Expedited Partner Therapy (EPT) for Gonorrhea & Chlamydial Infection
advertisement

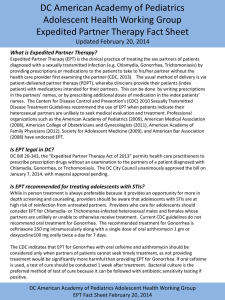
Expedited Partner Therapy (EPT) for Gonorrhea & Chlamydial Infection Matthew R. Golden MD, MPH Center for AIDS & STD, University of WA Public Health – Seattle & King County Overview • Background on development of EPT • Overview of data from randomized trials • Barriers to EPT • Community-level scale-up Gonorrhea — Rates: United States, 1941–2006 and the Healthy People 2010 target Rate (per 100,000 population) 500 Gonorrhea 2010 Target 400 300 200 100 0 1941 46 51 56 61 66 71 76 81 86 91 96 Note: The Healthy People 2010 target for gonorrhea is 19.0 cases per 100,000 population. 2001 06 Chlamydia — Rates: Total and by sex: United States, 1987–2006 Rate (per 100,000 population) 600 Men Women Total 480 360 240 120 0 1987 89 91 93 95 97 99 2001 03 Note: As of January 2000, all 50 states and the District of Columbia had regulations requiring the reporting of chlamydia cases. 05 Chlamydia in Minnesota Rate per 100,000 by Year of Diagnosis, 1992-2007 300 Rate of Chlamydia per 100,000 . 275 250 225 200 273 per 100,000 175 150 125 100 75 50 115 per 100,000 25 0 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 Year Figure 35. Nonspecific urethritis — Initial visits to physicians’ offices by men: United States, 1966–2000 160 Adjusted chlamydia prevalence Gonorrhea incidence 0.14 0.12 140 120 0.1 100 0.08 80 0.06 60 0.04 40 0.02 R2=0.95 0 20 0 GC cases per 100,000 women 0.16 19 88 19 90 19 92 19 94 19 96 19 98 20 00 20 02 20 04 Proportion of positive chlamydia tests Adjusted chlamydia prevalence in Infertility Prevention Project (IPP) clinics & gonorrhea incidence, 1988-2005 Chlamydia — Positivity Rates by Age and Gender MIPP† Clinics, 2002-2007 20% Males, 15-19 Females, 15-19 Males, 20-24 Females, 20-24 Percent Positive (No. positive / No. of tests) 16% 12% 8% 4% 0% 2002 2003 2004 2005 2006 2007 Year † The Minnesota Infertility Prevention Project (MIPP) is a project funded by the CDC to provide STD testing and treatment to uninsured men and women ages 15-24. Participating clinics include STD, family planning, adolescent, and community clinics. Pelvic inflammatory disease — Hospitalizations of women 15 to 44 years of age: United States, 1980–2003 Hospitalizations (in thousands) 200 Acute, Unspec. Chronic 160 120 80 40 0 1980 82 84 86 88 90 92 94 96 98 2000 02 Pelvic inflammatory disease — Initial visits to physicians’ offices by women 15 to 44 years of age: United States, 1980–2004 Visits (in thousands) 500 400 300 200 100 0 1980 82 84 86 88 90 92 94 96 98 Note: The relative standard error for these estimates ranges from 19% to 30%. SOURCE: National Disease and Therapeutic Index (IMS Health) 2000 02 04 Ectopic pregnancy — Hospitalizations of women 15 to 44 years of age: United States, 1980–2003 Hospitalizations (in thousands) 100 80 60 40 20 0 1980 82 84 86 88 90 92 94 96 98 2000 02 16 Racial Disparities in a Probability Sample of American Adolescents 14 14 13.3 12 White Black Latino Asian Native American 10 8 6 4 4.4 2.5 3.3 1.9 2 0.13 0.13 0 Risk Ratio Chlamydia 1.0 5.5 1.8 1.3 5.3 Gonorrhea 1.0 14.6 1.0 JAMA 2004:291:2229 Gonorrhea Rates by Race/Ethnicity Minnesota, 1997-2007 White American Indian Hispanic* 1200 Rate per 100,000 persons . 1000 Black Asian/PI 800 600 400 200 0 1997 1998 1999 * Persons of Hispanic ethnicity can be of any race. 2000 2001 2002 Year 2003 2004 2005 2006 2007 Gonorrhea & Chlamydia in the U.S. Circa 2008 • Gonorrhea rates are very low relative to the 1970-80s • Chlamydia probably dropped with the introduction of screening • Major morbidity from gonorrhea and chlamydia is way down • Burden of disease is now probably roughly stable • Dramatic racial disparities persist • Additional progress will require new approaches Strategies to Improve the Control of Bacterial STD • Primary prevention – behavior change • Primary & secondary prevention - Case-finding & treatment • Increase screening • Rescreening – retest those with an STD at 3 months • Improve partner treatment Partner Notification • Process of notifying the sex partners of persons with an STD and assuring their treatment • Public health authorities developed partner notification programs in the 1940s for syphilis • Public health advisors interview people with STD and notify their partners • Growth in the 1960s and 70s and assumed some responsibility for gonorrhea • Contraction in the 1980s – tentative response to HIV, no response to chlamydia PN: Data from mathematical models Source: Am J Epi 2001;153:90 Percent Interviewed for PN Percentage of Cases of STD/HIV Interviewed for PN in High STD/HIV Morbidity Areas of U.S., 1999-01 & 2006 100 80 1999-2001 2006 10 12 89 87 60 52 40 32 20 17 6 0 Syphilis HIV Gonorrhea Sources: STD 2003:30:490, STD 2004;31:709, unpublished Chlamydia Could We Provide DIS Services To Everyone with a Reportable STD? • ~ 1.5 million cases of HIV, syphilis, gonorrhea, and chlamydia reported annually in U.S. • ~2800 Disease Intervention Specialists (DIS) to provide services to 75% of cases • ~ $200 million annually for DIS • CDC STD budget = $108 million in 2007 Chlamydia partner notification practices among private sector providers in King County (n=150) 100 Percent 80 90 60 40 20 17 0 Source: STD 1999;26:543-7. Told patient to notify partners Knows all partners treated 4 Gave patient medication for partners Outcomes of partner notification for gonorrhea and chlamydial infection by patient referral Number STD % partners evaluated Colorado 1977 93 GC 51% Colorado 1985 3368 GC 62% Canada 1992 37 CT 68% London 1994 254 CT 53% Amsterdam 1997 440 GC/CT 40% Seattle 2001 698 GC/CT 51% Indianapolis 2002 241 GC/CT/NGU/TV 65% France 2002 145 Any STD 49% City (yr) Expedited Partner Therapy (EPT) • Global term for process of treating partners without their mandatory prior examination • Patient delivered partner therapy (PDPT) – index patient gives meds to partners • Most common form of EPT Proportion of women “reinfected” with Chlamydia trachomatis based on partner notification practices: Swedish observational data 15 10 10.2 8.4 5 0 4.8 1.8 No PN Source: Int. J STD & AIDS 1991;2:116 Pt. referral Conditional referral Pt delivered prescription Proportion of patients with chlamydial infection to whom physicians give medications for their sex partners 60 50 40 44 Chlamydia 50 30 Gonorrhea 34 31 20 10 0 8 Never N=2,538 CT N=1,873 GC Sometimes 7 Half 9 7 6 4 Usually Always Source: Sex Trans Dis 2005;32:101 3 RCTs of Expedited Partner Therapy (EPT) Study Multi-city CT in ♀1 Population 1787 Women screened CT+ – mostly FP clinics Intervention Patient-delivered partner therapy (PDPT) Seattle CT/GC2 Populationbased All offered assistance 1) PDPT 2) Partners contacted by hlth. dept. offered direct Rx 2751 Men & Women Outcome - Partner treated* - Infection at 1& 4 months - Partner treated* - Infection at 34 months Follow-up 90% 1 month 55% 3-4 months 68% at 10-18 weeks New Orleans urethritis3 977 STD clinic patients 2 Interventions 1) Informational booklet 2) PDPT - Partner treated* - Infection at 12 months 85% Interview 30% specimen Scotland CT 303 Women in STD, FP and Abortion clinics 2 Interventions 1) PDPT 2) Mailed specimen -Partner treated - Infection w/in 12 months 65% * Partner treatment per participant report in all studies except Scotland Sources: Schillinger et al Sex Transm Dis 2003;30:491, Golden et al NEJM 1992;352:6762, Kissinger et al Clin Inf Dis 2005;41:6233, Cameron ST et al, Num Reprod 20094 Partner treatment per index patient report 100 Percent 80 Standard Expedited P<.0001 83 82 P<.0001 61 60 57 65 50 40 P=.001 20 11 6 0 Talked to partner about STD Partner "very likely" treated All partners treated Sex untreated partner Source: NEJM 2005;352:676 Percent Infection during follow-up among 1860 persons completing the randomized trial 16 14 12 10 8 6 4 2 0 Standard care Expedited care P=.02 P=.17 13.2 13 10.8 10.6 P=.04 9.9 3.4 Gonorrhea Chlamydia N=358 N=1595 Source: NEJM 2005;352:676 Gonorrhea or Chlamydia N=1860 Impact of PDPT on Index Patient GC/CT Reinfection in 4 Randomized Controlled Trials CT in women (CDC multi city trial) GC or CT in men or women (Seattle) Urethritis in men (New Orleans) 0.19 0.8 0.62 0.59 0.76 0.38 0.74 0.54 CT in women (Scotland) 0.1 1.05 0.98 1.32 1 Log Odds Ratio 3.56 10 Impact of PDPT on Index Patient Report that Partner was Treated in 4 Randomized Controlled Trials Study Multi-city CT in ♀ Seattle CT/GC New Orleans urethritis Scottish CT in ♀* PDPT Control P-value 86% 57% 0.001 64% 52% 0.001 56% 34% 0.001 94% 78% 0.02 * Outcome is all partners contacted, not treated Subgroup Analysis: Reinfection Partner Study 12 10 EPT Standard 11.2 10.5 Percent 9.6 8 9.4 9.1 7.4 6 8 7.8 6.6 6.2 6.2 5.1 4 7.4 7.4 7.2 4.2 2 0 Age <=20 Age >20 White African Am 1 sex >1 sex partner partner Relative risks associated with receipt of standard care 1-2-1.8 Sources: Golden et al NEJM 1992;352:6762 (unpublished data) Male Female Subgroup Analysis: Percentage of Partners Treated 100 EPT Standard 80 Percent 77 60 67 63 53 76 65 56 55 48 40 66 66 63 50 56 47 37 20 0 Age <=20 Age >20 1 sex partner >1 sex partner Relative risks associated with receipt of EPT 1-2-1.3 Sources: Golden et al NEJM 1992;352:6762 (unpublished data) Male Female Casual partner Not Casual CDC & Professional Activities Related to EPT CDC Dear Colleague Letter Date 5/05 Expedited Partner Therapy Review & Guidance Document 2/06 American Medical Assoc. Statement on EPT 6/06 Legal Status EPT Evaluation 6/06 STD Treatment Guidelines 8/06 CDC EPT Website 10/6 New Partner Notification Guidelines 2008 Am. Acad. Pediatrics Supports EPT 2008 Barriers • Is this legal, and what is my liability? • Is this an acceptable standard of medical care? • Will EPT promote antimicrobial resistance? • Is this ethical? Legal Status of EPT in the United States WA ME ND MT OR ID MN NY WI SD MI WY PA IA NE NV IL UT CO CA KS OH IN WV VA MO KY NC TN OK AZ SC AR NM MS AL TX GA LA FL AK HI Source: Adapted from Hodge JG. AJPH 2008;98:236 EPT Permissible EPT newly legal EPT Prohibited EPT legal status uncertain EPT under consideration Legal Issues in MN • “Nothing in this chapter prohibits a licensed practitioner from issuing a prescription or dispensing a legend drug in accordance with the Expedited Partner Therapy in the Management of STD guidance document issued by the US CDC.” • CDC recommends that EPT when other management options are impractical or unsuccessful http://www.cdc.gov/std/treatment/EPTFinalReport2006.pdf Legal Issues Information to provide with EPT • Name of original patient sufficient in MN • Information about medications & STD • Advice about complications and need for care (e.g. PID) • Where to seek care Information in MN • MN Dept Health has information sheets on their website that can be distributed with medications http://www.health.state.mn.us/divs/idepc/dtopics/stds/ept/ctinstructions.pdf Liability • You can always be sued • Are you acting in a manner that is consistent with standards of care in your community? • Can you be sued for not providing EPT? Is EPT a Good Standard of Care? • A complete evaluation of all partners would be best • Are we missing concurrent diagnoses? • Are we placing partners at significant risk of adverse drug reactions? STD diagnoses in persons presenting as contacts to gonorrhea, chlamydia or NGU/MPC Seattle, Baltimore, Birmingham and Denver Women (n=2507) Gonorrhea* 3.9% PID 3.7% Heterosexual Men Men who Have Sex with Men (n=3511) (n=460) 3.1% 6.1% NA NA New HIV 0 0.2% 5.5% Early Syphilis <0.1% 0 0.4% * GC excludes contacts to GC. Source: CID 2005;40:787 Adverse Drug Reactions • Anaphylaxis to macrolides is very rare • PCN – Anaphylaxis with cephalosporins is rare (0.10.0001%) – ~10% of people report having a PCN allergy – Cross reactivity to 3rd gen cephalosporins 1-3% – Only avertable reactions are those occurring in persons with a known allergy who take meds despite written warnings • No cases anaphylaxis to date in CA and WA Antimicrobial Resistance • No known chlamydial resistance to azithro • Cephalosporin resistant GC very uncommon is U.S. – Some evidence rising MICs in Japan • Standard of care is to treat contacts to GC & chlamydia without awaiting test results – EPT primarily increases antimicrobial use by increasing appropriate treatment of partners • In 2005, 55 million prescriptions for Azithro; 3 million cases of chlamydia in U.S. Ethics Respect for Patient Autonomy Beneficence Nonmaleficence Justice • Insofar as RCTs show decreased reinfection in index cases given EPT, EPT is a superior standard of care • Is EPT better for the partner? Can partners make an informed decision? EPT Guidelines CDC CA MN WA Heterosexual “Can be used as GC & CT an option when other management strategies are impractical or unsuccessful.” Partners who are “unable or unlikely to seek timely treatment” Most appropriate for partners who are unable or unlikely to seek prompt clinical services. Give if partner treatment “not otherwise assured” MSM GC & CT Should not be considered a routine partner management strategy No different recommendation – acknowledges potential risk Not recommended as routine MSM should be referred to health Dept. Trichomonas Not recommended as routine Not addressed Not recommended as routine Not addressed California State EPT Program • Guidelines promulgated and published (Sex Transm Dis 2007, epub) • Paying for EPT • Medicare waiver to pay for PDPT denied • State bulk purchasing medication for PDPT for Infertility Prevention Program clinics • CDC funded evaluation in family planning clinics CA Family Planning Clinic Evaluation: Association of Treatment Outcome with Management Strategy by Relationship Type Partner Notification Method Employed Patient Referral Bring Partner to Clinic (BYOP) PDPT None Percentage Partners Treated, by Index Case Report 100 80 79 10 77 60 20 54 40 40 20 14 12 0 Source: Yu. 2007 CDC STD Prevention Conference Patient Referral BYOP PDPT None Association of Treatment Outcome with Management Strategy by Relationship Type Partner Management Strategy Steady Partner (n=551) Non-steady Partner (n=404) OR (95%)* OR (95%CI)* BYOP 3.6 (1.8-7.4) 3.5 (1.7-7.0) PDPT 2.8 (1.4-5.4) 6.0 (3.3-10.8) Patient referral 1.4 (0.7-2.6) 2.0 (1.2-3.3) 1.0 1.0 None *OR adjusted for patient’s age and race/ethnicity Source: Yu. 2007 CDC STD Prevention Conference Steps in Developing and Implementing A New Public Health Intervention Evaluate Existing System & Literature on Alternatives Design Intervention Consider Feasibility for Wide-Spread Implementation Individual Level Randomized Controlled Trials Cost-Effectiveness Analysis (relative CEA) Re-Design Intervention for Scale-up Model Population-Level Impact Community-Level RCT Scheme of PN Barriers & Interventions Index patient diagnosed & treated Partner Notified BARRIERS Doesn’t know partner(s) Doesn’t like partner(s) Can’t reach partner(s) Afraid of partner(s) INTERVENTION DIS Partner Treated Access to care (clinic hrs, transportation) Partner asymptomatic - not concerned Pt Delivered Rx Proportion of Patients with Untreated Partners at Time of Study Interview 100 80 60 40 20 + Risk Factor No Risk Factor 0 0 2 4 6 8 10 12 14 Days Between Treatment & Interview Risk factors: > 1 sex partner 60 days or pt does not anticipate sex with partner in future Source: STD 2001;28:658 PN CT & GC: where do we go from here? Association of PN Plan on Case Report Form with PN Outcomes All partners already treated Provider to assure PN Health dept. assistance requested 100 80 60 78 40 20 0 47 42 32 40 6 30 39 16 22 13 11 % Given PDPT by % with Untreated Given PDPT by Increase in Clinician Before Partners Health Dept. Partner Health Dept. Treatment* contact Source: Golden et al. Sex * Limited to persons contacted >7 days after treatment Transm Dis 2007;epub Percentage of Persons with Gonorrhea or Chlamydia in King County Given PDPT by Their Diagnosing Provider 50 40 30 20 10 16 5 0 1998-2002 2004-2005 Use of PDPT remained significantly greater in the 2004-05 (OR 3.2, 95% CI 2.5- 4.1) compared to 1998-2002 after adjusting for diagnosing site, gender, GC vs. CT, and the presence of case report risk factors for PN failure Estimated Percentage of Persons Assuring the Treatment of All of their Sex Partners Among All Cases* of Gonorrhea or Chlamydial Infection in King County 100 80 Percent 64 58 60 40 39 20 0 * Nonincarcerated heterosexuals No Intervention Intervention without Direct Public Health Assistance Intervention Including Direct Public Health Intervention Assessment of Community-Wide EPT: Simulation Model 50% → 60% partners treated Ct prevalence in women (%) 5 4 3 2 1 0 -2 0 2 4 6 8 Years since PDPT introduction 15 realisations, thick line is median. Includes annual Ct screening of 25% of women aged <26. 10% increase in partner treatment results in a ~25% reduction in CT prevalence at 2 years, and a ~50% reduction in 4 years 10 Percent infected Chlamydia Positivity in Women Tested in IPP Clinics in King County and WA State Outside of King County, 1998-2007 9 8 7 5.8 5.5 6 5 5.4 4.9 4 3 EPT 2 RCT Begins 1 0 1998 6.3 5.5 6.2 5.7 6.9 6 7.3 5.7 PHSKC Recommends EPT 2000 2002 Time 7.5 5.9 7.1 7.1 7.7 5.9 5.6 PHSKC Institutes Free EPT and Case-Report Based Partner Notification Triage 2004 2006 5.9 WA State EPT Community-Level Randomized Trial • Stepped-wedge community-level randomized trial • Unit of randomization = health jurisdiction (n=24) • Timing of program institution is randomly assigned as “steps” • Every ~6 months - 1st step 9/07, 2nd step 5/08, 3rd step 12/08 • Intervention • Case-report based triage of cases for assisted partner notification • Free PDPT distributed via large clinics & commercial pharmacies • Case report form has prescriptions preprinted for faxing • Outcome = Prevalence of chlamydia in sentinel clinics (IPP), reported incidence of gonorrhea in women Cases with at Least One Partner Treated via EPT from the Diagnosing Provider, WA State EPT Community-Level Trial Waves 1 and 2 Wave 1 40 Wave 2 Intervention Begins Wave 1 Intervention Begins 30 20 10 0 Ju n07 Ju l -0 7 A ug -0 7 Se p07 O ct -0 7 N ov -0 7 D ec -0 7 Ja n08 Fe b08 M ar -0 8 A pr -0 8 M ay -0 8 Ju n08 Ju l -0 8 A ug -0 8 Percent 50 Wave 2 Preliminary Outcomes: Wave 1 Communities, WA State EPT, Proportion of Partners Notified and Treated Prior Intervention Intervention Period - Prior DIS Interviews Intervention Period - Post DIS Interviews 100 80 73 60 P<.0001 71 40 47 55 38 20 50 0 Notified Treated Outcomes restricted to persons interviewed >7 days post treatment. Adjusted for demographic factors. Conclusions • Expedited partner therapy (EPT) decreases reinfection rates and increases the proportion of partners treated per index patient report • EPT is legal in MN, but requires that you dispense information for partners • EPT can be introduced into a diverse large communities and appears to have a population-level effect on the proportion of all partners treated • The population-level of effect of EPT on the occurrence of STD or STD associated morbidity, like that of other STD interventions, has yet to be proven