chapter20.pptx
advertisement

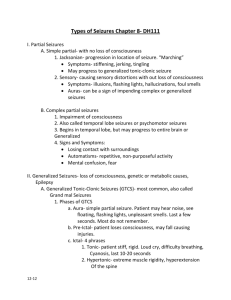
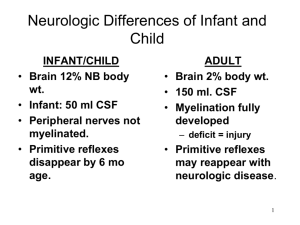
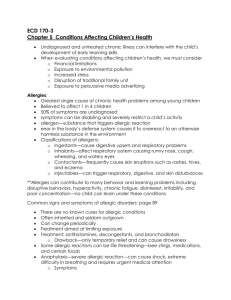
• Scalp protects skull but infection can enter through veins draining the face or through the loose connective tissue layer • Trauma to skull can produce hematomas or fractures that can let infection enter • Cerebrospinal fluid protects the brain, but can carry infection • Meningeal layers can have hemorrhages & hematomas • Vertebral column can dislocate, fracture, or disks can protrude, which can affect neural function • Lordosis – exaggerated lumbar curvature • Kyphosis – exaggerated thoracic curvature • Scoliosis – lateral displacement • Discs decrease in size & flexibility with age and can herniate • Autoregulation of blood flow guarantees adequate blood supply to the brain • Infarcts occur at margins of adjacent vascular fields that supply the cortex – watershed zones, after impaired perfusion (fibrillation) or oxygenation (CO poisoning, drowning) • Areas of infarct undergo liquefaction nerosis, leaving a cyst – lacunae • Vasogenic edema – with inflammation • Brain tissue swells if capillaries get permeable & allow accumulation of fluid • Cytotoxic edema – results from hypoxia – intracellular swelling • Expansion of brain, CSF, blood in the skull can increase intracranial pressure, impair perfusion, compress, shift or tear tissue, herniation can occur • Compensations include decreased CSF & blood volume, with eventual hypoxia that increase blood pressure, eventually coma & death • Oversecretion, impaired absorption, blocked circulation of CSF expands the ventricles – hydrocephalus – alleviated by shunting • Consciousness levels can be measured to assess neural function • Causes of coma include alcohol or barbiturate overdose, trauma, stroke, epilepsy, meningitis, diabetes, kidney failure, heart disease • Reflexes & automatic functions aid in localization of CNS lesions • Neural tube defects can lead to defects in the bone or meninges, abnormal development of tissue - spin bifida in spinal cord, anencephaly in the brain • Aneurysms are dilation of an artery at an injury or weak side, usually by the circle of Willis – berry or fusiform, or secondary to hypertension – microaneurysms • Hemorrhage causes violent headaches, blood in the CSF • Subarachnoid vasospasms happen spontaneously or secondary to subarachnoid hemorrhage • Arteriovenous malformation are congenital and can cause ischemia and hemorrhage • Infection or inflammation can cause clots in cerebral veins or venous sinuses • Usually arise from ear, sinuses, scalp, nasal cavity, or the face • Cerebrovascular accidents occur when blood flow is impaired by occlusion or hemorrhage – will affect function controlled by the area • More common in people with hypertension, heart disease, hypercholesterolemia, diabetes, atherosclerosis, oral contraceptive use, smokers • TIA – brief vasospasm of an artery from a developing plaque but are temporary and reversible • Amaurosis fugax with TIA in ophthalmic artery • Thrombotic CVA is from a thrombus on a plaque, usually due to atherosclerosis, asymptomatic until major stenosis blocks flow • Ischemia is followed by infarct & liquefaction necrosis • embolic CVA’s are 2nd most common, usually from a-fib, but also from fractures or tumors - they occur more rapidly • Hemorrhagic CVA can produce a hematoma mass, usually because of hypertension and aneurisms, blood can enter ventricles or subarachnoid space • Bacterial infection of subarachnoid space – pyogenic meningitis – causes stiff neck, fever, vomiting, + Brudzinski & Kernig signs • Nisseria meningitides, streptococcus pneumoniae, hemophilus influenzae most common causes • Other bacteria are syphilis, lyme disease, tuberculosis can affect brain tissue • Viral infections can cause viral meningitis & fatal encephalitis • Varicella & measles virus remains in nervous tissue • Reye’s syndrome is postviral, affects the CNS, seen after aspirin use • Brain abscesses are treated with antibiotics • CNS tumors vary between children & adults • Adult tumors arise in glial cells that still undergo mitosis, secondary metastasis from lung, breast, skin, kidney cancers • Stem cell tumors usually arise in children • Drugs that affect autonomic function produce broad or focused effects by blocking or stimulating receptors • Peripheral nerve injuries can repair, 1.5mm/day; not central lesions because of atrophy and scar tissue • Peripheral nerve injuries decreased muscle tone, weakness or paralysis of voluntary movement, loss of reflexes, muscle atrophy • Upper motor neuron – increased muscle tone, weakness or loss of voluntary movement, increased reflexes, abnormal plantar reflex • Cerebellar lesions cause tremor, difficulty in performing voluntary movements • Basal ganglia lesions cause difficulty initiating movement, tremor or other movements at rest, rigidity • Parkinson disease – from a lesion in the substantia nigra – loss of dopamine - muscle rigidity, bradykinesia, tremor, stooped posture, shuffling gait, autonomic dysfunction • Huntington disease – dominant inheritance – loss of GABA - motor disorder, cognitive impairment, derangement • Cerebral palsy – ante or perinatal lesion to a normal nervous system impairs voluntary control, hyperreflexia, symptoms like either basal ganglia or cerebellar dysfunction • Muscle diseases, usually from genetic or autoimmune disorders, cause muscle weakness • Myasthenia gravis is a disorder of neuromuscular junction, autoimmune loss of neurotransmitter receptors for acetylcholine • Acetylcholinesterase inhibitors allow ACh accumulation to counteract loss of receptors • Multiple sclerosis – sensory, motor, psychic abnormalities from an immunemediated attack on central nervous system myelin that leaves scars called plaques • Guillain-Barre syndrome is immune attack of peripheral myelin • Agents can cause lesions in peripheral nerves • Viatmin B12 deficiency can affect spinal cord function, and alcoholic degeneration Korsakoff’s psychosis • Entrapment syndrome cause focal lesions, with weakness & impaired sensations • Injury to the spinal cord interrupts sensory, motor pathways, with increased reflex activity below the site of the lesion Amyotrophic lateral sclerosis – loss of corticospinal neurons without any cognitive impairment • Autosomal recessive disorders: • Wednig-Hoffmann disease – weakness – floppy baby syndrome • Wohlfart-KugelbergWelander disease - loss of motor supply to proximal muscles • Friedrech’s Ataxia – thin spinal cord affecting movements • Alzheimer disease – progressive loss of cortical neurons, degenerative dementia that affects all mental function • Biopsies show neurofibrillary tangles and neuritic plaques of amyloid • Seizure – rapidly evolving disturbance of brain function that can produce impaired consciousness, abnormal sensations or mental functioning, or convulsive movements • Nonepileptic seizures are secondary to conditions like alcohol withdrawal, meningitis, liver or kidney failure • Epileptic seizures result when a relatively permanent change in the environment, input, or nature of cortical gray matter pyramidal cells allows some of them – the focus – to discharge spontaneously & recruit larger areas • Pyramidal cells are predisposed to generating seizures • Most seizures begin focally and produce temporary recruitment that presents as an aura – mental, sensory, or motor phenomena at the onset;, localized EEG activity, abnormal movements, sensations, consciousness, or psychic function • Prodrome – set of symptoms that warns of an impending seizure • Partial seizures begin at a limited focus • Simple partial seizure can spread to become a complex or generalized (secondarily generalized tonic-clonic seizure) • Complex seizures include an alteration of consciousness, may show automatisms – purposeless behaviors • Generalized seizures arise instantly with no evidence of focal origin • Absence seizures – minor impairments of neural function & consciousness • Tonic-clonic grand mal seizures – begin with prodrome, and have jerks • Normal consciousness depends on sensory stimulation & processing and integrated function of the reticular activating system, cortex, hippocampus • Consciousness is unimpaired in simple partial seizures, impaired in partial complex & specific generalized seizures • Grand mal status epilepticus (tonic-clonic status) is medical emergency • Acidosis, increased CO2, hypoglycemia from muscle contraction, can lead to death • Evaluation of tendency to have seizures involves routine EEG, CT, MRI drug therapy with a single anticonvulsant is usual medical management