12601189_Main.doc (701.5Kb)
advertisement

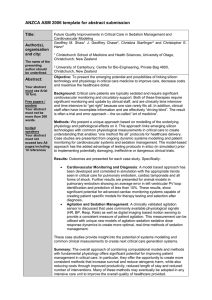
Page 1 of 32 Physiological Modelling of Agitation-Sedation Dynamics Including Endogenous Agitation Reduction A. D. Rudge1, J. G. Chase1, G. M. Shaw2, D. Lee3 1 Centre for Bioengineering, Department of Mechanical Engineering, University of Canterbury, Christchurch, New Zealand 2 Department of Intensive Care Medicine, Christchurch Hospital, Christchurch, New Zealand, University of Otago School of Medicine and Health Sciences 3 Centre for Bioengineering, Department of Mathematics and Statistics, University of Canterbury, Christchurch, New Zealand Centre for Bioengineering Department of Mechanical Engineering University of Canterbury Private Bag 4800 Christchurch New Zealand Correspondence to Andrew Rudge Email: a.rudge@mech.canterbury.ac.nz Telephone: +64 21 147 5582 Fax: +64 3 364-2078 Page 2 of 32 ABSTRACT Sedation administration and agitation management are fundamental activities in any intensive care unit. A lack of objective measures of agitation and sedation, as well as poor understanding of the underlying dynamics, contribute to inefficient outcomes and expensive healthcare. Recent models of agitation-sedation pharmacodynamics have enhanced understanding of the underlying dynamics and enable development of advanced protocols for semi-automated sedation administration. However, these initial models do not capture all observed dynamics, particularly periods of low sedative infusion. A physiologicallyrepresentative model that incorporates endogenous agitation reduction (EAR) dynamics is presented and validated using data from 37 critical care patients. High median Relative Average Normalised Density (RAND) values of 0.77 and 0.78 support and minimum RAND values of 0.51 and 0.55 for models without and with EAR dynamics respectively show that both models are valid representations of the fundamental agitation-sedation dynamics present in a broad spectrum of ICU patients. While the addition of the EAR dynamic increases the ability of the model to capture the observed dynamics of the agitation-sedation system, the improvement is relatively small and the sensitivity of the model to the EAR dynamic is low. Although this may represent a limitation of the model, the inclusion of EAR is shown to be important for accurately capturing periods of low, or no, sedative infusion, such as during weaning prior to extubation. Keywords Physiological models, Non-linear dynamics, Dynamic modelling, Agitation, Sedation Page 3 of 32 1.0 INTRODUCTION Effective delivery of sedation in the intensive care unit (ICU) is fundamental to providing comfort and relief to the critically ill. A Midazolam and Morphine combination, given by intermittent bolus or infusion, is the mainstay of most ICU regimens [1]. Midazolam is a sedative agent used to induce a state of conscious sedation, and Morphine is a powerful opioid analgesic with additional mild sedative effects. Insufficient sedation exacerbates anxiety and agitation, and increases the risk of selfextubation. Over-sedation is a common outcome, and is damaging to patient health, and increases length of stay and cost [2]. While sedation is administered to maintain patient comfort, most sedation in the ICU is administered in response to patient agitation [3]. Hence, the target, or control, metric for regulating sedation in critical care is minimal agitation, rather than a given level of consciousness. Several recent studies have highlighted the cost and healthcare benefits of drug delivery protocols based upon agitation-sedation assessment scales [4-6]. Very simple sedation control protocols aimed at minimizing over-sedation have reduced length of stay 28–35%, total drug requirements 46–57%, and testing for altered mental status 67% [2, 7]. Therefore, controlling agitation without over-sedation offers significant potential. The key to achieving such control is accurate models that include all fundamental clearance pharmacodynamic behaviours. Agitation-sedation cycling describes oscillations between states of agitation and over-sedation often observed in critically ill patients. The underlying non-linear dynamics of the agitationsedation cycle are not well understood and many complex interactions contribute to observed patient behaviour. Therapeutic treatment methods rely heavily upon the experience and intuition of the medical staff, introducing variability and inconsistency. Computerized sedative infusion protocols that enable consistency of care and minimize fluctuations in Page 4 of 32 treatment could therefore improve patient care, simplify administration, minimize drug consumption and staff effort, and reduce costs. In spite of these advantages, current computer assisted infusion systems utilising feedback control in the ICU are still in their infancy [8-10]. Target Controlled Infusion (TCI) systems deliver drugs to maintain target plasma concentrations, using a pharmacokinetic model. This approach is well suited to anaesthesia where short periods of reduced consciousness and wellknown pharmacology are common. However, infusion systems that regulate the infusion rate to maintain target agitation levels, thus regulating the primary metric for long-term sedation, are the goal for improving care in the ICU. Although conscious sedation in the ICU utilises hypnotic drugs similar to those used in Total Intra-Venous Anaesthesia (TIVA), the drug dose and consciousness levels are distinctly different, as are the patients and the environment. More importantly, the overall goal of the therapy is significantly different. Anaesthesia applications aim to induce reduced consciousness for short periods. However ICU sedation seeks to simultaneously minimise both agitation and over-sedation over long periods of time. Hence, critical care sedation management is a very different problem that seeks the best trade-off between sedative dose and patient agitation. Therefore, while similarities between the two fields may provide insight, the differences prevent simple application of anaesthesia delivery methods, measurements and protocols to long-term ICU sedation administration. The primary limitations to the development of optimized sedative infusion protocols are the lack of an objective, physiologically-based, quantified agitation scale and limited understanding of the underlying system dynamics. The subjective measures of agitation currently employed introduce significant variability between assessors and inconsistency of care [5, 11]. While no gold-standard agitation-sedation scale exists, the Riker Sedation Agitation Scale (SAS) is widely accepted [12]. Quantitative agitation sensors being developed Page 5 of 32 [13-16], offer the potential to significantly improve agitation management when coupled with dynamic models and control protocols [17]. This research further develops the physiologically-based models required to develop agitation feedback protocols for medical decision support systems and eventually automated sedation administration. Previous attempts to improve agitation management in the ICU have been limited to clinical trials employing fixed sedative protocols using subjective agitation assessments [2, 4, 7, 18]. The use of quantitative modelling to enhance understanding of the system and provide a simulation platform is a recently developed tool in this area [10, 17, 19]. Initial models [17, 20] were built upon a simple 2-compartment pharmacokinetic framework and treated the concomitant administration of Morphine and Midazolam as one drug for pharmacokinetic purposes. The assumption of a linear relationship between plasma drug concentration and drug effect led to underestimation of the patient’s sedative requirements at higher doses. More complex dynamics including separate pharmacokinetics, effect saturation and drug synergism were added upon further development of the model [21, 22]. It is proposed that time-varying parameters and the inclusion of an endogenous agitation reduction (EAR) dynamic may improve the fit of the agitation-sedation model with recorded data. This research incorporates these additional non-linear dynamics to create more physiologically representative models of the agitation-sedation system. These models are then statistically validated against prior work and clinical data to assess the importance of these additional dynamics. 2.0 METHOD 2.1 Physiological Modelling The model presented utilizes separate pharmacokinetic (PK) models for Midazolam and Morphine. Displayed schematically in Fig. 1, it is a closer representation of the actual physiological system than other works [17, 19, 20-22], and includes delayed distribution, drug Page 6 of 32 synergism, effect saturation and endogenous agitation reduction. The model is defined in three main portions: I. Pharmacokinetics of Morphine: Vco dCco o ( K CL K ceo K cpo )Cco P oU K eco Ceo K opcC op dt V po Veo dC op (1) K opcC op K cpo C co (2) dCeo K eco Ceo K ceo Cco dt (3) dt II. Pharmacokinetics of Midazolam: Vcs dCcs s ( K CL K ces )Ccs P sU K ecs Ces dt Ves dCes K ecs Ces K ces Ccs dt (4) (5) III. Pharmacodynamics of Morphine and Midazolam: t dA w1S w2 (t ) KT EComb ( )e KT ( t ) d w3 A dt 0 (6) where Cc, Cp and Ce are the drug concentrations (mg/L) in the central, peripheral and effect compartments, Vc, Vp and Ve are the distribution volumes (L) of the central, peripheral and effect compartments, U is the intravenous infusion rate (mL/min), A is an agitation index, S is the stimulus invoking agitation, Kij is the transfer rate (L/min) from compartment i to compartment j, KCL is the drug clearance (L/min), KT is the effect time constant (min-1), and Po and Ps are the proportions of Morphine (‘o’) and Midazolam (‘s’) per unit volume of solution respectively (mg/mL). Time is represented by t (min), is the variable of integration, and the terms w1 and w2(t) are the relative weighting coefficients between stimulus and sedative sensitivity. Similarly, w3 is the coefficient associated with the endogenous reduction of patient agitation, or agitation reduction without sedative. Finally, EComb is the combined pharmacodynamic effect of the individual effect site drug concentrations of Morphine and Page 7 of 32 Midazolam determined using response surface modelling as defined in Minto et al. [23] and o s detailed in the lower portion of Fig. 1. In Fig. 1 C50 and C50 represent the concentrations at which Morphine or Midazolam would have 50% effect if administered alone. This model is intended to be the simplest necessary to capture the essential dynamics of the agitation-sedation system, matching patient observations and published literature with a physiologically representative model. Equations (1)–(2) represent the pharmacokinetics (PK) of the infusion and distribution of Morphine, and Equation (3) represents transport of Morphine to the effect site. Similarly, Equation (4) represents the pharmacokinetics of the infusion and distribution of Midazolam, and Equation (5) represents transport of Midazolam to the effect site. The non-linear pharmacodynamic (PD) Equation (6) is based on physiological observations of patient behaviour, and simply states that the rate of change of agitation depends upon the relative magnitude of the stimulus to the cumulative sedative effect and endogenous agitation reduction. Stimulus in this context refers to the combined effect of inherent pain, distress, or loss of inhibition caused by the diseased/injured state of the patient, and the therapeutic and diagnostic procedures performed by medical staff [21]. 2.1.1 Pharmacokinetic (PK) Modelling Many pharmacological models exist for the delivery of Morphine or Midazolam independently. Typically, Morphine and Midazolam are administered as a fixed ratio solution. Hence, this paper utilizes separate compartmental PK equations for each drug, so the combined drug infusion rate results in accurate effect site concentrations. The central PK compartment in Fig. 1 represents the infusion site and local blood vessels, such as the heart and lungs. The peripheral compartment can be thought of as the peripheral parts of the body to which blood flows, such as the legs and arms, and incorporating the fatty tissues into which Page 8 of 32 these drugs and/or metabolites can be deposited. The effect site concentration is that region in which the drug exerts its primary effect. For drugs affecting the central nervous system, such as Morphine and Midazolam, the cerebro-spinal-fluid [24], or the brain [25, 26], is an acceptable representation of the effect site. Clinical trials investigating the PK of Morphine show that concentration profiles in healthy and ICU subjects are best approximated by a 3-compartment model [24, 27]. These studies attempt to model the PK of intravenous (I.V.) Morphine incorporating the effect of metabolites such as Morphine-3-glucuronide (M3G) and Morphine-6-glucuronide (M6G) by adding additional compartments. However, the analgesic and sedative effects of these metabolites are not easily quantified and the details of their pharmacological effect are not yet fully understood [25, 28, 29]. Further, metabolite concentrations have been shown to be small when administration techniques bypassing the first-pass effect are used, such as I.V. administration [28]. Therefore, this portion of the model uses three compartments and does not model the formation, distribution or secondary effect of Morphine metabolites. Clinical trials investigating the PK of I.V. Midazolam show that concentration profiles in healthy and ICU subjects are best approximated by a 2-compartment model [30-32]. While the activity of the major metabolite of Midazolam, alpha-hydroxy-midazolam (α-OH Midazolam) has received a lot of attention, the effect has not yet been fully defined [1, 3335]. Therefore, this portion of the model uses two compartments and does not model the formation, distribution or secondary effect of metabolites. The overall model defined in Equations (1)-(6) consists of several PK and PD components. The PK parameters form the basis for the drug distribution and elimination half-life, while the PD parameters define the shape of the response surface and drug sensitivities. It is commonly accepted that significant inter-patient variability is observed in the pharmacology of sedatives in the critically ill and elderly [6, 36]. However, studies have also shown that inter-patient Page 9 of 32 variability appears to be due primarily to variations in PD parameters, such as drug sensitivity, rather than PK parameters, such as drug clearance or volume of distribution [20, 37-39]. Therefore, identical PK parameters representative of a typical ICU patient were obtained from the literature [24, 27, 31, 32] and applied across all patients. 2.1.2 Pharmacodynamic (PD) Modelling Midazolam is a commonly used sedative agent that can be used to induce anaesthesia or induce conscious sedation, depending on selected dose [31, 36]. Morphine, while primarily an analgesic, is also a mild sedative [6, 40]. However, Morphine and Midazolam, administered concomitantly, synergistically have an overall combined effect greater than the simple sum of the two individual effects [41, 42]. Furthermore, the effects of Morphine and Midazolam are typically not linearly proportional to drug concentrations, and instead behave like the wellknown sigmoid concentration-effect relationship [23, 43, 44]. The combined PD effect of these drugs is modelled in Equation (6) using a response surface for drug interactions [23], incorporating synergism and effect saturation, as shown in Fig. 1. The sedative effect on the vertical axis lowers awareness, relieving anxiety and reducing agitation. Finally, Equation (6) captures the cumulative sedative effect of the drugs on the brain over time, and provides the relationship between stimulus invoking agitation and the sedative agents employed to manage agitation. The non-linear pharmacodynamic (PD) Equation (6) is based on physiological observations of patient behaviour. It states that the rate of change of agitation depends upon the relative magnitude of the stimulus to the cumulative sedative effect and endogenous agitation reduction. Observed agitation typically falls upon increased infusion of sedative agents. Similarly, patients become more agitated by increased stimulus if infusion rates are not increased. Patient agitation is therefore primarily reduced by the cumulative impact of current and prior sedation administration, as modelled by the convolution integral in Equation (6). Page 10 of 32 The final term in Equation (6) represents the effect of the endogenous opioid biochemical compounds, endorphins. Abbreviated from “endogenous morphine”, endorphins are a form of natural analgesic produced in response to pain and physical stress [45, 46]. An agitated patient may therefore experience a reduction in agitation due to the natural sedative effect of endorphins produced as result of agitation itself, modelled by the EAR term, -w3A, in Equation (6). This term is unique in comparison to prior works and represents a dynamic by which agitation can decline without the presence of exogenous sedative. Such a dynamic is a stabilising factor and would be significant during periods of low or no exogenous sedative input. o ,s PD parameters, such as w2(t), w3, and C50 , can vary widely between patients, and are fitted using recorded drug infusion profiles for each patient. The general shape of the PD response surface in Fig. 1 [23] is approximated by information in the literature [37, 38]. In particular, the response surface is defined to capture the synergistic sedative effects observed when Morphine and Midazolam are administered concomitantly [41, 42], the mild sedative effect of Morphine alone [6, 40], and saturation dynamics. C50 represents the concentration at which the drug, administered alone, would have 50% effect. Using the PK model parameters and employing the recorded infusion rate, Equations (1)-(5) yield Morphine and Midazolam effect-site concentration profiles. These profiles can be used to estimate a patient-specific C50 value, assuming that clinical effect site concentration rarely becomes completely saturated. Natural initial estimates for C50 would be either the average, or 50% of the maximum, effect-site drug concentration from Equations (3) and (5). However, the impact of the synergistic effect surface means that the total combined effect of the drugs is higher than the simple sum of the individual drug effects, more regularly Page 11 of 32 resulting in effect saturation. As a result, setting C50 to be 80% of the max effect site concentration provides an effective estimate. An integral-based fitting method is adapted from Hann et al [47], to obtain the patientspecific, time-varying, sedative sensitivity parameter, w2(t), and a patient-specific, timeinvariant w3 EAR parameter from clinical data. Initial studies investigating the sensitivity of the model to changes in w3 indicated that small changes (i.e. less than an order of magnitude) had no observed effect on performance metrics. Therefore, the EAR parameter, assumed to be patient-specific, is selected for each patient from an array of values w3=[0 0.00001 0.0001 0.001]. All remaining model parameters used in this paper are taken from previous work [17, 19-21]. 2.2 Model Verification Equations (1)–(6) are implemented in conjunction with a validated nurse sedation control model that accurately captures the basic nursing sedation administration response to patient agitation using a simple derivative-weighted Proportional-Derivative controller [17, 19]. This simple nurse controller captures the basic psychology behind subjective assessments [20, 48], and closes the feedback loop between clinically observed or simulated agitation and sedation delivery, matching current clinical practice. Comparison of recorded infusion data with infusion profiles from simulations using fitted parameters provides a basis for statistically validating the model presented. Infusion data were recorded using an electronic drug infusion device [10, 49] for all ICU patients admitted to the ICU during a nine month observation period and requiring more than 24 hours of sedation. Infusion data containing less than 48 hour of continuous data, or data from patients whose sedation requirements were extreme, such as those with severe head injuries, were excluded. A total of 37 ICU patients met these requirements and were enrolled in this study. Approval was obtained from the Canterbury Ethics Board for this research. Page 12 of 32 The unknown nature of pain and anxiety, combined with disease state, makes direct recording of stimulus profiles impossible. However, the input for the semi-automatic sedation infusion system implemented in the Christchurch ICU [10, 49] is the bedside medical staff’s indication of observed agitation, and therefore demand for additional drug. These recordings indicate times where the patient’s agitation level increased enough to warrant additional sedative, implying the presence of stimulus. It therefore forms the basis for a surrogate measure of stimulus for model validation [17]. The 4-hour moving average of this record retains the underlying structure of the recording, while creating a smooth stimulus profile congruent with recorded data. Note that clinical implementation of agitation feedback control of sedation would not require this input profile, requiring only measured agitation to determine the infusion needed. Hence, this is a model validation tool only. One approach to model verification uses kernel smoothing of the recorded data to create a probability band using Chebychev’s inequality, and compares the simulated infusion profile to the probability band [17]. The higher the percentage of time that the simulated infusion profile lies within the band, the better the model is considered to capture the essential dynamics of the underlying system for that patient. While this approach is graphically useful, it lacks an objective numerical measure of how close the simulated infusion profile is to the empirical data. The percentage time in band (TIB) does not serve this purpose because it simply quantifies visual closeness by means of artificial hard boundaries, and ignores the fact that the in-band region does not have the same probabilistic importance everywhere. This paper utilises the statistical measure Relative Average Normalised Density (RAND), which indicates whether the simulated infusion profile coincides with a region of high probability determined from the recorded empirical data. RAND takes values between 0 and 1, where a value close to 1 means that the simulated infusion profile is, on average, in a high probability region and hence in good agreement with the empirical data. This measure Page 13 of 32 effectively replaces the hard boundaries of the probability band by soft boundaries defined by probabilistic importance determined from the empirical data. Specific details on the development of the RAND metric can be found in the relevant literature [17, 20, 50-54]. RAND measures how probabilistically similar the model outputs are to the smoothed data, and hence the degree of compatibility between the model and the empirical data. For example, a RAND of 0.6 may be interpreted as the model outputs being 60% similar, on average, to the smoothed data. Since the model is deterministic, its outputs do not come from the same probabilistic mechanism that generated the recorded data. Hence, RAND is an extremely stringent measure, and consistently high RAND values close to 1 are not expected. A reasonable and practical threshold for adequate model performance is RAND ≥ 0.5, which says that the model outputs are more similar than not, to the smoothed data. If comparing two or more models to the data, the model with the higher RAND value would be selected. In this case, with one model, the threshold is 0.5. Finally, Relative Total Dose (RTD) expresses the total dose administered in the simulation as a percentage of the actual total recorded dose [17]. Ideally, this metric would approach 100%, indicating that the simulated total drug dose is identical to the recorded total drug dose. RTD, TIB and RAND are different objective measures of the ability of the model to capture the essential dynamics of the agitation-sedation system. Together, they create a clear picture of the model’s performance. 2.2 Analyses The results of simulations with and without the EAR dynamic in Equation (6) are analysed using all of these performance measures. The goal is to investigate the impact of including EAR. The first goal is to ascertain the physiological range of the EAR parameter, w3, by broadly testing a range of possible values over all patients. Secondly, the effect of EAR dynamics on modelled drug sensitivity, w2(t), and the resulting fit with recorded infusion data are studied. Page 14 of 32 3.0 RESULTS The w3 value corresponding to the best fit between the simulated and recorded data was w3=0.0001 for all patients. The performance metrics in Table 1 show high values for the model with (w3=0.0001) and without (w3=0) EAR. The RAND values for simulations without EAR have a median of 0.77 with standard deviation 0.08 and range [0.51, 0.89]. TIB without EAR has a median of 0.87 with standard deviation of 0.05 and range [0.78, 0.97], while RTD has a median of 98.7 with standard deviation 2.1 and range [93.1, 101.4]. Similarly, the RAND values for simulations including EAR have a median of 0.78 with standard deviation 0.07 and range [0.55, 0.91]. TIB including EAR has a median across all patients of 0.89 with standard deviation of 0.04 and range [0.81, 0.97], and RTD has a median of 98.6 with standard deviation 2.1 and range [92.5, 101.0]. For w3 =0.00001 slightly lower values of the performance metrics were observed, and for w3 = 0.001 much lower values were observed. These high reported RAND, RTD and TIB values correspond to very close fits of the simulated infusion rate to the recorded infusion rate, as shown in Figures 2-4. In these figures, the upper plot shows the time-varying nature of the fitted w2(t), while the lower plot shows the resulting fit of the simulated and recorded infusion rates. In each of these figures, the dark solid line shows the results without the inclusion of EAR, and the dark dotted line shows the results including EAR. The light solid line in the lower plots shows the recorded infusion rate, and its 99% probability band is the grey band around it. 4.0 DISCUSSION The statistical model validation metric, RAND, complements and completes the other statistical tools (RTD and TIB) previously employed [17, 19-21] for model validation of this system. The probability band with hard boundaries developed previously allows visual Page 15 of 32 assessment and numerical TIB evaluation, which is useful during model development and refinement. The RTD value simply represents a global assessment of the similarity of the resulting infusion rates to clinical data. In contrast, RAND provides an objective, calibrated measure of statistical compatibility between the simulated infusion profile and the recorded data. It thus provides a statistical measure of how well the model captures the essential dynamics of the agitation-sedation system. Together, all three metrics (RAND, TIB and RTD) cover a range of model validation criteria. The best fit between the simulated and recorded data was obtained using w3=0.0001 for each and every patient, which shows the low inter-patient variability and low sensitivity to the EAR parameter, and indicates that w3 can be assumed constant across all patients. The sensitivity of the model to the value of w3 is reduced further by the fitting process for w2(t), which can compensate for potentially slightly incorrect selection of w3 [47]. This insensitivity in the EAR parameter is also seen for the similar term in the glucose-insulin system modelling [55]. Hence, it might be expected. The impact of EAR can be seen by comparing columns 2 and 3 to columns 5 and 6 in Table 1. The median and upper and lower quartiles of the RAND and TIB for the model including EAR are all higher than those without EAR, and the standard deviations of these metrics are reduced for the model including EAR. These results indicate that the addition of the EAR dynamic improves the ability of the model to capture the observed dynamics of the agitationsedation system. The upper plot in Figures 2-4 show that while the difference is small, the inclusion of EAR results in a slight decrease in w2(t) throughout the entire profile, especially where infusion rates in the lower plot are very low. This result should be expected since the EAR dynamic is another form of agitation decrease thus reducing the sedative sensitivity required to match the clinical data when it is included. Note that when infusion rates are very low the primary Page 16 of 32 means of agitation reduction would be EAR. Hence, the model that includes EAR has the greatest effect during periods of low sedation infusion where there is less exogenous agitation reduction. Such periods of low infusion, where the EAR dynamic is most important, would most notably include sedative weaning prior to extubation. Visually, the lower plots on Figs. 2–4 show that the current model produces infusion profiles that are a close approximation to the recorded infusion profiles. The fact that the solid and dotted dark lines on the bottom plot in these figures are difficult to distinguish indicates that the simulated infusion rates are very similar whether EAR is included or not. High median RAND values for both models of 0.77 (without EAR) and 0.78 (with EAR), support this visual finding with a statistically-based objective measure. Minimum RAND values of 0.51 and 0.55 for the two respective models reinforce this result. These results support both models as a valid representation of the fundamental agitation-sedation dynamics present in a broad spectrum of ICU patients. While the addition of the EAR dynamic increases the ability of the model to capture the observed dynamics of the agitation-sedation system, the improvement is relatively small when assessed globally across entire records. Further, the sensitivity of the model to the w3 parameter is low, a feature also found for non-drug mediated endogenous removal mechanisms in similar dynamic systems such as the glucose-insulin system [47, 55]. This result offers the question of whether the EAR dynamic should be included at all. It may be possible that the errors and assumptions in the development of the model and the performance metrics are larger than the difference in performance between the model with and without EAR. Although this issue may represent a limitation of the model, it is important to note that the inclusion of EAR is important for accurately capturing periods of low, or no, sedative infusion, such as weaning. In addition, visual inspection of results show that in periods of low or no infusion the impact is greater than elsewhere. Page 17 of 32 The performance parameters summarized in Table 1 were achieved using very few patientspecific PD parameters and identical PK parameters across all patients. This result supports the idea that interpatient pharmacological variability is due primarily to PD differences rather than PK differences, as reported in several studies [20, 38, 39]. However, the insensitivity of the w3 parameter and its smaller impact on results indicate that EAR is not a significant PD parameter in this case. However, EAR becomes important when simulating low infusion rates, such as during weaning. Therefore, although EAR is not always a significant dynamic, it is important during specific clinical periods. Because it has no negative impact during other periods it should be retained. For some patients high w2 values are observed immediately after periods of relatively constant w2, as seen in Figure 2-4. Although this feature is sometimes located centrally in recorded data, in many cases this feature is observed at the end of recorded data and may correspond to weaning off sedation. These observations may be the result of a change in sedative sensitivity as the patient’s health improves prior to them leaving the ICU. However, the magnitudes of the changes are in some cases quite large, which indicates that the change in observed sedative sensitivity may also be the result of a delayed release of drugs stored in fatty tissue or the effects of active metabolites. Although the peripheral compartment represents the fatty tissues into which these drugs and/or metabolites can be deposited, this dynamic may be considerably more prominent than that currently modelled, requiring an additional separate storage compartment. Because benzodiazepines are lipid soluble, longterm infusions can lead to depositions of large amounts of the administered drug in fatty tissues [56]. When the sedative administration stops, the stored drug is released back into circulation [2, 6, 56]. Alternatively, these effects may be due to the prolonged action of active metabolites. If these dynamics were present during the recordings, the effect would be an inflated observed sedative sensitivity, w2. Page 18 of 32 To determine if a relationship exists between the improvement resulting from the EAR dynamic and the duration of the infusion, a correlation analysis was undertaken. The correlation between the improvement resulting from inclusion of the EAR dynamic and the duration of infusion was determined using the non-parametric bootstrap (Efron et al, 1993), which does not require a parametric distribution for the data. The correlation coefficient was found to be r=-0.007, with 95% confidence interval bounds of (-0.246 , 0.398), and P=0.968, indicating that there is almost 97% chance that correlation exists. Although there is a lack of correlation, this does not imply that delayed release of drugs stored in fatty tissue or the effects of active metabolites are not present. Further investigation is required to determine the effect of an additional storage dynamic and active metabolites. Finally, the model incorporates physiological drug effect saturation dynamics, seen by the dual-sigmoid surface in Fig. 1. Physiological metabolism and excretion of Morphine and Midazolam is limited by renal and hepatic clearance capacity. However, the maximum clearance rate and plasma concentrations at which the dynamics change from first-order to saturated zero-order kinetics are not easily obtained, particularly in the ICU population. A lack of available parameter values therefore makes the immediate implementation of more representative Michaelis-Menton saturation dynamics difficult. Clinical trials with quantified agitation sensors [13, 14] and measured plasma drug concentrations could provide the data to improve these model parameters and add any necessary additional dynamics. Page 19 of 32 5.0 CONCLUSIONS The physiological model presented captures the essential dynamics of the agitation-sedation system, both with and without the Endogenous Agitation Reduction (EAR) term. High median RAND values of 0.77 (without EAR) and 0.78 (with EAR) support and minimum RAND values of 0.51 and 0.55 for the two respective models show that both models are valid representations of the fundamental agitation-sedation dynamics present in a broad spectrum of ICU patients. While the addition of the EAR dynamic increases the ability of the model to capture the observed dynamics of the agitation-sedation system, the improvement is relatively small and the sensitivity of the model to the w3 parameter is low. Although this may represent a limitation of the model, the inclusion of EAR is important for accurately capturing periods of low, or no, sedative infusion, such as weaning. Page 20 of 32 6.0 ACKNOWLEDGEMENTS The authors wish to acknowledge the funding for this research, provided by the New Zealand Foundation for Research, Science and Technology through a Bright Futures Top Achiever Doctoral Scholarship, and the Todd Foundation through the Award for Excellence. REFERENCES [1] A.M. Burns, M.P. Shelly and G.R. Park, “The use of sedative agents in critically ill patients,” Drugs, vol. 43(4), pp. 507–515, 1992. [2] J.P. Kress, A. Pohlman, M. O’Conner and J. Hall, “Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation,” N. Engl. J. Med., vol. 342(20), pp. 1471–1477, 2000. [3] G.L. Fraser and R.R. Riker, “Advances and controversies in sedating the adult critically ill,” The New York Heath-System Pharmacist, vol. 20(3), pp. 17–24, 2001. [4] N.A. Smyrnios, A. Connolly, M.M. Wilson, F.J. Curley, C.T. French, S.O. Heard and R.S. Irwin, “Effects of a multifaceted, multidisciplinary, hospital-wide quality improvement program on weaning from mechanical ventilation,” Crit. Care Med. vol. 30(6), pp. 1224–1230, 2002. [5] J.W. Szokol and J.S. Vender, “Anxiety, delirium, and pain in the intensive care unit,” Crit. Care Clin. vol. 17(4), pp. 821–842, 2001. [6] J. Barr and A. Donner, “Optimal intravenous dosing strategies for sedatives and analgesics in the intensive care unit,” J. Crit. Care Clin., vol. 11(4), pp. 827–847, 1995. [7] G. Brattebo, D. Hofoss, H. Flaatten, A.K. Muri, S. Gjerde and P.E. Plsek, “Effect of a scoring system and protocol for sedation on duration of patients’ need for ventilator support in a surgical intensive care unit,” BMJ., vol. 324(7350), pp. 1386–1389, 2002. [8] B.E. Smith and J.G. Reves, Computer-assisted continuous infusion of intravenous anesthesia drugs, Boston, Little, Brown and Company, 1995. Page 21 of 32 [9] G.M. Shaw, R.A. Dove, K.M. Greenfield, A.D. Rudge and J.G. Chase, “A computerised approach to sedation administration in critically ill patients,” in Proc. of ANZICS/ACCCN 28th Australia and New Zealand ASM on Intensive Care, Dunedin, New Zealand, 2003. [10] G.M. Shaw, J.G. Chase, A.D. Rudge, C. Starfinger, Z. Lam, D. Lee, G.C. Wake, K. Greenfield and R. Dove, “Rethinking sedation and agitation management in critical illness,” Critical Care and Resuscitation, vol. 5, pp. 109–120, 2003. [11] C.R. Weinert, L. Chlan and C. Gross, “Sedating critically ill patients: factors affecting nurses’ delivery of sedative therapy,” Am. J. Crit. Care, vol. 10(3), pp. 156–165, 2001. [12] G.L. Fraser and R.R. Riker, “Monitoring sedation, agitation, analgesia, and delirium in critically ill adult patients,” Crit. Care. Clin., vol. 17(4), pp. 967–987, 2001. [13] J.G. Chase, F. Agogué, C. Starfinger, Z. Lam, G.M. Shaw, A.D. Rudge and H. Sirisena, “Quantifying agitation in sedated ICU patients using digital imaging,” J. of Computer Methods and Programs in Biomedicine, vol. 76(2), pp. 131–141. [14] J.G. Chase, C. Starfinger, Z. Lam, F. Agogué and G.M. Shaw, “Quantifying agitation in sedated ICU patients using heart rate and blood pressure,” Physiological Measurement, vol. 25, pp. 1037–1051. [15] Z. Lam, C. Starfinger, J.G. Chase, G.M. Shaw and F. Agogué, “Movement quantification for use in agitation quantification in sedated ICU patients,” In Proc. of the World Congress on Medical Physics and Biomedical Engineering (WC2003), Sydney, Australia, 2003. [16] C. Starfinger, Z. Lam, J.G. Chase, G.M. Shaw and F. Agogué, “Measurement of agitation in sedated ICU patients using adaptive signal processing and fuzzy mathematics,” In Proc. of the World Congress on Medical Physics and Biomedical Engineering (WC2003), Sydney, Australia, 2003. Page 22 of 32 [17] J.G. Chase, A.D. Rudge, G.M. Shaw, G.C. Wake, D. Lee, I. Hudson and L. Johnston, “Modelling and control of the agitation-sedation cycle for critical care patients,” Medical Engineering and Physics, vol 26(6), pp. 459–471, 2004. [18] A.D. Brook, T.S. Ahrens, R. Schaiff, D. Prentice, G. Sherman, W. Shannon and M.H. Kollef, “Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation,” Crit. Care Med., vol. 27(12), pp. 2609–2615, 1999. [19] A.D. Rudge, J.G. Chase, G.M. Shaw and G.C. Wake, “Improved agitation management in critically ill patients via feedback control of sedation administration,” In Proc. World Congress on Medical Physics and Biomedical Engineering (WC2003), Sydney, Australia, August 24–29, 2003, 4 pages, ISSN: 1727–1983. [20] A.D. Rudge, J.G. Chase, G.M. Shaw, L. Johnston and G.C. Wake, “Modelling and control of the agitation-sedation cycle,” In Proc. of the 5th IFAC Symposium on Modelling and Control in Biomedical Systems, Melbourne, Australia, August 21–23 pp. 89–95, 2003. [21] A.D. Rudge, J.G. Chase, G.M. Shaw and D.S. Lee, “Physiologically-based minimal model of agitation-sedation dynamics,” in Proc. 26th International Conf. of IEEE Engineering in Med. and Biology Society (EMBS 2004), San Francisco, CA, Sept 1– 5, 2004. [22] Chase, JG , Rudge, AD, Lee, DS and Shaw, GM (2004). “H-infinity control analysis of patient agitation management in the critically ill,” Intl Journal of Intelligent Systems Technologies and Applications (IJISTA), vol. 1(1-2), pp. 111–125. [23] C.F. Minto, T.W. Schnider, T.G. Short, K.M. Gregg, A. Gentilini and S.L. Shafer, “Response surface model for anesthetic drug interactions,” Anesthesiology, vol. 92(6) pp. 1603–1616, 2000. [24] I. Meineke, S. Freudenthaler, U. Hofmann, E. Schaeffeler, G. Mikus, M. Schwab, H.W. Prange, C.H. Gleiter and J. Brockmoller, “Pharmacokinetic modelling of morphine, morphine-3-glucuronide and morphine-6-glucuronide in plasma and Page 23 of 32 cerebrospinal fluid of neurosurgical patients after short-term infusion of morphine,” Br. J. Clin. Pharmacol., vol. 54(6), pp. 592–603, 2002. [25] G. Andersen, L. Christrup and P. Sjogren, “Relationships among morphine metabolism, pain and side effects during long-term treatment: an update,” J. Pain Symptom Manage., vol. 25(1), pp. 74–91, 2003. [26] J.J. Bates, J.F. Foss and D.B. Murphy, “Are peripheral opioid antagonists the solution to opioid side effects?” Anesth Analg, vol. 98(1), pp. 116–122, 2004. [27] J. Lotsch, C. Skarke, H. Schmidt, J. Liefhold and G. Geisslinger, “Pharmacokinetic modelling to predict morphine and morphine-6-glucuronide plasma concentrations in healthy young volunteers,” Clin. Pharmacol. Ther., vol. 72(2), pp. 151–162, 2002. [28] C.C. Faura, S.L. Collins, R.A. Moore and H.J. McQuay, “Systematic review of factors affecting the ratios of morphine and its major metabolites,” Pain, vol. 74(1), pp. 43–53, 1998. [29] R.W. Milne, R.L. Nation and A.A. Somogyi, “The disposition of morphine and its 3and 6-glucuronide metabolites in humans and animals, and the importance of the metabolites to the pharmacological effects of morphine,” Drug Metab. Rev. vol. 28(3), pp. 345–472, 1996. [30] H.P. Platten, E. Schweizer, K. Dilger, G. Mikus and U. Klotz, “Pharmacokinetics and the pharmacodynamic action of midazolam in young and elderly patients undergoing tooth extraction,” Clin. Pharmacol. Ther., vol. 63(5), pp. 552–560, 1998. [31] P. Persson, A. Nilsson, P. Hartvig and A. Tamsen, “Pharmacokinetics of midazolam in total I.V. anaesthesia,” Br. J. Anaesth., vol. 59(5), pp. 548–556, 1987. [32] M. Bolon, O. Bastien, C. Flamens, S. Paulus, F. Salord and R. Boulieu, “Evaluation of the estimation of midazolam concentrations and pharmacokinetic parameters in intensive care patients using a bayesian pharmacokinetic software (PKS) according to sparse sampling approach,” J. Pharm. Pharmacol., vol. 55(6), pp. 765–771, 2003. Page 24 of 32 [33] T.M. Bauer, R. Ritz, C. Haberthur, H.R. Ha, W. Hunkeler, A.J. Sleight, G. ScolloLavizzari and W.E. Haefeli, “Prolonged sedation due to accumulation of conjugated metabolites of midazolam,” Lancet, vol. 346(8968), pp. 145–147, 1995. [34] A. Shafer, “Complications of sedation with midazolam in the intensive care unit and a comparison with other sedative regimens,” Crit. Care. Med., vol. 26(5), pp. 947–956, 1998. [35] B. Tuk, M.F. van Oostenbruggen, V.M. Herben, J.W. Mandema and M. Danhof, “Characterization of the pharmacodynamic interaction between parent drug and active metabolite in vivo: midazolam and alpha-OH-midazolam,” J. Pharmacol. Exp. Ther., vol. 289(2), pp. 1067–1074, 1999. [36] C. Young, N. Knudsen, A. Hilton and J.G. Reves, “Sedation in the intensive care unit,” Crit. Care Med., vol. 28(3), pp. 854–866, 2000. [37] H. Oldenhof, M. de Jong, A. Steenhoek and R. Janknegt, “Clinical pharmacokinetics of midazolam in intensive care patients, a wide interpatient variability?” Clin. Pharmacol. Ther., vol. 43(3), pp. 263–269, 1988. [38] H.R. Vinik, J. Reves, D. Greenblatt, D. Abernethy, and L. Smith, “The pharmacokinetics of midazolam in chronic renal failure patients,” Anesthesiology, vol. 59(5), pp. 390–394, 1983. [39] S. Albrecht, H. Ihmsen, W. Hering, G. Geisslinger, J. Dingemanse, H. Schwilden and J. Schuttler, “The effect of age on the pharmacokinetics and pharmacodynamics of Midazolam,” Clin. Pharmacol. Ther., vol. 65(6), pp. 630–639, 1999. [40] R.L. Levine, “Pharmacology of intravenous sedatives and opioids in critically ill patients,” Crit. Care. Clin., vol. 10(4), pp. 709–731, 1994. [41] B.K. Wagner and D. O'Hara, “Pharmacokinetics and pharmacodynamics of sedatives and analgesics in the treatment of agitated critically ill patients,” Clin. Pharmacokinet., vol. 33(6), pp. 426–453, 1997. [42] B. De Jonghe, D. Cook, L. Griffith, C. Appere-de-Vecchi, G. Guyatt, V. Theron, A. Vagnerre and H. Outin, “Adaptation to the Intensive Care Environment (ATICE): Page 25 of 32 development and validation of a new sedation assessment instrument,” Crit. Care. Med., vol. 31(9), pp.2344–2354, 2003. [43] R. Romberg, E. Olofsen, E. Sarton, J. den Hartigh, P.E. Taschner and A. Dahan, “Pharmacokinetic-pharmacodynamic modelling of morphine-6-glucuronide-induced analgesia in healthy volunteers: absence of sex differences,” Anesthesiology, vol. 100(1), pp. 120–133, 2004. [44] R. Koopmans, J. Dingemanse, M. Danhof, G.P. Horsten, C.J. van Boxtel, “Pharmacokinetic-pharmacodynamic modelling of midazolam effects on the human central nervous system,” Clin. Pharmacol. Ther., vol. 44(1), pp. 14–22, 1988. [45] N. Carlson, Physiology of Behaviour, 8th Edition, Boston, Allyn and Bacon, 2001. [46] A.C. Guyton and J.E. Hall, Textbook of Medical Physiology, 9th Edition, London, W.B. Saunders Company, 1996. [47] Hann, CE, Chase, JG, Lin, J, Lotz, T, Doran, CV, and Shaw, GM (2005). “IntegralBased Parameter Identification For Long-Term Dynamic Verification Of A GlucoseInsulin System Model,” J. of Computer Methods and Programs in Biomedicine, vol. 77(3), pp. 259–270. [48] H. Helson, Psychology: A study of a science, vol. 1, New York, McGraw-Hill, 1959. [49] K.M. Greenfield, R.A. Dove and G.M. Shaw, “Optimisation of sedation therapy within an intensive care setting,” In Proc. of the Engineering and Physical Sciences in Medicine, Fremantle, Australia, 2001. [50] M.P. Wand and M.C. Jones, Kernel smoothing. Monographs on statistics and applied probability, London, Chapman & Hall, 1995. [51] W. Hardle, Applied nonparametric regression. Cambridge, Cambridge University Press, 1990. [52] D.S. Lee, A.D. Rudge, J.G. Chase, G.M. Shaw, L. Johnston and G.C. Wake, “Dynamic model assessment using a probability band for local linear kernel regression, with an application in agitation-sedation modelling,” in Proc. of New Page 26 of 32 Zealand Statistical Association 54th Annual Conference, Massey University, Palmerston North, 2003. [53] Rudge, AD, Chase, JG, Shaw, GM, Lee, DS (2005). “Physiological modelling of agitation–sedation dynamics,” Medical Engineering and Physics, Accepted March 2005, to appear. [54] Lee, DS, Rudge, AD, Chase, JG, Shaw, GM (2005). “A New Model Validation Tool Using Kernel Regression and Density Estimation,” J. of Computer Methods and Programs in Biomedicine, Accepted March 2005, to appear. [55] Chase, JG , Shaw, GM, Lin, J, Doran, CV, Hann, CE, Robertson, MB, Browne, PM, Lotz, T, Wake, GC and Broughton, R (2005). “Adaptive bolus-based targeted glucose regulation of hyperglycaemia in critical care,” Medical Engineering and Physics, vol. 27(1), pp. 1-11, ISSN: 1350-4533 [56] Arbour, R. (2000). "Sedation and pain management in critically ill adults." Crit Care Nurse, vol. 20(5): 39-56. FIGURE & TABLE CAPTIONS Fig. 1. Representation of the agitation-sedation system model, showing separate compartmental pharmacokinetics (upper portion), the pharmacodynamic effect surface with the associated defining equation [21]. Fig. 2. Plot showing the effect of endogenous agitation reduction (EAR) on sedative sensitivity,w2(t),(upper plot), and fit to recorded infusion rate (lower plot) for Patient 2. The dark solid line shows the results without the inclusion of EAR, and the dark dotted line shows the results including EAR. The light solid line in the lower plots shows the recorded infusion rate, and its 99% probability band is indicated by the grey band. Fig. 3. Plot showing the effect of endogenous agitation reduction (EAR) on sedative sensitivity,w2(t),(upper plot), and fit to recorded infusion rate (lower plot) for Patient 37. The dark solid line shows the results without the inclusion of EAR, and Page 27 of 32 the dark dotted line shows the results including EAR. The light solid line in the lower plots shows the recorded infusion rate, and its 99% probability band is indicated by the grey band. Fig. 4. Plot showing the effect of endogenous agitation reduction (EAR) on sedative sensitivity,w2(t),(upper plot), and fit to recorded infusion rate (lower plot) for Patient 36. The dark solid line shows the results without the inclusion of EAR, and the dark dotted line shows the results including EAR. The light solid line in the lower plots shows the recorded infusion rate, and its 99% probability band is indicated by the grey band. Table 1. Validation metrics for 37 patients for simulations with and without EAR Page 28 of 32 Morphine Midazolam C co C cs o K CL K opc C op K eco o cp K K ceo C o e s K CL K ecs K ces C s e EComb C eo o C50 C 50s C es ( ) EComb CO C S C50 ( ) E0 [ E max ( ) E0 ] ( ) CO C S 1 C50 ( ) Fig. 1. Representation of the agitation-sedation system model showing separate compartmental pharmacokinetics (upper portion) and the pharmacodynamic effect surface with the associated defining equation [21]. Cc, Cp and Ce are the drug concentrations (mg/L) in the central, peripheral and effect compartments respectively, o s C50 and C50 represent the concentrations at which Morphine or Midazolam would have 50% effect if administered alone, and Kij is the transfer rate (L/min) from compartment i to compartment j. Page 29 of 32 x 10 -3 2 1.8 1.6 1.4 w2(t) 1.2 1 0.8 0.6 0.4 0.2 0 0 20 40 0 20 40 60 80 100 80 100 4.5 4 Infusion Rate (mL/h) 3.5 3 2.5 2 1.5 1 0.5 0 60 Time (Hours) Fig. 2. Plot showing the effect of endogenous agitation reduction (EAR) on sedative sensitivity,w2(t),(upper plot), and fit to recorded infusion rate (lower plot) for Patient 2. The dark solid line shows the results without the inclusion of EAR, and the dark dotted line shows the results including EAR. The light solid line in the lower plots shows the recorded infusion rate, and its 99% probability band is indicated by the grey band. Page 30 of 32 0.01 w2(t) 0.008 0.006 0.004 0.002 0 0 10 20 0 10 20 30 40 50 60 40 50 60 Infusion Rate (mL/h) 15 10 5 0 30 Time (Hours) Fig. 3. Plot showing the effect of endogenous agitation reduction (EAR) on sedative sensitivity,w2(t),(upper plot), and fit to recorded infusion rate (lower plot) for Patient 36. The dark solid line shows the results without the inclusion of EAR, and the dark dotted line shows the results including EAR. The light solid line in the lower plots shows the recorded infusion rate, and its 99% probability band is indicated by the grey band. Page 31 of 32 x 10 -3 3.5 3 w2(t) 2.5 2 1.5 1 0.5 0 0 20 40 0 20 40 60 80 100 120 80 100 120 18 16 Infusion Rate (mL/h) 14 12 10 8 6 4 2 0 60 Time (Hours) Fig. 4. Plot showing the effect of endogenous agitation reduction (EAR) on sedative sensitivity,w2(t),(upper plot), and fit to recorded infusion rate (lower plot) for Patient 37. The dark solid line shows the results without the inclusion of EAR, and the dark dotted line shows the results including EAR. The light solid line in the lower plots shows the recorded infusion rate, and its 99% probability band is indicated by the grey band. Page 32 of 32 Table 1. Validation metrics for 37 patients for simulations with and without EAR 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 Max UQ Median LQ Min STD RAND 0.79 0.80 0.69 0.69 0.83 0.82 0.77 0.74 0.73 0.78 0.71 0.73 0.79 0.51 0.76 0.71 0.86 0.80 0.88 0.89 0.79 0.69 0.75 0.77 0.67 0.86 0.70 0.79 0.60 0.87 0.83 0.77 0.78 0.73 0.75 0.64 0.73 0.89 0.80 0.77 0.71 0.51 0.08 No EAR, w3=0 TIB RTD (%) 0.97 100.3 0.89 98.3 0.94 101.3 0.88 95.8 0.85 96.5 0.92 98.5 0.86 93.4 0.85 98.6 0.81 101.4 0.87 97.4 0.87 101.2 0.89 99.0 0.87 96.9 0.90 98.7 0.87 100.7 0.83 99.7 0.89 97.8 0.83 97.1 0.94 100.0 0.94 99.1 0.84 96.4 0.80 98.6 0.88 93.1 0.91 98.7 0.78 101.1 0.90 99.5 0.80 97.2 0.87 99.4 0.93 93.9 0.90 98.7 0.92 99.9 0.85 99.0 0.88 99.3 0.82 100.3 0.82 100.3 0.79 97.9 0.88 95.6 0.97 101.4 0.90 99.9 0.87 98.7 0.84 97.2 0.78 93.1 0.05 2.1 EAR, w3=0.0001 RAND TIB RTD (%) 0.79 0.97 99.7 0.84 0.92 97.7 0.74 0.95 99.7 0.69 0.89 95.7 0.84 0.86 96.9 0.83 0.92 98.5 0.79 0.86 92.6 0.77 0.85 98.8 0.75 0.82 101.0 0.82 0.89 97.7 0.75 0.89 100.8 0.76 0.91 98.4 0.82 0.88 97.3 0.55 0.90 97.3 0.77 0.88 100.5 0.73 0.84 100.0 0.86 0.89 97.6 0.84 0.84 97.6 0.89 0.94 100.1 0.91 0.94 99.2 0.81 0.85 96.0 0.72 0.83 98.3 0.76 0.89 93.1 0.78 0.91 98.8 0.69 0.81 100.6 0.88 0.92 98.8 0.77 0.83 97.4 0.82 0.88 99.6 0.70 0.94 92.5 0.87 0.90 98.6 0.86 0.93 99.9 0.79 0.87 99.2 0.81 0.89 99.5 0.77 0.84 100.0 0.78 0.84 100.0 0.74 0.84 96.8 0.76 0.89 96.0 0.91 0.97 101.0 0.83 0.91 99.7 0.78 0.89 98.6 0.75 0.85 97.3 0.55 0.81 92.5 0.07 0.04 2.1