Daily Inpatient Care Checklist
advertisement

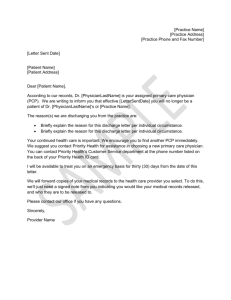
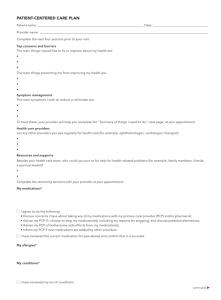
Inpatient Care Checklist Daily rounds- Gather data Review records (H&P, Off service notes, transfer notes, consult notes, nursing notes, allied health care professional notes like PT, OT, dietary etc. and previous DC summaries) Review vital sign, current labs, and radiology tests. Make a note to track test results which may require you to stroll back few days Check overnight orders placed on patient Check med list -Check for expired meds or those about to expire -Check for meds that the patient no longer needs. Those should be DC -Check for meds that he patient should be on but is not getting because it was DC by accident or omitted on admission or transfer Check for duplicate or excess meds in the same category (for e.g. patient may be on scheduled albuterol nebs as well as nebulizer or too many narcotics Does he any medication to be restarted, which was placed on hold for a procedure or for a certain reason? Always keep cleaning out the med list! Check for active DVT prophylaxis Touch base w/ RN re: current issues/events overnight before you walk in the patient’s room Daily rounds-Clinical Care: Write daily progress note If you are copying a previous note make SURE you don’t copy anything that is inaccurate or does not apply to that day any more- Make RN aware of plan for the day Make care Coordinators aware of plan of care Check any labs ordered for the day or pending from a few days ago Check potential barriers for discharge (i.e. Foley still in place, constipation, diet not advanced, diet of the wrong consistency, ongoing pain issues needing IV narcotics, patient on oxygen and needs to be weaned off, mobility not optimized or not at baseline. Check these daily Patient visit and communication Evaluate the patient. Remember to sit and be at an eye level. Introduce yourself every day. Do NOT assume that the patient remembers you from the previous day. Identify your role in his care. Physical exam on daily rounds. Certain systems should be routinely examined Lungs and heart and abdomen frequently get deranged for hospitalized patients Skin- check for edema, erythema on and around any tube/drains in place, check for any decubiti and pressure ulcer and check for any newly made incisions wounds from a recent surgery Always remove the sheets- there could be a fund of information about the patient’s condition when you remove barriers Check for all lines and tubes present including, Texas, Foley, IV site, PICC line, central line, rectal tube, chest tube, any external drainage, and oxygen Examine the abdomen- Frequently gets involved in hospitalized patients with ileus, constipation etc. Assess mental status (identify delirium early) Always clarify that patient understands the plan of care prior to leaving the room Set expectation with the patient. Tell them how frequently will you see them daily, ask who is their spokesperson and tell how frequently will you contact their spokesperson during their hospital stay. Make sure to notify patient and family if you are not rounding the next day Touch base with patients family as needed Discharge Checklist Decide disposition plans and get work ahead of time when possible without having to add too many addendums to the DC instructions, med reconciliation form, DC note and DC summary. These can be too confusing and can be a cause of error. Having addendums are hard to follow for an already compromised patient. Inform the family the ahead of time about DC Complete a DC note or DC summary and other DC paper works at the time of DC and cc to the PCP. In complex cases, call the PCP to alert them that the patient is being DC and what needs to be followed. Complete DC instructions in a patient friendly lingo including instructions about the diagnoses, plan for follow up, any labs or studies need to be followed, instructions on diet and medication, what each medication is being prescribed for and what symptoms to watch out for deterioration at home. Remove confusing items from the DC instruction template (if you are using one) and create a clean, visually friendly DC instructions Check potential barriers for discharge (i.e. Foley still in place, constipation, diet not advanced, diet of the wrong consistency, ongoing pain issues needing IV narcotics, patient on oxygen and needs to be weaned off, mobility not optimized or not at baseline. Check these daily Identify discharges as early as possible and discuss with RN and Care co coordinator Examine patient on the day of DC, answer questions and call appropriate family spokesperson to update. Remember to review items Dc instructions verbally with the patient. Reconcile discharge meds and make sure they match the med list on your DC discharge summary and actual medication med list given to the patient Do discharge prescriptions if applicable. Work on prescriptions based on the system at the institution you are doing your clerkship. Dictate discharge summary should include primary & secondary Dx, procedures and consults obtained, dc meds, brief summary, disposition, plan for follow-up, tests which need to be followed and condition on DC Remember to cc or fax a copy of DC summary to PCP and other involved specialists Call PCP to notify of DC, leave msg with the office if not available especially for patients with complex hospital admission, those who require many complex fup details, who have labs and other tests which need follow up and those who have multiple admissions Admission Checklist Review EMS (ambulance) Flow sheet if appropriate Review ED record Make sure you put in some tuck in orders for the patient to get the care started while you are thinking through your H/P and problem list. For example steroids, nebs and oxygen for a patient with COPD. That way, the patients get prompt care while the admitting team is thinking through in more details. Your documented history should also include where patient came from, what is his/her activity level, what is the code status, who the spokesperson for the patient Remember to send a copy or fax a copy to PCP and other relevant outpatient subspecialty provider Decide what meds to continue, what to hold and make a note to you about medication change plans. If you are going off service, remember to share this information with the incoming provider Dictated H&P should always include where the patient came from (home vs. nursing home vs. assisted living etc.), where they normally get their care, their functional status (activity level), code status and their spokesperson or health care agent who the team should communicate with. Reconcile admission meds Review assessment & plan with patient and appropriate family Place admission orders Review adm assessment & plan with RN Discuss with PCP when appropriate plan of care as appropriate