12640798_Presentation - Geoff Shaw - ver 3.7.pptx (9.445Mb)
advertisement

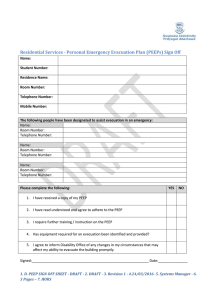
Optimal PEEP – the final solution (Model-Based Mechanical Ventilation for Intensive Care) Geoffrey M Shaw1 J.Geoffrey Chase2 Chiew Yeong Shiong2 Nor Salwa Damanhuri2 Erwin van Drunen2 1Intensive Care, Christchurch Hospital, New Zealand 2Mechanical Engineering, University of Canterbury, New Zealand Department of Intensive Care Melbourne Christchurch Department of Intensive Care Universities of Canterbury, Otago, and Christchurch Hospital Department of Intensive Care Presentation Outline • Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS) in Intensive Care Unit (ICU) • Treatment for ALI and ARDS (Mechanical Ventilation) • Model-Based Mechanical Ventilation – Minimal Model – Elastance Model • Results and Discussion • Conclusion and Future Work Department of Intensive Care Acute Respiratory Distress Syndrome • A syndrome of acute onset of respiratory failure with findings of bilateral infiltrates on chest radiograph, a partial pressure of arterial oxygen to fraction of inspired oxygen ratio (PaO2/FiO2) less than 300 (ARDS if less than 200mmHg) and the absence of elevated left heart filling pressure determined either diagnostically with a pulmonary artery catheter (pulmonary artery occlusion pressure of < 18mmHg) or clinically (absences of evidence of left arterial hypertension) • 1.3 to 22 per 100,000 (ALI: 17.9 to 34 per 100,000) • Mortality is up to 70% Ware et al. (2000). The acute respiratory distress syndrome Gattinoni, L. & Pesenti, A. (2005). The concept of "baby lung“ Ferguson, N. D. et al(2005). Airway pressures, tidal volumes, and mortality in patients with acute respiratory distress syndrome. Department of Intensive Care Treatment for ALI/ ARDS Department of Intensive Care Model-based Mechanical ventilation • Mechanical ventilation (MV) is the primary form of support for ALI/ARDS patients • However, due to intra- and inter- patient-variability reduce the efficacy of general protocols • Computer modelling can be used to identify and characterise patient-specific pulmonary mechanics and guide clinical decisions • 2 Model-based Methods – Minimal Model – Lung Elastance Monitoring Department of Intensive Care Model-based Mechanical Ventilation Part 1 A Minimal Model of Lung Mechanics Department of Intensive Care Minimal Model – Recruitment • Traditional Theory – Isotropic Balloon like expansion followed by overstretching • Recruitment Theory – Alveoli open or collapse – Recruitment continues throughout the cycle – Once recruited – no significant volume change Department of Intensive Care Minimal Model – Recruitment Alveoli do not behave like balloons Department of Intensive Care Threshold Opening Pressure/ Threshold Closing Pressure • Threshold Opening Pressure (TOP) – Clinical Pressure when Alveoli Opens • Threshold Closing Pressure (TCP) – Clinical Pressure when Alveoli Collapse • TOP > TCP Crotti, et al. (2001). Recruitment and derecruitment during acute respiratory failure: a clinical study Department of Intensive Care Minimal Model Development • Based on the following Concepts: – Lung is modelled as a collection of lung units – Either Recruited or Collapsed – The state of every unit is governed by TOP and TCP – The TOP and TCP for every lung unit assumed normally distributed. *allowing fitting of a Gaussian Distribution Curve: Mean and Standard Deviation Original data sourced form: BERSTEN, A. D. 1998. Measurement of overinflation by multiple linear regression analysis in patients with acute lung injury. Eur Respir J, 12, 526-532. Department of Intensive Care Model Basics Mean Threshold Opening Pressure Department of Intensive Care Standard Deviation of the distribution Clinical Model Validation • MEAN FITTING ERROR – – • • 1.62% - Inflation 4.42% - Deflation Capable of capturing patients fundamental lung mechanic Model TOP, TCP and SD Original data sourced form: BERSTEN, A. D. 1998. Measurement of overinflation by multiple linear regression analysis in patients with acute lung injury. Eur Respir J, 12, 526-532. Department of Intensive Care Model - Application • PEEP selection based on TOP and TCP concept – TOP – How much pressure required to open the Lung units – TCP – Maintain Recruitment • Can this give us insight about the disease process? Department of Intensive Care Change in TOP or SD • Monitor the Change of TOP or Standard Deviation • Potential to group Patients based on TOP and SD information Department of Intensive Care Disease State Grouping (DSG) How does the lung recover? ALI ARDS Normal H1N1 How does lung injury progress? • • • A metric to classify patients disease state. Potential to guide MV treatment based on patient’s condition Theoretical – Warrant investigation on TOP and SD relation with known patient’s disease state Department of Intensive Care Disease State Grouping (DSG) E.g. “Bad cold” vs Bird/Swine flu Department of Intensive Care Possible Examples in DSG H1N1 Healthy Beginning of ALI Department of Intensive Care ARDS Example - Clinical • Case Study 1 – 59y Male (survived) – Pneumonia, COPD • Day 0 (PEEP = 12cmH2O) – – – – Auto PEEP = 14cmH2O PaO2 = 114 FiO2 = 0.4 Average Mean TOP = 45cmH2O • Day 3 (PEEP = 12cmH2O) – – – – Auto PEEP = 8cmH2O PaO2 = 80 FiO2 = 0.4 No significant changes in Standard deviation - The lung state remains unchanged. – Mean TOP drop with time – The patients lung became less stiff compared to earlier. Department of Intensive Care SUNDARESAN, A., CHASE, J., SHAW, G., CHIEW, Y. S. & DESAIVE, T. 2011. Model-based optimal PEEP in mechanically ventilated ARDS patients in the Intensive Care Unit. BioMedical Engineering OnLine, 10, 64. • Case Study 2 – 69y Male (Deceased) – Intra-abdominal sepsis • Day 0 (PEEP = 15cmH2O) – Auto PEEP = 11cmH2O – PaO2 = 126 – FiO2 = 0.7 • Day 7 (PEEP = 12.5cmH2O) – Auto PEEP = 2.3cmH2O – PaO2 = 98 – FiO2 = 0.35 • Day 14 (PEEP =10cmH2O) * – – – – – Auto PEEP = 1.6cmH2O PaO2 = 93 FiO2 = 0.4 TOP drops Lung is less stiff But SD increases meaning more lung (alveoli) are injured. Department of Intensive Care SUNDARESAN, A., CHASE, J., SHAW, G., CHIEW, Y. S. & DESAIVE, T. 2011. Model-based optimal PEEP in mechanically ventilated ARDS patients in the Intensive Care Unit. BioMedical Engineering OnLine, 10, 64. Model-based Mechanical Ventilation Part 2 Continuously Monitoring Lung Elastance to Guide Mechanical Ventilation PEEP Department of Intensive Care Lung Elastance Monitoring Respiratory System Equation of Motion V(t) Paw = Ers.V + Rrs.Q + P0 • • • • • • Paw Ers V Rrs Q P0 - Airway Pressure Respiratory Elastance Volume Airway Resistance Flow Offset Pressure (PEEP) BATES, J. H. T. 2009. Lung Mechanics: An Inverse Modelling Approach, Cambridge University Press. Department of Intensive Care Ers P(t) Rrs Q(t) What if... Respiratory System Elastance changes with Time during each volume increase? Paw (t) = Edrs (t).V(t) +Rrs.Q(t) + P0 Can we capture the lung condition with time? • • • Continuous Monitoring of Lung Elastance/ Dynamic Lung Elastance and Resistance Integral Based Method (Similar to Multiple Linear regression) Monitoring the Elastance Trend may provide an opportunity to optimise PEEP SUAREZ-SIPMANN, F., BOHM, S. H., TUSMAN, G., PESCH, T., THAMM, O., REISSMANN, H., RESKE, A., MAGNUSSON, A. & HEDENSTIERNA, G. 2007. Use of dynamic compliance for open lung positive end-expiratory pressure titration in an experimental study. Crit Care Med, 35, 214 - 221. CARVALHO, A., JANDRE, F., PINO, A., BOZZA, F., SALLUH, J., RODRIGUES, R., ASCOLI, F. & GIANNELLA-NETO, A. 2007. Positive end-expiratory pressure at minimal respiratory elastance represents the best compromise between mechanical stress and lung aeration in oleic acid induced lung injury. Critical Care, 11, R86. LAMBERMONT, B., GHUYSEN, A., JANSSEN, N., MORIMONT, P., HARTSTEIN, G., GERARD, P. & D'ORIO, V. 2008. Comparison of functional residual capacity and static compliance of the respiratory system during a positive end-expiratory pressure (PEEP) ramp procedure in an experimental model of acute respiratory distress syndrome. Critical Care, 12, R91. Department of Intensive Care Concept of Minimal Elastance • During each breathing cycle, as PEEP rises, respiratory elastance (Ers) may fall as new lung volume is recruited faster than pressure can build up in the lung. This indicates recruitability • If there is little or no recruitment, Ers rises with PEEP indicating that inspiratory pressure was unable to recruit significant new lung volume and now the pressure is, instead, beginning to stretch already recruited lung • Hence, recruitment and potential lung injury can be balanced by selecting PEEP at minimum Ers • Compared to a single, constant Ers value at each PEEP, identifying time-variant Edrs allows this change to be seen dynamically within each breath as pressure increases thus allowing a more detailed view of patient’s lung physiology. Department of Intensive Care Model-based Mechanical Ventilation Part 2 Clinical Trials for Proof of concept Department of Intensive Care Clinical Protocol • Patients underwent a protocol-based step-wise incremental PEEP recruitment manoeuvre (RM) using SIMV (Vt =500 ml) The ETT cuff pressure was inflated to ~60 cmH2O to ensure there was no leakage so changes in FRC could be measured • Baseline measurements were taken, then PEEP was decreased to ZEEP or reduced to a “safe” clinical level as determined by the PI) • During the RM, PEEP was increased using 5 cmH2O steps until peak airway pressure reached at least 45 cmH2O. Other settings were maintained throughout the RM. • Each PEEP level was maintained for 10~15 breaths until stabilisation before increasing to a higher PEEP level. Department of Intensive Care Patients Recruited in CHC Hospital • A total of 10 patients have been included in the 1st phase of the trial. (Still recruiting more) Patients Sex 1 2 3 4 5 6 7 8 9 10 F M M M M M M F M M Age (year) 61 22 55 88 59 69 56 54 37 56 Clinical Diagnostic Peritonitis, COPD Trauma Aspiration Pneumonia, COPD Pneumonia, COPD, CHF Intra-abdominal sepsis, MOF Legionnaires Aspiration H1N1, COPD* Legionnaires, COPD* Department of Intensive Care P/F Ratio (mmHg) 209 170 223 165 285 280 265 303 193 237 FiO2 0.35 0.50 0.35 0.40 0.40 0.35 0.55 0.40 0.40 0.35 Patient 6 (Trauma) • • • • • As PEEP Increases, Respiratory System Elastance drop until minimal before rising Minimal Elastance (Maximum Compliance) was observed at PEEP 15cmH2O The inflection line is identified as +5~10 % above minimal Elastance. Selecting PEEP at Minimum Elastance (Maximum Compliance) is not a new concept. Relatively few clinical trials have been carried out. Department of Intensive Care Example – Variable PEEP with Respiratory System Elastance Pt 2: (Trauma) Pt 6: (Intra-abdominal sepsis, CHF) Minimal Elastance PEEP = 15cmH2O Minimal Elastance PEEP = 15cmH2O Inflection PEEP = 6~9cmH2O Inflection PEEP = 7.5~10cmH2O Pt 8: (Aspiration) Pt 10: (Legionnaires, COPD) Minimal Elastance PEEP = 25cmH2O Minimal Elastance PEEP = 20cmH2O Inflection PEEP = 12~18cmH2O Inflection PEEP = 12~15cmH2O Department of Intensive Care Patient 6 (Intra-abdominal sepsis, CHF) • • • • • Using Edrs with time, it is possible to identify the change of Respiratory Elastance within a breathing cycle A drop in Edrs will indicate the recruitment over pressure build up. An increase will suggest recruitment. The Respiratory system compliance within each breath can be monitored Edrs potentially provides higher resolution in monitoring the patients breathing condition compared to a single Elastance value within a breath Department of Intensive Care New Concept - Variable PEEP with Edrs Pt 2: (Trauma) Pt 6: (Trauma) Pt 8: (Aspiration) Pt 10: Legionnaires, COPD Department of Intensive Care Example: Monitoring Edrs with time Pressure and Edrs 40 30 20 10 0 10 15 20 25 Time (seconds) Measured Pressure (Blue Line) Model Pressure Fitting (Black Dots) Edrs within a breath (Red Line) What happens to Ers if PEEP Changes? Department of Intensive Care 30 Comparing Lower and Higher PEEP in a Patient • Pressure and Edrs 40 • 30 20 Ventilated at Lower PEEP Edrs within a breath drops, suggesting recruitment 10 0 10 15 20 25 30 Time (seconds) Pressure and Edrs 40 • 30 • 20 10 Ventilated at Higher PEEP Edrs within a breath increases, suggesting over distension 0 10 15 20 25 30 Time (seconds) BERSTEN, A. D. 1998. Measurement of overinflation by multiple linear regression analysis in patients with acute lung injury. Eur Respir J, 12, 526-532. Department of Intensive Care Animal Trials in Belgium • Animal Trials have been carried out to investigate the performance of the models. • Healthy anesthetised piglet was ventilated with fixed tidal volume using Engström CareStation (Datex, General Electric, Finland). • ARDS was induced using oleic acid. • Subject’s arterial blood gases were sampled to monitor the development of ARDS. • Elastance (Ers, Edrs), and resistance (Rrs) using integral based method Department of Intensive Care Use of Electrical Impedance Tomography to compare with our findings • Electric Impedance Tomography (Collaborations) Zhao, Z., D. Steinmann, et al. (2010). "PEEP titration guided by ventilation homogeneity: a feasibility study using electrical impedance tomography." Crit Care 14: R8. • Minimal Model Sundaresan, A., T. Yuta, et al. (2009). "A minimal model of lung mechanics and model-based markers for optimizing ventilator treatment in ARDS patients." Computer Methods and Programs in Biomedicine 95(2): 166-180. • Elastance Model Chiew, YS, Chase, JG, Shaw, GM, and Sundaresan, A and Desaive, T, Model-Based PEEP Optimization for Mechanically Ventilated ARDS Patients, BioMedical Engineering Online 2011. • Cross comparison and validation Department of Intensive Care Animal trial results (unpublished) Elastance 150 100 Integral Based Constant Elung Integral based Median Edrs Multiple Linear Regression Edrs Vent Dynamic Elastance Vent Static Elastance 50 0 20 40 60 80 100 120 140 160 180 Time (minutes) • • • • • Blue Line Black Line Green Line Red Line Pink Line inspiratory pause - Integral Based Constant Ers. - Integral Based Median Edrs. - Multiple Linear Regression Median Edrs. - Ventilator Dynamic Elastance (∆P/Vt). - Ventilator Static Elastance ((Pend insp – P0)/Vt) – The ventilator has an allowing estimation of ‘Static Elastance’. *Blue, Black and Green Line Overlaps each other Computer Methods estimating Ers was able to reproduce the findings in ventilator. Change in Elastance was observed with the development of ARDS Department of Intensive Care 200 Conclusion and Future Work • The initial clinical trials indicate that the minimal model and respiratory elastance monitoring may be able to assist in the clinical decision for optimizing MV – Minimal Model – There is insufficient clinical data to determined the Disease Sate Groups. (What value is high TOP/SD?) – Minimal Elastance Selection – Proof of concept that warrants further investigation • More trials to validate the performance of the model – ARDS Animal model – University of liege, Belgium (June 2012) – Clinical trials open for recruitment (On going) • Bedside and real time application (In progress) – Tablet +Software and Ventilator interface development Department of Intensive Care Research Collaborations? • Main Collaboration on MV Research – – – • Other Collaborations – – – – • Cardiovascular Research Center, University of Liege, Liege, Belgium Intensive Care Unit, CHU Sart-Tilman, Liege, Belgium Institute for Technical Medicine, Furtwangen University, Germany Intensive care and burn unit, University Hospital of Lausanne, Lausanne, Switzerland St-Luc University Hospital, Intensive care unit, Brussels, Belgium Intensive Care Unit, Clinique Notre Dame de Grâce, Gosselies, Belgium Intensive care unit, University Hospital of Geneva, Geneva, Switzerland Prospective Collaborations? Department of Intensive Care Department of Intensive Care Thank you! Department of Intensive Care Supplementary material Department of Intensive Care Identifying Ers, Rrs and Edrs • Multiple Linear Regression (MLR) – Solving a Matrix • Integral Based Method - Similar to MLR – Instead of using data points of a curve, it uses the area under the curve – More information and more robust to noise • Paw = Ers.V + Rrs.Q + P0 – We can identify Ers, and Rrs • Using this Ers and Rrs from previous Equation • Paw (t) = Edrs (t).V(t) +Rrs.Q(t) + P0 can be solved. Department of Intensive Care Publications • Sundaresan, A., T. Yuta, et al. (2009). "A minimal model of lung mechanics and model-based markers for optimizing ventilator treatment in ARDS patients." Computer Methods and Programs in Biomedicine 95(2): 166-180. • Chiew, YS, Chase, JG, Shaw, GM, and Sundaresan, A and Desaive, T, ModelBased PEEP Optimization for Mechanically Ventilated ARDS Patients, BioMedical Engineering Online 2011. • Sundaresan, A., J. Geoffrey Chase, et al. (2011). "Dynamic functional residual capacity can be estimated using a stress-strain approach." Computer Methods and Programs in Biomedicine 101(2): 135-143. • Sundaresan, A, Chase, JG, Shaw, GM, Chiew, YS and Desaive, T, ModelBased Optimal PEEP in Mechanically Ventilated ARDS Patients in the Intensive Care Unit, BioMedical Engineering Online 2011, 10:64. • Chiew, YS, Desaive, T, Lambermont, B, Janssen, N, Shaw, GM, Schranz, C, Moeller, K and Chase, JG (2012), “Physiological relevance of a minimal model in Healthy Pigs Lung”, 8th IFAC Symposium on Biological and Medical Systems, Budapest, Hungary. (In-Review) (Invited Paper) Department of Intensive Care Publications • Mishra, A, Chiew, YS, Shaw, GM, and Chase, JG (2012), “Model-Based Approach to Estimate dFRC in the ICU Using Measured Lung Dynamics”, 8th IFAC Symposium on Biological and Medical Systems, Budapest, Hungary. (In-Review) • Chiew, YS, Desaive, T, Lambermont, B, Janssen, N, Shaw GM and Chase, JG (2012), “Performance of lung recruitment model in healthy anesthetized pigs”, 2012 World Congress of Medical Physics and Biomedical Engineering, Beijing, China, May 26-31, 1-page. (Accepted) • Chiew, YS, Chase, JG, Shaw, GM and Desaive T (2012), “Respiratory system elastance monitoring during PEEP titration”, 32th International Symposium of Intensive Care and Emergency Medicine (ISICEM), Brussels, Belgium, March 20-23, 1-page. (Poster Presentation) • Sundaresan, A., Shaw, G. M., Chiew, Y.S. and Chase, J.G., PEEP in mechanically ventilated patients: a clinical proof of concept, AustraliaNew Zealand Intensive Care Society (ANZICS) ASM, Taupo, New Zealand, March 31 – April 1, 1-page, (2011). Department of Intensive Care