Introduction to Multifamily Groups (.ppt)
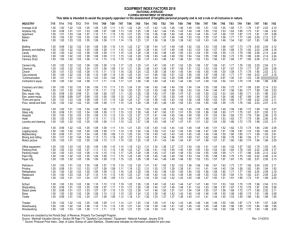
advertisement

Introduction to Multifamily Groups Alex Kopelowicz, MD Raising the Bar Project-Valley Nonprofit Resources Human Interaction Research Institute PORT Treatment Recommendations Patients who have on-going contact with their families should be offered a family psychosocial intervention which spans at least nine months and which provides a combination of education about the illness, family support, crisis intervention, and problem solving skills training. Such interventions should also be offered to non-family caregivers. Standard Approaches to Family Work in Serious Mental Illness Psychoeducation Communication skills training Problem solving techniques Social network development (MFG) Better outcomes in family psychoeducation Over 20 controlled clinical trials, comparing to standard outpatient treatment, have shown: – Much lower relapse rates and rehospitalization Up to 75% reductions of rates; minimally 50% – Increased employment At least twice the number of consumers employed, and up to four times greater--over 50% employed after two years--when combined with supported employment – Improved family relationships and well-being – Reduced friction and family burden – Reduced medical illness in family members Doctor visits for family members decreased by over 50% in one year Dixon et al 2003 MFG TRAINING PROGRAM DAY 1 9:00- 9:30am Welcome/Overview of MFG Training What is MFG and why should we do it? 9:30 -12:00 pm The Psychoeducational Workshop 12:00-1:00 pm Lunch 1:00 – 4:00 pm McFarlane Videoconference Science of Mental Disorders Family Psychoeducation Outcomes Overview of Treatment Model DAY 2 9:00 – 12:00 noon Joining Sessions (Demonstration and Role Play) 12:00 – 1:00 pm Lunch 1:00 – 4:00 pm MFG Sessions (Demonstration and Role Play) Stages of a Psychoeducational Multifamily Group Joining Family and patient separately 3-6 weeks Educational workshop Families only 1 day Ongoing MFG Families & patients bi-weekly for 1 year JOINING with FAMILIES & CLIENTS JOINING means to CONNECT, BUILD RAPPORT, CONVEY EMPATHY, ESTABLISH AN ALLIANCE, ENGAGE It is the First Stage of Treatment Designed to create a bond between Client/Family Members and Family Clinicians CLINICIAN as ADVOCATE JOINING PROCEDURES THREE Joining Meetings SEPARATELY with Relatives and Clients WEEKLY – 1 HOUR with Relatives, ½ HOUR with Clients Start sessions A.S.A.P. after crisis or hospitalization Gain an understanding of family’s stresses, problems, reactions to illness, etc. JOINING – I 15 Minutes of SOCIAL TALK Review any recent CRISIS: Who and What Helped or Didn’t IDENTIFY WARNING SIGNS – PRODROMAL SIGNS – PRECIPITANTS Distribute to Families & Keep for Future Reference Describe the Plan for On-going MFG sessions 5 Minutes SOCIALIZING JOINING – II 15 Minutes of SOCIAL TALK FAMILY’S EXPERIENCE DURING EPISODES The Sharing of Painful Events: A Crucial Aspect of “Joining” The Client/Family’s Understanding of Etiology Family’s Social Network & Resources (Material & Emotional) 5 Minutes SOCIALIZING JOINING – III 15 Minutes of SOCIAL TALK FAMILY’S SOCIAL NETWORK & RESOURCES SHORT & LONG-TERM GOALS (e.g., Prevent Relapse) Preparation for Workshop & MFGs MULTIFAMILY GROUPS Five to Eight Families Two Clinicians 1 ½-Hour Sessions – Biweekly – 1 Year Minimum Refreshments/Snacks are provided Initial Sessions avoid emphasis on clinical issues Initial Sessions emphasize establishing a working alliance by building group identity and developing a sense of mutual interest and concern. Drop outs are Failures FIRST MFG SESSION “GETTING TO KNOW EACH OTHER” Go Around the Room Background Hobbies Occupation Interests Clinician Goes First (Discloses/Shares with the Group SETTING BASIC RULES Regular ATTENDANCE (for Relatives) CONFIDENTIALITY (No Pressure to Disclose) INTERACTION AMONG MEMBERS PHYSICAL/EMOTIONAL CONTROL SECOND MFG SESSION “HOW MENTAL ILLNESS HAS CHANGED OUR LIVES” Building a SENSE OF TRUST & COMMITMENT Sense of COMMON EXPERIENCE (Listen to each other) Strengthening GROUP IDENTITY & SENSE OF RELIEF The PATIENT’S INNER EXPERIENCES Clinicians emphasize the vital role of SHARING GRIEF, CONFUSION, GUILT, FEAR with those “on the same boat”. AND HOPE Remind participants about Problem Solving (next session) GENERAL POINTS New Members Late-Arriving Members Reminders about Attending Crises & Emergencies COMMUNICATION & INTERACTIONS Clinicians DON’T speak for clients or relatives Interaction among member is essential Clients are ENCOURAGED (not pressured) to participate Respect other’s turn and avoid criticism PROBLEM SOLVING IN MFGs The CORE of MFG Sessions Designed to compensate Information-Processing Deficits in Mental Disorders FORMAT: Checking in 15 Minutes Go-round 20 Minutes Selecting a Problem to Solve 5 Minutes Solving the Problem 45 Minutes Wrap-up Socializing 5 Minutes Clinicians should GET READY and HAVE A PLAN – IN ADVANCE SELECTING A PROBLEM TO SOLVE TOPICS: Safety in The Home Medication Compliance Drugs and Alcohol Life Events Outside Agency Events Disagreements among Family Members Conflict with a Family Guideline “REJECTED” PROBLEMS: Make a Direct Suggestion and Review Outcome Meet Outside the Group (E.G., Crises) Refer to Past Solutions that Apply Refer to Solution/Family with Successful Outcome THE PROBLEM-SOLVING METHOD 1. 2. 3. 4. 5. 6. Define the Problem or Goal List Possible Solutions Evaluate Advantages and Disadvantages of each Solution Choose “the best” Solution Implement Plan to Carry Out Solution Review Implementation and Outcome