were within 30% of measured GFR (P30) according to National Kidney Foundation [18]. To be regarded as statistically certain, the lower 95% confidence limit of P30 should be ≥75%. Definition of validations Study quality depends on characteristics of the validation procedure. External validation has the highest quality followed by internal validation. Development validation has the lowest quality. External validation Validation performed in a different population and at a different laboratory than where the equation was developed. The validation is not regarded as external if its results are allowed to influence the final functional form or coefficients, or which one of alternative equations that is advocated. 8(16) Internal validation The expression of the equation and its coefficients is determined from a subset of a certain population (development cohort) and then tested in another subset of the same population (validation cohort). A validation performed in a different population than that used to develop the equation but at the same laboratory is also regarded as internal. In an internal validation the results are allowed to affect the final expression of the equation and which one of alternative equations that is advocated. Development validation Validation results presented for the same cohort that was used to develop the final expression of the equation and its coefficients. 9(16) Supplementary Figures and Tables based on the SBU systematic review Figure S1. Comparison performed by Equalis AB (External quality assessment for clinical laboratory investigations, www.equalis.se/en) of reported plasma concentrations of creatinine in µmol/L (Y-axis) between about 100 Swedish laboratories from 2003 to 2011 (year-week on the Xaxis) using a certified creatinine sample (71 µmol/L, 95% confidence interval 69.6 - 71.5 µmol/L). Median value, 1st and 3rd quartile (box plot), 5% and 95% percentiles, and maximum and minimum values (+) are illustrated. Dotted lines indicate the certified creatinine concentration. During the same time interlaboratory variation coefficient from measurements of the certified creatinine sample decreased from 10% to 5%. Adapted from Figure 1.5 in reference [19]. Permission granted for publication from the Swedish Council on Health Technology Assessment. 10(16) Figure S2. Estimated GFR (eGFR) in mL/min/1.73 m2 (Y-axis) based on MDRD, CKD-EPI and the original (LM-original) and revised Lund-Malmö (LM-revised) equations at a plasma creatinine concentration of 80 µmol/L in girls and females 1-30 years of age. eGFR based on the LM equations decreases with decreasing age at a given creatinine level, which reflects decreasing renal function when muscle mass (creatinine production) also decreases at the same time. On the other hand, MDRD and CKD-EPI will markedly overestimate GFR in children. The markedly different performance of the LM equations vs. MDRD and CKD-EPI may be attributed to the noticeable difference in the age coefficients [20]. Adapted from Figure 3.2.16 in reference [19]. Permission granted for publication from the Swedish Council on Health Technology Assessment. MDRD CKD-EPI LM-original LM-revised (GFR (mL/min/1.73 m2) 150 120 90 60 30 0 1 5 10 15 18 Age (years) 20 30 40 11(16) Table S1. Meta-analysis of creatinine based equations in children regarding P30 accuracy (95% confidence intervals), i.e. percent of GFR estimates within 30% of measured GFR. Adapted from Table 3.2.10. based on studies with details given in Table 3.2.29 (English text) in reference [19]. Comparisons Type of validation Number SchwartzIDMS vs. Schwartz original External in the same cohorts [20, 21] 337 SchwartzIDMS 80 (76-84) SchwartzIDMS vs. LM-original External and internal in the same cohorts [20, 22] 267 58 (53-64) SchwartzIDMS External [20-24] 700 74 (70-77) Schwartzoriginal 24 (19-28) SchwartzExternal and internal 807 74 (71-77) IDMS [9, 20-23, 25] Schwartz-IDMS = Schwartz equation based on IDMS traceable creatinine assays. Schwartz original = the original Schwartz equation [26]. LM-original = the original Lund-Malmö equation [4]. LM-original 69 (63-74) 12(16) Table S2. Meta-analysis of creatinine based equations in adults regarding P30 accuracy (95% confidence intervals), i.e. percent of GFR estimates within 30% of measured GFR. Results are based on pair wise comparisons and adapted from Table 3.2.4. which in turn is based on studies with details given in Table 3.2.17 (English text) in reference [19]. Comparisons Type of validation Number CG MDRD CG/MDRD External [4, 27-29] 3 267 75 (74-77) 85 (83-86) CG/MDRD External (CG) Extern and internal (MDRD) [4, 27-30] 8 771 71(70-72) 84(83-85) CKD-EPI/ MDRD External [28, 31, 32] 7 485 78 (77-79) 79(78-80) CKD-EPI/ MDRD External and internal [8, 28, 31-33] 14 131 80 (79-80) 81(80-82) External [31] 1 397 80 (77-82) 79 (77-81) MDRD/CKD-EPI/ LM CG = Cockcroft-Gault equation normalized to 1.73 m2 body surface area MDRD = Modification of Diet in Renal Disease Study equation CKD-EPI = Chronic Kidney Disease Epidemiology Collaboration equation LM = Lund-Malmö equation CKD-EPI LMoriginal/ reviderad 82 (80-84)/ 84(82-86) 13(16) Table S3. Meta-analysis of the best performing cystatin C and creatinine equation in each study as well as equations combining the two analytes in adults regarding P30 accuracy (95% confidence intervals), i.e. percent of GFR estimates within 30% of measured GFR. Results are based on pair wise comparisons and adapted from Table 3.2.9. which in turn is based on studies with details given in Table 3.2.28 (English text) in reference [19]. Type of validation Cystatin C equation Creatinine equations 83 (80-86) (n=760) Arithmetic mean equation* Composite equation** 83 (80-85) (n=760) 83 (80-86) (n=760) 89 (86-91) (n=760) 90 (87-93) (n=438) 89 (88-91) (n=1617) 89 (88-90) (n=4713) External [29, 34] External and internal [29, 34] External, internal and 82 (81-83) 84 (83-85) developmental [29, 34, 35] (n=5035) (n=5035) *Arithmetic mean of one cystatin C and one creatinine equation. **Single equation based on both cystatin C and creatinine. 14(16) References 1. Grubb A, Blirup-Jensen S, Lindstrom V, Schmidt C, Althaus H, Zegers I (2010) First certified reference material for cystatin C in human serum ERM-DA471/IFCC. Clin Chem Lab Med 48:1619-1621 2. DuBois D, DuBois E (1916) A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med 17:863-871 3. Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31-41 4. Nyman U, Björk J, Sterner G, et al. (2006) Standardization of p-creatinine assays and use of lean body mass allow improved prediction of calculated glomerular filtration rate in adults: a new equation. Scand J Clin Lab Invest 66:451-468 5. Hallynck TH, Soep HH, Thomis JA, Boelaert J, Daneels R, Dettli L (1981) Should clearance be normalised to body surface or to lean body mass? Br J Clin Pharmacol 11:523526 6. Björk J, Grubb A, Sterner G, Nyman U (2011) Revised equations for estimating glomerular filtration rate based on the Lund-Malmö Study cohort. Scand J Clin Lab Invest 71:232-239 7. Levey AS, Coresh J, Greene T, et al. (2006) Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 145:247-254 8. Levey AS, Stevens LA, Schmid CH, et al. (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604-612 9. Schwartz GJ, Munoz A, Schneider MF, et al. (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629-637 10. Gao A, Cachat F, Faouzi M, et al. (2013) Comparison of the glomerular filtration rate in children by the new revised Schwartz formula and a new generalized formula. Kidney Int 83:524-530 11. Grubb A, Horio M, Hansson LO, et al. (2014) Generation of a New Cystatin C-Based Estimating Equation for Glomerular Filtration Rate by Use of 7 Assays Standardized to the International Calibrator. Clin Chem 60:974-986 12. Inker LA, Schmid CH, Tighiouart H, et al. (2012) Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med 367:20-29 13. Chehade H, Cachat F, Jannot AS, et al. (2014) New combined serum creatinine and cystatin C quadratic formula for GFR assessment in children. Clin J Am Soc Nephrol 9:54-63 15(16) 14. Soveri I, Berg UB, Björk J, et al. (2014) Measuring GFR: A Systematic Review. Am J Kidney Dis 64:411-424 15. Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J (2003) The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 3:25 16. Whiting PF, Weswood ME, Rutjes AW, Reitsma JB, Bossuyt PN, Kleijnen J (2006) Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol 6:9 17. Spinler SA, Nawarskas JJ, Boyce EG, Connors JE, Charland SL, Goldfarb S (1998) Predictive performance of ten equations for estimating creatinine clearance in cardiac patients. Iohexol Cooperative Study Group. Ann Pharmacother 32:1275-1283 18. National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Part 5. Evaluation of laboratory measurements for clinical assessment of kidney disease. Guideline 4. Estimation of GFR. Am J Kidney Dis 39:S76-S92 19. Swedish Council on Health Technology Assessment (2012). Methods to estimate and measure renal function (glomerulär filtration rate). A systematic review. SBU Report 214. Available at http://www.sbu.se/214. Accessed March 1, 2015. 20. Nyman U, Björk J, Lindström V, Grubb A (2008) The Lund-Malmö creatinine-based glomerular filtration rate prediction equation for adults also performs well in children. Scand J Clin Lab Invest 68:568-576 21. Bacchetta J, Cochat P, Rognant N, Ranchin B, Hadj-Aissa A, Dubourg L (2011) Which creatinine and cystatin C equations can be reliably used in children? Clin J Am Soc Nephrol 6:552-560 22. Pottel H, Mottaghy FM, Zaman Z, Martens F (2010) On the relationship between glomerular filtration rate and serum creatinine in children. Pediatr Nephrol 25:927-934 23. Berg UB, Back R, Celsi G, et al. (2011) Comparison of plasma clearance of iohexol and urinary clearance of inulin for measurement of GFR in children. Am J Kidney Dis 57:55-61 24. Blufpand HN, Tromp J, Abbink FC, et al. (2011) Cystatin C more accurately detects mildly impaired renal function than creatinine in children receiving treatment for malignancy. Pediatr Blood Cancer 57:262-267 25. Andersen TB, Jodal L, Boegsted M, et al. (2012) GFR prediction from cystatin C and creatinine in children: effect of including body cell mass. Am J Kidney Dis 59:50-57 16(16) 26. Schwartz GJ, Haycock GB, Edelmann CM, Jr., Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259-263 27. Froissart M, Rossert J, Jacquot C, Paillard M, Houillier P (2005) Predictive performance of the modification of diet in renal disease and Cockcroft-Gault equations for estimating renal function. J Am Soc Nephrol 16:763-773 28. Nyman U, Grubb A, Sterner G, Björk J (2011) The CKD-EPI and MDRD equations to estimate GFR. Validation in the Swedish Lund-Malmö Study cohort. Scand J Clin Lab Invest 71:129-138 29. Tidman M, Sjöström P, Jones I (2008) A Comparison of GFR estimating formulae based upon s-cystatin C and s-creatinine and a combination of the two. Nephrol Dial Transplant 23:154-160 30. Stevens LA, Manzi J, Levey AS, et al. (2007) Impact of creatinine calibration on performance of GFR estimating equations in a pooled individual patient database. Am J Kidney Dis 50:21-35 31. Björk J, Jones I, Nyman U, Sjöström P (2012) Validation of the Lund-Malmö, Chronic Kidney Disease Epidemiology (CKD-EPI) and Modification of Diet in Renal Disease (MDRD) equations to estimate glomerular filtration rate in a large Swedish clinical population. Scand J Urol Nephrol 46:212-222 32. Murata K, Baumann NA, Saenger AK, Larson TS, Rule AD, Lieske JC (2011) Relative performance of the MDRD and CKD-EPI equations for estimating glomerular filtration rate among patients with varied clinical presentations. Clin J Am Soc Nephrol 6:1963-1972 33. Stevens LA, Schmid CH, Greene T, et al. (2010) Comparative performance of the CKD Epidemiology Collaboration (CKD-EPI) and the Modification of Diet in Renal Disease (MDRD) Study equations for estimating GFR levels above 60 mL/min/1.73 m2. Am J Kidney Dis 56:486-495 34. Stevens LA, Coresh J, Schmid CH, et al. (2008) Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis 51:395-406 35. Nyman U, Grubb A, Sterner G, Björk J (2009) Different equations to combine creatinine and cystatin C to predict GFR. Arithmetic mean of existing equations performs as well as complex combinations. Scand J Clin Lab Invest 69:619-627