Patient with shortness of breath
advertisement

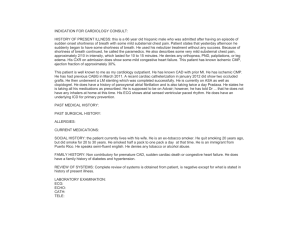
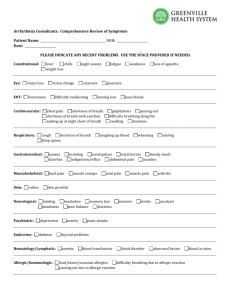
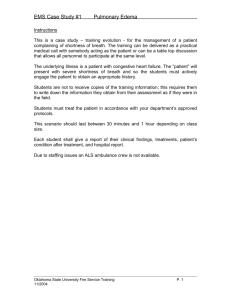
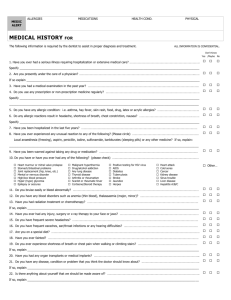
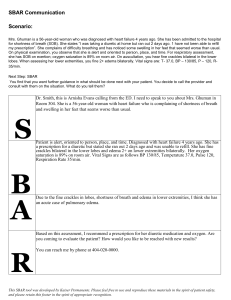
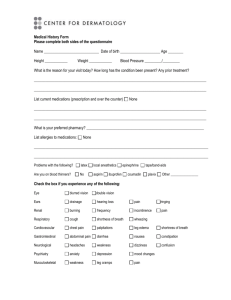
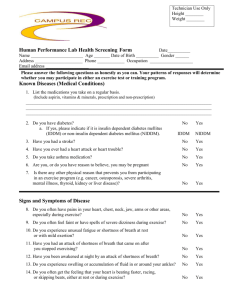
A Patient with Shortness of Breath A 53-year-old man is admitted from the emergency room with shortness of breath (SOB). He had never had this problem until about 2 weeks PTA when he began to notice difficulty breathing when climbing stairs. Last week he began to have SOB when walking less than one block and last night he awoke from sleep and had to get up to "get some air". He denied any fever, cough, hemoptysis, chest pain or discomfort, back pain, urinary abnormalities, abdominal pain or ankle swelling. The patient has visited the Yale Emergency Department on many occasions over the last 15 years. He has a history of hypertension for 10 years and Type II DM diagnosed two year ago. He has been prescribed various medications to help control his hypertension and diabetes but he has been non-compliant and states cannot afford to pay for them. He is currently unemployed, lives in a New Haven shelter, has no health insurance and rarely keeps his clinic appointments in the Primary Care Center. He smokes and drinks alcohol regularly, but he can't quantitate the amount or duration of each. P.E. reveals a thin man appearing older than his age with difficulty breathing. T 976; BP 180/100; P 120 reg; R 36. SKIN - normal turgor without rash or spider angiomata. LN - none palp. HEENT - conj normal. FUNDI - sharp discs; vessels reveal "copper wiring" changes with A-V nicking but no exudates or hemorrhages; oropharynx, TMs and sinuses are benign. CHEST - diminished tactile fremitus with dullness to percussion at both bases about 1/4th the way up posteriorly; breath sounds are diminished at both bases but rales are audible about 1/2 way up bilaterally. COR JVP estimated at 12 cm H2O. PMI is diffuse, sustained and is felt lateral to the anterior axillary line. Ascultation reveals regular rhythm, but tachycardia; S1 is diminished in intensity; S2 is loud and there is evidence for an S4 and S3. There is a 2/6 holosystolic murmur heard at the apex that radiates to the left axillary line and can be heard as far back as the patient's thoracic vertebral spine. Abdomen is soft, without hepatosplenomegaly or evidence for ascites. G/R exam is benign, extremities are without edema and neuro exam is nonfocal. LABS: Na 129, K 3.0, Cl 100, HCO3 22, BUN 30 Cr 1.2, glu 258 Hb 13.0, Hct 38.6, WBC 11.0 UA: clear/1.025/2+ protein/2+ glucose/no ketones EKG: S tach 120/nl intervals/+ for LVH by voltage criteria no ST-T wave changes CXR: heart size enlarged; + Kerley B lines + bilateral alveolar interstitial edema with bilateral pleural effusions ABG (RA) 7.48/28/55 (O2) QUESTIONS: 1. Does this patient have congestive heart failure? If so, what aspects of history and physical exam support the diagnosis of CHF? What other clinical findings would you look for? 2. What are the most common underlying etiologies of systolic heart dysfunction leading to congestive heart failure? What are the most common etiologies of diastolic dysfunction? Which would be most likely in this patient? 3. What is the pathophysiology of the diminished S1, loud S2, and audible S4 and S3 sounds? What is the most likely source of the heart murmur? 4. Is there a role for echocardiography or stress testing for this patient? 5. Identify at least three factors responsible for the patient’s inability to adhere to medical regimen? What steps might you take to assure long term adherence in the future? . 6. What acute medical interventions would you pursue to initially treat the pulmonary edema? 7. What pharmacologic interventions should be considered for therapy on a chronic basis? Which ones have been shown to improve survival for patients with chronic CHF? Does race have an impact on response to therapy?