Evaluation of the San Mateo County Children’s Health Initiative:
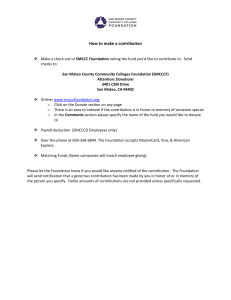
advertisement

Evaluation of the San Mateo County Children’s Health Initiative: Third Annual Report Embry Howell, Urban Institute Dana Hughes, University of California, San Francisco Brigette Courtot, Urban Institute Louise Palmer, Urban Institute September 2006 Submitted to: San Mateo County Children’s Health Initiative Coalition 225 37th Avenue San Mateo, CA 94403 ACKNOWLEDGMENTS We appreciate the help of all the individuals whom we interviewed, including members of the Children’s Health Initiative coalition, school personnel, providers, employers, and community members. We thank Vicky Shih and Min Zheng of the Health Plan of San Mateo, who prepared the data. We especially appreciate the help and support of ST Mayer, Marmi Bermudez, and Sosefina Pita of the San Mateo County Health Department. EXECUTIVE SUMMARY This report, the third in a series of five annual reports from the Evaluation of the San Mateo County Children’s Health Initiative (CHI), provides an overview of the Initiative as well as a detailed look at particular aspects of the program and access to specific services. During 2005 the initiative took on several new challenges, such as an increased focus on improving retention in public programs, increasing use of preventive care, and improving access to dental and mental health care. This annual report provides some new data on several of these and other issues that are important to the continued development of the initiative. Using several data sources, the evaluation investigated issues that are of special interest to the CHI. These include: the demographic and health status characteristics of Healthy Kids served by the CHI; how demographic characteristics and service use have changed over time; characteristics of high cost users of services and how they differ from other children; access to dental services; access to mental health services; the role of schools in outreach and enrollment; and the factors influencing employer decisions to offer insurance for dependents. The data for the analysis come from the annual site visit conducted in October 2005; health plan administrative enrollment and utilization data; and interviews with employers. Key findings include • The growth in the Healthy Kids program continued at a slow pace in 2005, particularly for the youngest children (ages 0–5), despite special efforts to enroll more children in this age group. Growth in the 6–18 age group continued at a moderate pace, creating a challenge to the premium financing for these enrollees. • There was a moderate increase (of 4 percentage points) in the proportion of children who were in the higher income group (250–400 percent of the federal poverty level), and over 13 percent of children continuously enrolled in Healthy Kids from 2003–2004 were in this group. Penetration of coverage within this population was a specific priority for the CHI during the last year. • The use of preventive medical care, as well as dental and vision care, increased from the first to the second year of enrollment in Healthy Kids. In addition, overall use of ambulatory care increased from those who enrolled in 2003 to those who enrolled in 2004. • Ten percent of publicly insured children account for a sizable proportion of expensive medical (although not dental) care, particularly hospital and emergency room care. These children, defined as “high cost users,” account for a substantial portion of the total cost for all children enrolled in the Healthy Kids, Healthy Families, and Medi-Cal programs (39.9 percent, 48.4 percent, and 72.8 percent, i respectively). High cost users are more often chronically ill and have frequent contact with the health care system. Since it is possible to identify them through the claims/encounter data, this group could be targeted for more intensive contact by Certified Application Assistors (CAAs) or health plan staff, to assure that they are receiving coordinated care and that they have good access to the specialty care that they need. This might have the additional benefit of reducing high cost emergency room and hospital care. • About 40 percent of Healthy Kids enrollees do not use dental services, indicating potential access problems and the need to educate parents about the importance of such care. Still, a relatively high percentage of the youngest children (ages 0–5) used services. In addition, Healthy Kids enrollees are more likely to visit a private dentist than to utilize public providers. This finding is in contrast to a widely held perception that access to private dental providers for publicly insured children is limited in the county. • Children with mental health diagnoses are much more expensive than their peers, and these higher costs pertain to both mental health and other health services. Not all children receiving mental health services under Healthy Kids or Healthy Families are having their care coordinated by the San Mateo Health Department Mental Health Services department, but those who are in that system are the most expensive children. • School-based outreach and enrollment assistance is a high priority for the CHI. The increased proportion of Healthy Kids enrollees who are from higher income families is likely a result of this school-based approach, which may reduce the stigma of applying for a public program. Because of the variation in intensity and type of school-based outreach/enrollment from school district-to-district, the CHI could learn from this variation by documenting which districts yield the greatest number of applications and new enrollees. • Based on a limited sample of employer interviews (and complementing similar findings from the evaluation’s client survey and focus groups with parents), there is no evidence that employers of low wage workers have altered policies relating to offering insurance coverage to dependents because of the availability of public coverage for low income children in San Mateo County. In the coming year, the evaluation of the San Mateo CHI will collect new data to address a range of evaluation questions. The second wave of the client survey is currently underway, with an over-sample of children ages zero to five. Data from this survey will be used to measure the impact of the Healthy Kids program on access to care, use of services, and health status. The survey will also provide information on prior insurance coverage and parent satisfaction with the program. In addition, another site visit and two client focus groups will provide qualitative information to help monitor the progress of the CHI and interpret the findings from the client survey analysis. Administrative data on enrollment trends will also be analyzed. Finally, the data from the Health Plan of San ii Mateo, such as that included in this annual report, will be used to continue to monitor trends in enrollee characteristics and use of services across the three public health insurance programs for children in San Mateo County. iii Contents Chapter 1: Introduction....................................................................................................... 1 Chapter 2: The Context and Implementation of the CHI In 2005 ...................................... 3 Chapter 3: Who is Served by the San Mateo County CHI? Have Demographic Characteristics and Service Use Changed Over Time? .................................................... 12 Chapter 4: Who Are the High Cost Users of Services and How Do They Differ From Other Children Enrolled in Public Health Insurance Programs? ...................................... 20 Chapter 5: Do Healthy Kids Enrollees Obtain Needed Dental Health Services? What Barriers Restrict Access? .................................................................................................. 30 Chapter 6: Do Healthy Kids Enrollees Obtain Needed Mental Health Services? What Barriers Restrict Access? .................................................................................................. 38 Chapter 7: What Is The Role Of Schools In Outreach And Enrollment? ......................... 49 Chapter 8: What Factors Are Associated With Employer Decisions To Offer Private Insurance Coverage To Low Wage Workers In San Mateo County? Has The CHI Affected Employer Decisions? ......................................................................................... 55 Chapter 9: Conclusions and Recommendations ............................................................... 61 References ......................................................................................................................... 67 Appendix A: Research Questions of the Evaluation of the San Mateo Children's Health Initiative iv Chapter 1: Introduction The San Mateo Children’s Health Initiative (CHI) was launched in 2002, with a goal of assuring that all children in the county have health insurance. To further this goal, a new locally- funded Healthy Kids insurance program began in February 2003 to cover children up to 400 percent of the federal poverty level who are not entitled to private or other public insurance. The CHI also conducts outreach and enrollment for two other public insurance programs, Medi-Cal (Medicaid) and Healthy Families (SCHIP). The San Mateo County initiative is one of several similar initiatives being implemented in other California counties, including Los Angeles, Santa Clara, and San Francisco Counties among others. The CHI partners decided to evaluate their program over the first five years of the initiative. There are ten major research questions for the evaluation. During each year different sources of information are available to address different questions, and some questions will receive more attention than others over the course of the evaluation. 1 This year’s annual report addresses several evaluation questions and subquestions, including the following: 1 • Who is served by the San Mateo CHI? Have demographic characteristics and service use changed over time? • Who are the high cost users of services and how do they differ from other children enrolled in public health insurance programs? • Do Healthy Kids enrollees obtain needed dental services? What barriers restrict access? • Do Healthy Kids obtain needed mental health services? What barriers restrict access? Appendix A provides the full list of evaluation questions and the evaluation years when each is addressed. 1 • What is the role of schools in outreach and enrollment? • What factors are associated with employer decisions to offer private insurance coverage to low wage workers in San Mateo County? Has the CHI affected employer decisions? The data sources to answer these questions include information from interviews conducted with key stakeholders during the annual evaluation site visit of October 2005 and tabulations from claims/encounter data for children enrolled in the Health Plan of San Mateo for all three public programs (Healthy Kids, Healthy Families, and Medi-Cal). As the evaluation proceeds over the remaining two years, different data collection activities will occur each year, allowing for different types of analyses. The following chapters include, first, an update of the implementation of the San Mateo CHI during 2005 as well as state and local economic and policy issues that affect the CHI. This is followed by a series of chapters addressing each of the six evaluation sub-questions listed above. The evaluation is being conducted under contract with the Urban Institute, consultant Dana Hughes of the University of California San Francisco (UCSF), and subcontractors Mathematica Policy Research and the Aguirre Group. This is the third annual report to the San Mateo Children’s Health Initiative (CHI) partners. More detail on the early years of the San Mateo County CHI can be found in the First 2 and the Second 3 Annual Reports. 2 3 The First Annual Report can be accessed at http://www.urban.org/url.cfm?ID=411003 The Second Annual Report can be accessed at http://www.urban.org/publications/411240.html 2 Chapter 2: The Context and Implementation of the CHI in 2005 County and State Economic and State Policy Context. Although the local economy has not recovered completely from the major economic downturn in the early 2000s, at the time of the annual site visit the economic health of San Mateo had improved substantially over the previous year. For example, by 2005 the unemployment rate was only four percent, down from 4.5 percent in 2004 and 5.2 percent in 2003 (San Mateo County Controller 2006). Meanwhile, the economic health of the state also continued to improve. The state’s revised spending plan for 2006-2007 reflects a significant improvement in the state’s fiscal condition, largely due to higher than anticipated 2006-2007 revenue collections. Consequently, the May Revise (the document that modifies the original January budget proposal) proposed some health care expansions, including a moderate increase in health coverage to nearly 24,000 uninsured children for the 18 counties with waiting lists for Healthy Kids programs. In the final budget negotiations in June, however, this provision was removed from the budget. The budget did include increased payments to Certified Application Assistors (CAAs) who help enroll children Healthy families from $25 to $50 per successful application and rate increases for Medi-Cal managed care plans to offset the five percent reduction in rates approved by the Legislature as part of the 2003-2004 budget agreement (California Budget Project 2006). The recent budget negotiations are part of an on-going debate in California regarding state support for expanded children’s health insurance. During 2005 a bill was approved by both branches of the legislature that would have made Healthy Kids a statewide program by expanding Healthy Families to cover all children (including the 3 undocumented) with incomes up to 300 percent of the federal poverty level (similar to the recent provision that was dropped from the budget). However, the governor vetoed this 2005 legislation for cost reasons. Most recently, a ballot initiative (The Tobacco Tax Act of 2006) to achieve the same aim won sufficient signatures to be placed on the November 2006 ballot. At the time of this writing, its prospects remain uncertain. The Health Plan of San Mateo. The Health Plan of San Mateo (HPSM—which administers the Healthy Kids program for the CHI) experienced severe financial difficulty during the first two years of the CHI, but during 2005 the finances stabilized significantly, in part because of the new Medicare Advantage program. Increased revenue from this program has helped to fund staff expansions in the member services department. With this additional staff, HPSM is taking on more responsibility for health education and renewal for Healthy Kids enrollees. HPSM staff plan to contact families with a welcome call, as well as with phone calls to learn about whether the parent is having difficulty accessing their primary care physician, especially if there is no evidence of a visit within 120 days of enrollment. In addition, the HPSM now sends out quarterly mailings to monitor address changes. Mailings are sent First Class so that the health plan gets a change of address notification from the post office if the family has moved. Personnel Changes. All three of the key organizations that have formed the core staff for the CHI experienced personnel changes during 2005. However, since many of the individuals with new CHI responsibilities have been involved in the CHI in various capacities for some time, there is essential continuity of leadership. 4 Maya Altman was appointed to be Executive Director of the HPSM in June. She formerly served as the Director of Finance and Administration of the San Mateo County Heath Department, and she is familiar with and supportive of the CHI. At the Health Department (formerly the Health Services Agency), Charlene Silva replaced Margaret Taylor as the department director. Srija Srinivasan, previously of the Peninsula Community Foundation, assumed many of Toby Douglas’ prior responsibilities as the new Director of Policy, Planning, and Promotion. ST Mayer moved into the new Health Policy, Planning and Promotion unit. Marmi Bermudez, as the new Program Manager, assumed operational responsibility for CHI outreach and enrollment efforts, as well as the CHI Oversight Committee and fundraising. There have also been some changes in leadership in the Human Services Agency. Maureen Borland retired as agency director, and Glen Brooks was acting in her role at the time of our site visit, with Elsa Dawson assuming his previous position. Shannon Speak has since taken over Elsa Dawson’s prior responsibilities. CHI Financing. Table 2-1 shows funding for the CHI for 2005. There is substantial consistency between the amount and sources of funding between 2004 and 2005, with approximately $7.2 million being raised to fund the CHI in both years. However, for 2005 a higher percentage was spent for premiums than in 2004, when more of the funds were used for outreach. The diversity in funding sources continues. (See the Second Annual Report for more detail on funding levels and sources for 2004.) The San Mateo CHI is facing near-term financial difficulties. While funding for the CHI is available for 2006-2007, funding for children ages 6 to 18 is uncertain beyond that time. (First 5 funding for children five years of age and younger is secure for 10 5 years.) The CHI’s unstable funding situation for older children is the major factor behind the CHI partners’ enthusiastic support for the upcoming ballot initiative that would enact a statewide Healthy Kids program. Table 2-1: Funding for the San Mateo County CHI, 2005 Funder Premium Funding Foundations: David and Lucile Packard Foundation United Way Bay Area Kaiser Foundation Lucile Packard Foundation for Children's Health California Endowment Blue Shield Lucile Packard Children's Hospital California Healthcare Foundation Sub-total, Foundations Healthcare Districts: Sequoia Healthcare District Peninsula Healthcare District Sub-total, Healthcare Districts First Five Commission San Mateo County $1,350,000 $682,250 $2,032,250 $950,000 $2,700,000 Total Funding $6,232,250 $250,000 $100,000 $100,000 $100,000 $550,000 Non-Premium Funding Total Funding $88,200 $71,464 $25,000 $88,200 $71,464 $25,000 $15,000 $15,000 $250,000 $100,000 $100,000 $100,000 $749,664 $199,664 $813,902 $1,013,566 $1,350,000 $682,250 $2,032,250 $1,763,902 $2,700,000 $7,245,816 In spite of this generally problematic future for CHI funding, there have been a few new sources of funding that have become available during 2006 to ease the strain on funding premiums for children ages six to 18. Because the cost of services for Healthy Kids enrollees has been lower than originally anticipated, the HPSM is returning 80 percent of any excess revenues it generates to the CHI. (Almost $2 million was refunded by the time of the site visit in late 2005.) The excess revenue for children ages six to 18 is being placed in a trust fund to cover additional children ages six and older. As a result of this and other new funding, the CHI has avoided a cap on program enrollment. However, these funds may or may not be available in the future. 6 A second source of ne w revenue is from Assembly Bill 495, which authorized a waiver that provides federal matching funds for children with family incomes from 250 to 300 percent of the federal poverty level who otherwise meet the Healthy Families eligibility requirements. The county is in the process of filing a retrospective claim to the state for over $350,000 to cover the federal match for these children since 2004. They have requested approval from the federal government to file a claim for 2003 (which is needed since the time period for billing is usually two years). A third new source of revenue for outreach/enrollment activities is Medi-Cal Administrative Activities (MAA) funding. These funds cover some of the outreach conducted by the San Mateo Medical Center (SMMC) and the Health Department’s Community Health Advocates (CHAs). However, at the time of the site visit, the funds had yet to be distributed to the county. MAA funding is estimated to be about $300,000 per year, more than initially anticipated. Governance. There are no changes in the governance structure described in previous reports, and the same organizations are represented on the CHI Oversight Committee. The faith community, through Peninsula Interfaith Action, has become more involved in the CHI, particularly the lobbying efforts for universal statewide coverage for low- income children. Outreach/Enrollment. No major changes have occurred in the methods of outreach and enrollment. The number of outreach contractors is now six (California Health Initiative, North Peninsula Neighborhood Services, Ravenswood Family Health Center, Redwood City School District, Child Care Coordinating Council, and Cabrillo Unified School District), all of which have a regional focus. Each of these contractors 7 also now receives additional small grants to support retention efforts and enrollments in the county’s Adult Indigent Programs. Some new Community Health Advocates (CHAs) have been added to both the SMMC and Health Department staffs. While they were primarily added to enroll adults in the WELL 4 program, they also do enrollment for the children in the family. Healthy Kids Program. The design and structure of the Healthy Kids program has remained largely the same as when the program began, except for an increase in the premium for children in the 200-250 percent of poverty category, from $6 to $12, to be consistent with the Healthy Families’ new premium structure. In addition, as of February 2005, the Human Services Agency no longer collects the family premium; instead, the family is sent an invoice by the HPSM. This change has reduced the processing time for enrollment from six weeks to five days. (A child may be enrolled for 60 days without a premium payment.) Figure 2-1 shows enrollment trends for the Healthy Kids program. There was a gradual increase in the number of children enrolled in Healthy Kids during 2005, with the number of young children (ages 0–5) growing slightly from 853 in January 2005 to 901 in January 2006, and the number of older children growing from 4548 to 5018 in the same period. Since then, the growth has continued in the number of older children, so that current enrollment in that age group exceeds the number of children originally budgeted for the program. Unlike most other California counties with Healthy Kids programs, the San Mateo CHI has avoided an anticipated program cap for the older children because 4 WELL stands for Wellness - Education - Linkage - Low cost. It is a program to provide health care services for uninsured adults who are served in the San Mateo Medical Center and affiliated public clinics who meet certain eligibility criteria. 8 growth continues to be gradual and because some new sources of funding were identified to cover the additional children as described above. Figure 2-1: Number of San Mateo Healthy Kids Enrollees by Age 7000 6000 Numbers Enrolled 5000 4000 3000 2000 1000 Ma y-0 5 M ar -0 5 Ja n-0 5 No v-0 4 Se p-0 4 Ju l-0 4 Ma y-0 4 M ar -0 4 Ja n-0 4 No v-0 3 Se p-0 3 Au g-0 3 Ju n-0 3 Ap r-0 3 Fe b03 0 Month of Enrollment 0 to 5 6 to 18 Total One-e-App. One-e-App is on- line software to process all applications for Healthy Kids, Medi-Cal and Healthy Families. The purpose of One-e-App is to streamline application preparation and processing and provide a single application for all three programs. At the time of our second site visit in October 2004, One-e-App was not yet operating as a streamlined alternative to paper applications for Medi-Cal and Healthy Families. A year later, it was fully operational in the county and used by all application 9 assistors in all locations. Indeed, the county was awarded a “2005 County Challenge Award” by the California Association of Counties for the implementation of One-e-App. Although One-e-App is becoming more complex as more counties adopt it, since each county has unique desired features and programs, those interviewed in San Mateo remain very enthusiastic about it. Healthy Kids Renewal. In the past year, the CHI has placed great emphasis on improving renewal rates, which have been lower than expected. However, it has been difficult to develop consistent data over time, making it difficult to monitor progress. One of the possible reasons for lower than expected retention is the lack of centralized or shared responsibility for renewals. At the time of the site visit the HPSM was beginning to assume more responsibility for renewal. Another policy change is currently under consideration that would require dropping the child from Healthy Kids if the family cannot be contacted by mail. A new small grant from the California HealthCare Foundation will develop more consistent longitudinal data on retention rates over time. These will be available in future reports. Hardship Fund. A hardship fund covers the Healthy Kids premiums of families who cannot afford them. During 2005 the One-e-App system was changed so that the system prompts the application assistor to inform the parent about the fund’s availability, for families with incomes below 150 percent of the federal poverty level who elect to pay quarterly. (The fund is available to other families, but it is not actively advertised.) As a result of this broader advertising, use of the hardship fund has increased. There were 550 children receiving premium assistance from the hardship fund at the time of our visit. 10 Provider Network. New efforts are being made to develop stronger relationships with primary care providers (PCPs). The Provider Relations Department of the HPSM regularly reviews how many PCPs have signed up with the plan comparing that to the number of members to assure adequate capacity. Despite this, difficulties remain in engaging providers, especially bilingual clinicians, largely due to low reimbursement rates. In March 2006, however, providers serving Healthy Kids and Healthy Families enrollees received an increase in their HPSM reimbursement rates (the health plan now pays these providers 133 percent of the Medi-Cal fee schedule, an increase from 123 percent of the fee schedule). 11 Chapter 3: Who Is Served by the San Mateo County CHI? Have Demographic Characteristics and Service Use Changed over Time? Demographic Characteristics. There was substantial consistency in the demographic characteristics of the children enrolled in Healthy Kids in the first two years of the CHI. Table 3-1 compares the demographic characteristics of the children who enrolled in calendar year 2003 (the first year of Healthy Kids) to those who enrolled in the second year (2004). Healthy Kids enrollees are also compared to Healthy Families and Medi-Cal children who were newly enrolled in the HPSM in 2004. 5 The age profile for children in the Healthy Kids program remained stable between 2003 and 2004. In spite of efforts to reach out to children below age six and enroll them in Healthy Kids (where premium funding is secure), the proportion in that age group remained at just over 20 percent, lower than initially anticipated. The children enrolling in Healthy Kids and Healthy Families in 2004 were older on average than Medi-Cal enrollees, with the large majority of children in both programs being over age six (78 percent for Healthy Kids and 64 percent for Healthy Families in 2004), in contrast to Medi-Cal where only 38 percent of children were age six and older in that year. Additionally, Healthy Kids continues to serve more adolescents than the other two programs (33.7 percent of enrollees, compared to 18.9 percent for Healthy Families and 15.8 percent for Medi-Cal in 2004). These age differences in the programs are consistent with program eligibility guidelines. Medi-Cal has more generous income levels for the youngest children, and consequently, more young children are enrolled in Medi-Cal. In 5 All Healthy Kids and Medi-Cal children must enroll in HPSM in San Mateo County, while Healthy Families parents may or may not choose the HPSM for their child. 12 addition, those born in the U.S. are citizens and therefore entitled to Medi-Cal or Healthy Families. Table 3-1: Demographic Characteristics Children Continuously Enrolled in the Health Plan of San Mateo 2003-2004 Percent Healthy Medi-Cal Healthy Kids Families Cohort 1 (Enrolled Cohort 2 (Enrolled (Enrolled in 2004) in 2003) in 2004) Age 0 1-5 years 6-12 years 13 years and above 0.7 21.4 44.5 33.4 1.3 20.6 44.4 33.7 0.9 35.4 44.8 18.9 34.4 27.4 22.4 15.8 Ethnicity/Language Latino Spanish 86.6 84.7 74.2 59.2 - Income < 150 percent of FPL 150-200 percent of FPL >250 percent of FPL 76.7 14.0 9.3 75.8 10.6 13.3 - - Documented 6.7 12.4 - - 4,378 2,313 919 7,299 N Note: Each cohort includes children enrolled during the year who stayed enrolled for one full year following enrollment Table 3-1 also shows ethnicity/language for children enrolled in the three public programs. Exact measures differ by program; for Healthy Kids and Healthy Families we show the family’s preferred language (for receiving materials, applications, etc.). This is Spanish for 84.7 percent of Healthy Kids enrollees in 2004, a percentage that did not change substantially between the two years, and somewhat less (74.2 percent) for Healthy 13 Families enrollees. For Medi-Cal, the measure is self-reported ethnicity, which is Latino for about 60 percent of enrollees. Income and documentation status are available for Healthy Kids enrollees, and there appears to be a small shift in the composition of enrollees according to these measures. While only 9.3 percent of enrollees who joined the program in 2003 had family incomes above 250 percent of the Federal Poverty Level, the percentage in that income group increased to 13.3 percent among 2004 enrollees. Consistent with this slight shift in the income distribution for Healthy Kids is a shift towards a higher percentage of children who are documented (according to HPSM records), from 6.7 percent for the 2003 cohort to 12.4 percent for 2004. This, combined with the shift in income, suggests that targeted CHI outreach and enrollment efforts (for example, the school outreach discussed later in Chapter 7) are reaching more of their intended clients, including higher income children, who have been particularly difficult to reach through Children’s Health Initiatives in San Mateo County and other counties. Service Utilization. To examine trends in service use under the three public programs, we examined annual rates of use for the two cohorts described above for Healthy Kids. The first cohort is children who enrolled between February and December 2003. The second cohort is children who were newly enrolled in 2004. For Healthy Kids cohort 1, we examined use rates during the first year of enrollment as well as during their second year (for those who remained enrolled). For cohort 2, we examined use rates during the first year of enrollment. These rates are compared to use rates in the first year of enrollment for children who enrolled in the HPSM under both Healthy Families and Medi-Cal during 2004. 14 The CHI has a goal of increasing preventive care service use among children enrolled in public programs, particularly Healthy Kids. Last year’s annual report showed that preventive care service use was low early in the program. Those interviewed during the annual site visit emphasized that increasing use of preventive care services is a major goal for the CHI. Some felt that many parents are unfamiliar with the importance of preventive care. As a result, the HPSM instituted a plan to contact families on a regular basis, including calling if there is no evidence of services received within the first 120 days after enrollment. The HPSM also attempts to encourage preventive care by offering a higher provider reimbursement rate for the first physical examination. Finally, the newsletter (which goes out to all members) provides health education messages that encourage preventive care visits. In addition to these efforts by the HPSM, most CAAs go over a newly designed New Member Packet with families at the time of enrollment. The packet provides preventive care information and discusses the renewal process. Figure 3-1 reveals potentially positive trends in preventive care service use from this increased parental education. As shown, the annual rate of preventive care climbed for Healthy Kids between the first year of enrollment of Cohort 1 and the first year of enrollment of Cohort 2. Additionally, use of preventive care increased between the first year and second year of enrollment from 33.7 to 37.9 percent of children having an annual preventive care visit. This suggests that there may be an educationa l effect that takes some time for parents to absorb and that does not become evident until the second year of enrollment. Healthy Kids children who enrolled in 2004 still had a lower rate of use of preventive care than for Healthy Families, although the gap is less than for 2003 as 15 reported in last year’s annual report. The Healthy Kids preventive care use rate was similar to Medi-Cal, even though Medi-Cal children are younger on average and should be receiving higher rates of preventive care according to professional guidelines. 6 Percentage with a visit in year Figure 3-1 Percent of Children Having A Preventive Care Visit in a Year Children Continuously Enrolled in the Health Plan of San Mateo 2003- 2004 60 54.6 50 40 37.9 40.4 39.6 33.7 30 20 10 0 Healthy Kids Cohort 1, Year 1, 2003 Healthy Families Cohort 1, Year 2, 2004 Medi -Cal Cohort 2, Year 1, 2004 Annual service use of all types of ambulatory care (including care for sick children) increased from the first year of enrollment for Healthy Kids (Figure 3-2). As shown last year, use of any ambulatory care was substantially higher than the use of preventive care, and approached national norms. 7 Presumably some sick care visits also include preventive services. 6 CHDP claims/encounter records are included in the data. However, there is a lag in the inclusion of CHDP claims in the HPSM files. This could explain in part the low Medi-Cal preventive care use. 7 In 2000 78.6 percent of all U.S. children had an ambulatory care visit. (National Center for Health Statistics 2003) 16 Figure 3-2: Percent of Children Having An Ambulatory Care Visit in A Year Children Continuously Enrolled in the Health Plan of San Mateo 2003-2004 90 Percentage 80 81.5 69.3 72.5 77.4 73.8 70 60 50 40 30 20 10 0 Healthy Kids Healthy Families Cohort 1, Year 1, 2003 Cohort 1, Year 2, 2004 Medi-Cal Cohort 2, Year 1, 2004 If preventive and primary care are used appropriately, emergency room use could decline. There is no evidence this trade off in the trends shown in Figure 3-3, since there was almost no change in emergency room use over time for the Healthy Kids program. Still, as observed in last year’s annual report, Healthy Kids use of emergency rooms remains substantially below use in the other two public programs. Figure 3-3: Percent of Children Having An Emergency Room Visit in a Year Children Continuously Enrolled in the Health Plan of San Mateo 2003-2004 35 31.5 30 Percentage 25 20 16.4 15 12.5 12.7 12.5 10 5 0 Healthy Kids Cohort 1, Year 1, 2003 Healthy Families Cohort 1, Year 2, 2004 Medi -Cal Cohort 2, Year 1, 2004 17 The higher rates of emergency room use for Medi-Cal children than for children in the other two programs may not be completely due to overuse of the ER. Medi-Cal children are younger and in poorer health, as shown in last year’s annual report. Healthy Kids is providing new coverage for dental and vision care for most of the children in the program. Figure 3-4 shows trends in dental and vision care use for the Healthy Kids cohorts (complete data are unavailable for the other programs). As with preventive care use, the use from Cohort 1 increased in their second year of enrollment. Figure 3-4: Percent of Children Having Dental and Vision Visits in a Year Children Continuously Enrolled in Healthy Kids 2003-2004 70 62.9 60 55.8 55.9 Percentage 50 40 30 20 8.3 10 9.6 8.9 0 Dental V isit Cohort 1, Year 1, 2003 Vision Visit Cohort 1, Year 2, 2004 Cohort 2, Year 1, 2004 For example, use of dental care increased from 55.8 percent of children having a visit in the first year to 62.9 percent in the second year. The rates for vision care increased from 8.3 to 9.6 percent. This is also good news, since these are critical services and educational efforts may also be playing a role in the increase in use. On the other hand, use for the first years of Cohorts 1 and 2 did not change very much. The data also show that dental 18 visits are more common than preventive care visits, and approach the level of use of any ambulatory medical care. Conclusions. In conclusion, there is substantial stability in the types of children enrolling in Healthy Kids. However, Healthy Kids enrollees differ from Healthy Families and Medi-Cal children, with Healthy Kids enrollees being older and more often Spanishspeaking. The profile of Healthy Kids enrollees is shifting over time in small ways. For example, it appears that some higher income, documented families are learning about the program and enrolling their children. It will be important to continue to track these trends over time. While there is also substantial similarity in use of services over time, it appears that Healthy Kids enrollees use more preventive care (as well dental and vision care) during their second year of enrollment. In addition, the use of preventive care is increasing over time, since the children enrolled in 2004 had higher rates of preventive are than those enrolled in 2003 (although rates remain lower than desirable). 19 Chapter 4: Who Are the High Cost Users of Services and How Do They Differ From Other Children Enrolled in Public Health Insurance Programs? Other studies have shown that a small proportion of users of services account for a large proportion of the cost of health care. For example, an early study of this issue showed that the top 10 percent of users in cost nationwide accounted for 75 percent of all the cost for the non- institutionalized population (Garfinkel et al. 1998). Since chronic conditions—such as mental health problems (Buck et al. 2003) and other chronic conditions (Kozyrskyj et al. 2005)—are more prevalent in the high cost group, there have been special managed care initiatives for the high cost population in order to improve quality and continuity of care, as well as reduce cost. Less is known about the profile of children who are high cost users, but an analysis of San Mateo CHI evaluation client survey data showed that about ten percent of the children enrolled in Healthy Kids had six or more doctor visits in the six months prior to the survey, suggesting that some children are experiencing chronic illness and frequent use of services. Consequently, learning more about their health conditions, service use, and cost may help to identify ways to address their particular needs under managed care. In order to study this issue further, we requested tables for children continuously enrolled in Healthy Kids during the period July 2003 to June, 2004 in order to compare the diagnoses, use, and cost for the high cost children to other Healthy Kids service users. The HPSM summarized the cost per child across all Healthy Kids users, and sorted the data, in order to identify the children who fell into the top 10 percent of cost (called the “high cost user”) group. It is important to note that the tables apply only to users of 20 services (and therefore those with some cost), as opposed to all enrollees as did the tables in the previous chapter. Figure 4-1 High Cost Users and Other Users Children Continuously Enrolled in the Health Plan of San Mateo July 2004 - June 2005 60 57.1 55.5 52.1 53.3 52.0 50.5 50 Percent Male 40 30 20 10 0 Healthy Kids Healthy Families High Cost Children Medi-Cal Other Children Using this method, there were 220 high cost users in Healthy Kids during the time period, which is approximately 10 percent of users, compared with 1973 other users (90 percent). The number of children for Healthy Families was 107 high cost users (10 percent) and 956 other users (90 percent), and for Medi-Cal it was 1,092 high cost users (10 percent), and 9,828 other users (90 percent). Demographics. High cost children in all three public programs are more often boys (figure 4-1). There has been little data from previous research to show that boys are more expensive than girls under public health insurance programs. The consistency in this pattern across programs suggest that this is an area for further study, in order to 21 understand the special health care needs of boys that lead to higher costs. Adolescents are also more often in the high cost group (figure 4-2) than are other children. This distinct pattern is also consistent across all three public programs. Percent Adolescent (13+) Figure 4-2: Percent Adolescent (Age 13+) High Cost Users and Other Users Children Continuously Enrolled in the Health Plan of San Mateo July 2004 - June 2005 45.0 40.0 35.0 30.0 25.0 20.0 15.0 10.0 5.0 0.0 41.8 31.4 24.3 26.1 22.6 16.8 Healthy Kids Healthy Families High Cost Users Medi-Cal Other Users However, as figure 4-3 shows, the ethnicity differences between high cost and other users vary according to program. For Healthy Kids, an almost equal percentage of both groups are Spanish-speaking (about 85 percent). In the Healthy Families program, the proportion of high cost users who speak Spanish (71.8 percent) is also similar to the proportion for low cost users (78.1 percent). For Medi-Cal, a lower proportion of high cost users are Latino (49.5 percent) than are users (62.7 percent). (Data on language spoken are not available for Medi-Cal.) 22 Figure 4-3: Percent Latino/Spanish Speaking High Cost Users and Other Users Children Continuously Enrolled in the Health Plan of San Mateo July 2004 - June 2005 100.0 Percent Latino or Spanish Speaking 90.0 85.0 87.5 78.1 80.0 71.8 70.0 62.7 60.0 49.5 50.0 40.0 30.0 20.0 10.0 0.0 Healthy Kids (% Spanish Speaking) Healthy Families (% Spanish Speaking) High Cost Users Medi-Cal (% Latino) Other Users Diagnoses. Table 4-1 shows the prevalence of selected diagnoses for high cost users and other users for all three programs. We differentiate diagnoses that are generally more acute from those that generally require chronic care. The most prevalent conditions among high cost children include some acute conditions (infectious disease, otitis media, and skin disorders)—all of which are also relatively prevalent among other children—and some chronic conditions (asthma, endocrine disorders, and mental disorders), which have lower prevalence among the other children. The prevalence of acute conditions is usually higher for the highest cost children, but not always. In contrast, the prevalence of chronic conditions is at least twice as high for high cost users, and often the disparity is much greater. This is especially the case for some serious conditions such as congenital anomalies, diabetes, and neoplasms, which are very rare for children who are not in the high cost groups. 23 Table 4-1: Prevalence of Selected Diagnoses Children Continuously Enrolled in the Health Plan of San Mateo July 2004 to June 2005 Healthy Kids High Cost Users Acute Conditions Tuberculosis Other Infectious Disease Fractures Otitis Media Skin Disorders Wounds Chronic Conditions Asthma Congenital Anomalies Diabetes Other Endocrine Disorders Mental Disorders Neoplasms Healthy Families Medi-Cal Percentage with Condition High High Other Cost Other Cost Other Users Users Users Users Users 4.4 11.2 3.9 9.3 14.1 3.9 7.3 8.9 1.1 5.2 8.1 1.2 0.0 18.8 2.0 10.9 14.9 4.0 1.0 8.0 2.6 4.4 11.3 1.2 0.5 17.8 5.4 16.7 15.3 2.8 0.5 13.2 1.6 10.6 12.1 2.8 14.6 5.4 1.0 10.2 15.1 2.9 5.0 1.0 0.1 3.2 2.0 0.4 31.7 2.0 5.0 9.9 12.9 2.0 5.0 1.0 0.6 3.4 1.9 0.1 17.8 16.0 1.6 7.1 4.5 6.8 2.1 0.1 2.9 0.7 Notes: (1) Children may have more than one diagnosis reported in the table, and not all conditions are reported, so percentages do not add to 100%. (2) Most Medi-Cal mental health services are not paid for by HPSM. For Healthy Families some mental health services are not paid for by HPSM. Utilization. Table 4-2 shows the annual use of ambulatory care by high cost and other users, for several types of ambulatory care, both preventive care and other care. Use rates are higher for the high cost users, across all three programs and for all types of ambulatory care services. In contrast to rates of use of other types of ambulatory care (including specialty care), the rates of visits and the number of visits for preventive care are somewhat similar between high cost users and other users. Still, a higher proportion of children who are high cost users have preventive care of some type, indicating perhaps that once children 24 have contact with the health care system for their chronic conditions they are then more likely to receive their preventive care visits. For example, 59.6 percent of Healthy Kids high cost users had preventive care in the year, in contrast to 49.2 percent of other users with at least some utilization of services. Table 4-2 Annual Use of Ambulatory Care High Cost and Other Users Children Continuously Enrolled in the Health Plan of San Mateo July 2004-June 2005 Healthy Kids Outpatient/Clinic Preventive Visits - % with visit - Average no. of visits Other Visits - % with visit - Average no. of visits Other Doctor Preventive visits - % with visit - Average no. of visits Other Visits - % with visit - Average no. of visits Any Preventive Visit - % with visit - Average no. of % visits Any Ambulatory Visit - % with visit - Average no. of visits Healthy Famlies Medi-Cal High Cost Other High Cost Other High Cost Other 48.2 0.7 41.3 0.5 37.4 0.5 30.6 0.4 26.2 0.5 18.2 0.3 91.4 6.8 65.1 1.8 86.0 4.9 50.5 1.1 87.9 7.1 58.6 1.6 13.6 0.2 10.9 0.1 33.6 0.5 27.9 0.3 25.4 0.5 26.6 0.4 38.2 3.6 16.8 0.4 48.6 4.8 39.4 1.0 66.0 3.5 49.7 1.6 59.6 0.9 49.2 0.6 64.5 1.0 55.0 0.7 45.6 1.0 40.6 0.7 99.6 11.3 95.0 3.4 100.0 10.7 94.7 2.8 96.2 11.6 90.5 4.6 In contrast, use of other (non-preventive) ambulatory care is much higher among the high cost users. The greatest difference between high cost and other users was in the percentage of high cost users with visits to outpatient/ clinics for services other than preventive care. (This category includes care in specialty clinics.) For example, 91.4 percent of Healthy Kids high cost users visited an outpatient/clinic for non-preventive 25 care; corresponding rates for Medi-Cal and Healthy Families were 87.9 percent and 86.0 percent respectively. (Rates were much lower, from 50.5 to 65.1 percent, for other users.) An even more striking difference in the use of this type of care was in the average number of visits to such providers, which was at least three times as high for the high cost users. A similar pattern pertains for visits to other (private) doctors for non-preventive care. The table shows a final measure, “any ambulatory care”, which includes all types of ambulatory care, whether it is in outpatient/clinic settings or in other doctors’ offices, and whether it is for preventive or non-preventive care. As shown, almost all users, either high cost or other, had some ambulatory care in the year, so the main way that the high cost groups differed is in their average number of ambulatory visits (11.3 visits for Healthy Kids, 10.7 for Healthy Families, and 11.6 for Medi-Cal), which is two to four times greater than for other users. Moving to the use of other health care services, table 4-3 shows that hospital use is a major determinant of high cost status. Only high cost children had any hospital care. Rates of hospital care use were 14.5 percent of Healthy Kids high cost users, 10.3 percent of Healthy Families high cost users, and a larger proportion (30.2 percent) of Medi-Cal high cost users. Another marker for being a high cost user was emergency room use. From 40 to about 60 percent of high cost users had an emergency room visit, depending on the program. Rates were much lower for other users. The rate of prescription drug use was also much greater for high cost users, particularly for the Medi-Cal high cost users, where 26 94.2 percent of users had a prescription (for an average of 18.6 prescriptions per child), 8 compared to 91.6 percent for Healthy Families and 80.5 percent for Healthy Kids. Table 4-3: Annual Use of Other Care High Cost and Other Users Children Continuously Enrolled in the Health Plan of San Mateo July 2004 - June 2005 Healthy Kids High Cost Other Healthy Families High Cost Other Medi-Cal High Cost Other Hospital - % with stay - Average no. of stays 14.5 0.2 0.0 0.0 10.3 0.1 0.0 0.0 30.2 0.4 0.4 0.0 E R Visits - % with visit - Average no. of visits 40.6 0.6 15.3 0.2 50.5 1.0 16.3 0.2 56.3 1.4 35.3 0.6 Prescriptions - % with prescription - Average no. of prescriptions 80.5 5.4 47.5 1.1 91.6 7.9 54.1 1.4 94.1 18.6 71.7 3.0 Vision Visits - % with visit - Average no. of visits 15.5 0.2 10.9 0.1 - - 10.5 0.1 7.0 0.1 Dental Visits - % with visit - Average no. of visits 63.2 1.7 66.7 1.9 - - - - Table 4-3 also compares use of vision and dental care between high cost and other users. (Vision care data are available only for Healthy Kids and Medi-Cal, and dental care for Healthy Kids). Interestingly, while a greater percentage of high cost users have had a vision visit tha n other users (15.5 and 10.9 percent respectively for Healthy Kids, for example), slightly fewer have had a dental visit compared to other users, as well as fewer visits on average. This is in contrast to the use of other forms of preventive care, which high cost children are more likely to have. 8 Prescription drug claims include other types of services such as durable medical equipment, supplies, and nutritional supplements or vitamins, when these are prescribed. 27 Table 4-4 compares the average cost for the high cost children and other children in all three programs, by type of service. Overall (and by definition), the high cost children are much more expensive than other children. Those children’s average annual costs range from $1,834 (Healthy Families) to $2.614 (Healthy Kids) to a much higher $6,530 (Medi-Cal). In contrast (after excluding dental and vision care costs, which leads to a more accurate comparison across programs), the average cost for non-high cost children (who are 90 percent of the users on the programs) is very low and does not differ greatly from program to program, ranging from $218 to $265. Table 4-4: Average Annual Cost of Care, High Cost and Other Users Children Continuously Enrolled in the Health Plan of San Mateo July 2004 - June 2005 Healthy Kids High Cost Other Healthy Families High Cost Other Outpatient/Clinic Other Physician E.R. Hospital Vision Dental Prescriptions Other Total $771 347 121 826 9 171 333 36 $2,614 $148 31 22 0 8 198 19 12 $438 $457 351 196 357 447 26 $1,834 Without Dental/Vision $2,434 $232 $1,834 $86 72 24 0 Medi-Cal High Cost Other 26 10 $218 $1,095 413 204 2,320 8 1,287 1,203 $6,530 $93 48 64 0 5 58 2 $270 $218 $6,522 $265 - The cost patterns by type of service correspond to the patterns in utilization noted above. For example, the costs for outpatient/clinic, other physician, emergency room, hospital, and prescription services were all much higher for high cost children, with the greatest disparities being for Medi-Cal children. A high cost of dental care, while the most expensive service on average for non–high cost users, was not a marker of a high cost user in the Healthy Kids program. 28 The total cost for children in the high cost group was a substantial portion of the cost of all children enrolled in each program: 39.9 percent for Healthy Kids, 48.4 percent for Healthy Families, and 72.8 percent for Medi-Cal (data not shown). Therefore the heavy concentration of costs in a small number of children is not as prevalent in the Healthy Kids and Healthy Families programs as for Medi-Cal and for the national population including adults (as cited earlier). Conclusions. In conclusion, the ten percent of children who have the highest annual cost in a year are different in many ways from the average child on the three public health insurance programs in San Mateo County. They are more often male and adolescents, as well as more often have chronic health conditions. They have high rates of contact with the medical care system, especially hospital and emergency room care, and very high average costs, especially for Medi-Cal. It is possible that the care for these children could be targeted for more intensive care co-ordination, both to the benefit of the child in terms continuity of care as well as the programs in terms of reduced costs. 29 Chapter 5: Do Healthy Kids Enrollees Obtain Needed Dental Health Services? What Barriers Restrict Access? Tooth decay is a significant problem among California elementary school children, and 28 percent of them have untreated tooth decay. Poor children and children of color, particularly Latino children, are much more likely to have tooth decay and suffer the consequences of untreated disease (Dental Health Foundation 2006). The San Mateo County Healthy Kids client survey described in the Second Annual Report revealed problems with access to dental care for some children. Only 72.3 percent of parents reported that their child had a usual source of dental care, compared to 88.1 percent who had a regular source of medical care. Parents were also asked if there had been a time when their child needed to see a dentist but did not; about 12 percent said yes (in contrast to only 6.3 percent for specialist medical care). When asked why, only three parents responded that the unmet need for dental care was due to the cost of care. This suggests that there are other barriers to access, such as provider availability, for some families. Focus groups with parents confirmed that dental care access was a perceived problem more often than medical care access. This chapter examines utilization and costs of dental care, describes the major sources of dental services for Healthy Kids children, and identifies potential barriers to services. The findings are based both on dental cla ims/encounter data and site visit interviews. The HPSM contracts with Delta Dental to provide dental services for children enrolled in Healthy Kids, and in turn, the HPSM obtains claims/encounter records from Delta Dental describing the use and cost of dental services for enrolled children. HPSM 30 produced tables on dental care for Healthy Kids enrollees for this report. (The plan does not maintain data on dental services for children enrolled in Medi-Cal or Healthy Families.) Service Use. During July 1, 2004 through June 30, 2005, 1,788 children (64 percent of Healthy Kids who were enrolled for the full 12 month period) had at least one dental service (Figure 5-1). Of the three age groups examined, adolescents (ages 13-18) were the least likely to have a dental service (56.9 percent), while children ages zero to five and six to 12 had higher rates (61.7 percent and 69.5 percent respectively). The high Figure 5-1: Percent with Any Dental Service, by Age Children Continuously Enrolled in Healthy Kids July 2003 to June 2004 80.0% 69.5% 70.0% 63.9% 61.7% Percent with Dental Service 60.0% 56.9% 50.0% 40.0% 30.0% 20.0% 10.0% 0.0% 0-5 6-12 13-18 All children Age use rate for the youngest age group may reflect statewide efforts to promote early dental examinations for very young children. The mean annual number of visits for those who used any care was essentially the same across age groups: 3.0 visits for children ages 1-5; 2.8 for children ages 6-12; and 3.0 for children ages 13-18 (data not shown). While these 31 data on dental service use show a frequent use of services for many children, especially the youngest children, it is important to note that 36 percent of continuously enrolled Healthy Kids enrollees had no dental service during the year. Table 5-1 shows that the majority of Healthy Kids who used dental services had either one (25.6 percent) or two (27.0 percent) dental visits in the year. Conversely, almost half had more visits, suggesting that they needed more than preventive dental care. Among these children, 37.9 percent had between three and five visits, and a smaller proportion (9.5 percent) had more than five. There was no difference in the frequency of visits by age (data not shown). Table 5-1: Average Number of Visits for Dental Service Children Continuously Enrolled in Healthy Kids July 2003 to June 2004 Number of Visits 1 2 3 to 5 More than 5 N Percent 25.6 27.0 37.9 9.5 1788 The most common dental services provided to Healthy Kids were for diagnostic and preventive care services, such as exams, x-rays, prophylaxis, sealants, and fluoride treatment (table 5-2). Fully 90.8 percent of dental users had a diagnostic exam and 84.8 percent had X-rays, with lower rates for prophylaxis (80.3 percent), sealants (63.7 percent), and fluoride treatment (56.9 percent). On the other hand, many children had more serious dental problems; for example, 17.7 percent of dental users had restorative treatment. 32 Service Cost. Children who had dental care were more expensive for the Healthy Kids program than those without dental services (table 5-3), and the cost of dental services represented a substantial proportion of the overall cost of their care. As shown in the table, the average total cost per child who had at least one dental service was $648 Table 5-3: Average Annual Cost per Enrollee for Dental and Other Services Children Continuously Enrolled in Healthy Kids July 2004 to June 2005 Dental Care Costs Other Care Costs Total Costs N Dental Other All Users Enrollees Enrollees $294 $0 $187 $354 $338 $348 $648 $338 $535 1788 1012 2800 33 compared to just $338 for those without any dental care. The average annual cost for other services was about the same for children with dental care ($354) and those without dental care ($338). Increasing the number of dental care users—a program goal—would increase the overall cost of care for Healthy Kids children, since there does not appear to be an offsetting reduction in medical care cost among these children. Of the three age groups, the average dental care cost was highest for adolescent dental users, suggesting more dental treatment for those children (data not shown). Types of Dental Care Providers. Table 5-4 shows the types of dental providers who are seeing Healthy Kids enrollees. As shown, the most common type of oral health providers are private dentists and just over a third are seen in the public system (either at the San Mateo Medical Center clinic or one of the three affiliated clinics: Fair Oaks, Willow, or Daly City). A very small percentage are seen at Sonrisas Dental Clinic—a private nonprofit clinic in the Half Moon Bay area, which does not have a public clinic— or by the Tooth Mobile. Table 5-4: Healthy Kids Dental Users by Type of Dental Provider Children Continuously Enrolled in Healthy Kids July 2004 - June 2005 Provider Percent of all Users San Mateo Medical Center and County Clinics 39.1 Private Dentists 43.3 Private Dental Groups 20.9 Sonrisas Dental Clinic 5.8 Tooth Mobile 0.5 N 1778 Note: Percentages do not sum to 100% since some children saw more than one type of provider. 34 The remainder of Healthy Kids, and the large majority, are seen by private individual dent ists or by private dental groups. There were 25 private individual dentists, and 15 dental groups, that billed for Healthy Kids services during the study period. Care in the private sector was concentrated heavily in a few private providers; two individual dentists saw more patients than all of the remaining individual dentists combined. There is evidence that a wider network of private dentists is potentially available to serve Healthy Kids. Recently, CHI staff called 21 private dentists and dental groups on the list of Delta Dental participating dentists and found that all of them currently accept Healthy Kids patients with relatively short waiting times for appointments (one to three weeks). This is in contrast to waiting times for county clinics, which are one to four months for dental care. Access to Dental Care. As shown above, over 30 percent of Healthy Kids (and an unknown percentage of other publicly insured children) have no dental care during a year. Consequently, it is important to consider ways that dental care access in San Mateo County could be expanded for publicly insured children. During the most recent site visit, in order to better understand potential barriers to access to dental services, we interviewed one public and one non-profit dental provider. In the previous evaluation year, as reported in the Second Annual Report, we conducted intensive interviews with five participating and five nonparticipating private dentists. The individuals that we interviewed were unaware of the extent of availability of private providers to serve Healthy Kids. Those interviewed felt that private dentists represent only a small proportion of dental providers for low income children in the county. They were aware that private dentists often serve low income children on a pro bono basis, 35 such as at the Samaritan House free clinic, Give Kids a Smile Day (where free dental screenings are provided), or in their own offices on a limited basis. This perceived preference to provide services for free, rather than to seek reimbursement from public programs, was viewed as a reflection of low reimbursement rates and cumbersome paperwork. For example, the dentists we interviewed said that it is sometimes difficult to obtain prior authorization for services such as root canals and X-rays. Although the data presented above, and the CHI survey of private dentists, suggest that access to private dental providers may be better than perceived by many stakeholders, gaining even broader private provider participation remains important to improving access. The CHI has already taken steps to improve access and utilization in two important ways: the establishment of a dental workgroup as part of the CHI Oversight Committee and plans for the Health Plan Retention Specialist to contact parents of children who do not utilize dental services to facilitate appropriate utilization. 9 We also heard the following suggestions for further improving provider participation: • Ensure that dentists are familiar with all three programs: Medi-Cal, Healthy Families and Healthy Kids; • Offer training on how to complete paperwork for public patients (especially Medi-Cal); • Align policies and procedures for reimbursement across the Medi-Cal, Healthy Families, and Healthy Kids programs. (For example, Medi-Cal claim codes are different from the claims codes used for Healthy Families and Healthy Kids.) Another likely barrier to care for many children is their parent’s lack of knowledge about when and where to obtain dental services for their children, particularly 9 Delta Dental does not actively promote utilization of services. 36 if they are accustomed to using only the county clinics for care. For example, they may be unaware that there are alternative sources in the private sector. On-going education to families about the value of regular oral health care and sources of services could alleviate this problem. Conclusions. While access to dental care appears to be better than perceived by many stakeholders, there are still a substantial number of Healthy Kids enrollees who do not have any dental care during a given year. Our findings suggest that an improved dialogue between the two sectors serving Healthy Kids (public and private) is likely to improve planning for services. It appears that capacity exits in the private sector for more Healthy Kids children and more children who have insurance could be diverted to the private sector to improve their access to dental care. In addition, the public sector could play an important role in monitoring indicators of quality of care in the private sector (such as the frequency and types of services) through the data available from HPSM and more regular contact between the two sectors. 37 Chapter 6: Do Healthy Kids Enrollees Obtain Needed Mental Health Services? What Barriers Restrict Access? Need for Children’s Mental Health Services. Natio nally mental health disorders affect as many as one in five children. However, only about a fifth of children who need mental health services receive them (Jellinek et al. 1999; DHHS 1999a), even though services have been shown to prevent juvenile delinque ncy and improve cognitive, academic, and social outcomes (Ramey and Ramey 1998; Zigler, Taussig, and Black 1992). Studies indicate that Latino children have especially high rates of unmet need for mental health services relative to other children (Kataoka, Zhang, and Wells 2002). The prevalence of children’s mental health problems in San Mateo County appears to be similar to national rates, at least for Healthy Kids program enrollees. The evaluation’s survey of the parents of Healthy Kids enrollees, conduc ted in 2004, included a series of questions about children’s emotional and behavioral health status. Parents were asked, for example, whether their child was often unhappy, sad, or depressed, and whether the child often did not get along with other children. Using these indicators, about 20 percent of parents reported that their child had an emotional or behavioral problem in the past 30 days. In addition, about 40 percent of those with school-age children with a mental health problem (or about 8 percent of all children) indicated that their child’s emotional and behavioral problem limited the child’s ability to do school work (Howell et al. 2005). This lower rate is closer to the estimated 6 percent of children nationally who have a serious emotional disturbance (SED) (DHHS 1999b). Children’s Mental Health Services in San Mateo County. San Mateo County has a history of innovative mental health services to address the needs of those with serious 38 mental health problems, including children. The county-organized system of care provides a coordinated network of health and social services to low- income children with severe emotional and behavioral problems. All three public programs have generous mental health benefits, as compared to many private insurance plans. There are no inpatient or outpatient benefit limitations for children with SED. Under Healthy Kids and Healthy Families, inpatient mental health services are limited to 30 days (no co-payment requirements). Outpatient mental health and outpatient substance abuse services are limited to 20 visits per benefit year. A copayment of $5 per visit is required for outpatient care. Inpatient substance abuse services only include hospitalization for detoxification. Children enrolled in Medi-Cal have no benefit limits and have access to a broad array of services through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. The San Mateo County Health Department/Mental Health Services Department (MHS) organizes and manages the delivery of mental health services for children with SED and some other children with mental health problems, for all three public programs. These services are provided through contracts between the MHS and private providers. We were told that the benefit limits specified by Healthy Kids and Health Families are not applied these county-organized mental health services. These services are available, without cost-sharing, to Healthy Kids and Healthy Families children who meet the criteria for MHS services. Services must fall within the plan of care developed by MHS clinicians. The MHS bills the appropriate entity, which differs by program. For example, MHS bills the state for Medi-Cal children, and it bills the HPSM for Healthy Kids 39 enrollees. Mental health services for Healthy Families enrollees who have SED are billed to the state, while services for other children are billed to the HPSM. For the decade ending in 2005, MHS was reimbursed a case rate per Medi-Cal child in the plan (the only California county under this arrangement). Currently, reimbursement for all three programs is through fee- for-service arrangements, but the care co-ordination functions of the MHS are still in place. There are mental health services provided by providers outside the MHS network that are billed directly to the HPSM for all three programs. For example, a pediatrician may treat a child for ADHD, or a child may be hospitalized for a condition such as anorexia on an emergency basis. In contrast, there are also low income children receiving mental health services who are not tracked by either system, that is by the MHS or the HPSM, for example children treated by county- funded therapists on the staff of the Family Resource Centers operated by the Human Services Agency. San Mateo County is in the process of planning an expansion of mental health services due to the passage of Proposition 63 of 2004, which created the Mental Health Services Act making available $750 million of new funding (with $5 million for San Mateo County) to improve mental health. San Mateo County was among the first to begin planning its use of these funds, although it is too early to know how the new services will affect children with mental health problems. 10 Use of Mental Health Services. In order to investigate whether the use of mental health services is low for children, as reported anecdotally during site visits, we requested tabulations from the HPSM for the two programs for which HPSM receives mental health 10 Details about the County’s plan can be found at: http://sanmateo.networkofcare.org/mh/home/prop63_sanmateo.cfm. 40 care claims, Healthy Kids and Healthy Families. (The plan does no t receive claims for Medi-Cal, and for children with SED under Healthy Families.) The tabulations cover all services reported to the plan for all children continuously enrolled in both programs from July 1, 2004, to June 30, 2005. For those children, the plan identified all children with a mental health diagnosis on at least one claim, and tabulated the following: (1) number of children by mental health diagnosis; (2) number of children with a mental health diagnosis according to the provider that served them; and (3) average annual mental health and non- mental health cost per enrollee. The health plan also supplied information about children who did not have any mental health claims for comparison purposes. It is important to note that because the claims of children with SED in Healthy Families are billed to and paid for by the state rather than HPSM, our analysis under-represents the cost for Healthy Families enrollees with mental health problems. As shown in table 6-1, despite reports in the client survey that about 20 percent of children had a mental health problem, only 5.7 percent of the 2,800 Healthy Kids enrollees who were continuously enrolled from July 2004 to June 2005 had any claims with a mental health diagnosis. The percentage of Healthy Families children with a claim with a mental health diagnosis was even lower, 4.2 percent. (Note that this excludes children with SED, possibly another 5 percent of enrollees.) For Healthy Kids, where the data base includes all mental health claims, the prevalence was highest among adolescents (ages 13–18), 7.4 percent of Healthy Kids enrollees, in contrast to a lower rate among younger children. 41 Table 6-1: Number (and Percent) of Enrollees with Any Mental Health Diagnosis, by Age Children Continuously Enrolled in The Health Plan of San Mateo July 2004 to June 2005 Mental Health Diagnosis Healthy Kids 0-5 years Age 6-12 years 13-18 years Total N Healthy Families 0-5 years Age 6-12 years 13-18 years Total N 5.1 4.7 7.4 5.7 159 4.8 3.9 4.3 4.2 57 Table 6-2 shows which mental health diagnoses were reported in the claims/encounter data. Patterns were similar between the two programs and to national patterns of children’s mental health disorders. Mood and anxiety disorders were the most prevalent diagnoses, affecting about a third or more of all mental health users in both programs. Attention-deficit and disruptive disorders affected 20 percent of Healthy Kids mental health users, and an even larger portion of Healthy Families users (reflecting a milder case mix given that SED children are excluded from the data). Developmental disorders, including autism as well as milder learning and communication disorders, affected about 20 percent of both Healthy Kids and Healthy Families children. Serious psychotic disorders, such as schizophrenia, were very rare, as were substance abuse 42 disorders. The remainder of children had a variety of other mental health conditions, such as eating disorders and sleeping disorders. Table 6-2: Mental Health Diagnoses Children Continuously Enrolled in the Health Plan of San Mateo July 2004 to June 2005 Healthy Kids Healthy (%) Families (%) Mood and Anxiety Disorders 33.3 40.4 Attention Deficit and Disruptive Behavior Disorders 23.3 33.3 Developmental Disorders 19.5 17.5 Substance Abuse Disorders * * Schizophrenia and Other Psychotic Disorders * * Other Disorders 24.5 12.3 Total Number of Children with a Mental Health Diagnosis 159 57 * Fewer than 5 children Figure 6-1 displays health service use for children with mental health diagnoses in Healthy Kids, as compared to the service use of all Healthy Kids program enrollees. Children with mental health diagnoses were more likely to have received ambulatory care, a preventive visit, or an emergency room visit when compared to all enrollees. The magnitude of the difference varied according to the type of service. For example, differences in the use of preventive care were small. Almost 48 percent of Healthy Kids mental health users had a preventive care visit during the year, while 39.6 percent of all program enrollees had a visit of that type during the same period. Differences in emergency room and prescription drug use, however, were larger. About three times as many Healthy Kids with mental health diagnoses had one or more ER visits, when compared to the total enrollee population. Also, 62.2 percent of Healthy Kids mental health users had one or more prescriptions in the time period, versus just 33.5 percent of all program enrollees. 43 Figure 6-1: Health Service Use for Children with a Mental Health Diagnosis Children Continuously Enrolled in Healthy Kids July 2004 to June 2005 98.1 100 90 80 73.8 70 62.2 60 47.8 50 39.6 40 36.5 33.5 30 20 12.5 10 0 Percentage with Ambulatory Visit Percentage with Preventive Care Visit All Healthy Kids Members Percentage with One or More ER Visits Percentage with One or More Prescriptions Healthy Kids Members with Mental Health Diagnosis Table 6-3 compares the cost to the HPSM for children with a mental health diagnosis to those without a mental health diagnosis for Healthy Kids and Healthy Families. Costs are separated into those for claims with a mental health diagnosis and other non- mental health costs. It shows that—for the services billed to the HPSM--the average mental health cost is similar between the two programs, $432 per child per year for Healthy Kids and $416 for Healthy Families. The average cost for non- mental health care for the same children is somewhat higher for Healthy Families ($571 versus $642 respectively). If the cost of care for the SED children were taken into account, the cost for mental health care would be considerably higher for Healthy Families children than for Healthy Kids. For example, data from the San Mateo County MHS show that they managed an average of 29 Healthy Families children with SED per month during July 44 2004 to June 2005, and that those children cost an average of over $10,000 per child per year, in contrast to only $432 billed to HPSM for Healthy Kids for the year. Table 6-3 : Average Costs Per Enrollee for Mental Health and Other Services Children Continuously Enrolled in the Health Plan of San Mateo July 2004 to June 2005 Mental Health Diagnosis Mental Health Claims Other Claims No Mental Health Diagnosis Mental Health Claims Other Claims Healthy Kids $432 $571 $0 $295 Healthy Families $416 $642 $0 $271 Note: Excludes dental and vision claims and claims from Healthy Families children with SED. One extremely high-cost case was excluded from Healthy Kids. The cost of non- mental health care is considerably higher for children with a mental health diagnosis than for other children. For example, for Healthy Kids, the average annual non- mental health cost was only $295 for those without a mental health diagnosis and $571 for those with a diagnosis. 11 As table 6-4 indicates, a substantial proportion of children were served by either the San Mateo Medical Center (43.4 percent of Healthy Kids and 29.8 percent of Healthy Families mental health users in the HPSM database) or by the San Mateo County Mental Health Department (27.7 percent and 31.6 percent respectively). For the services billed to the HPSM, children enrolled in Healthy Families were more than twice as likely to receive services through a private provider (28.1 percent) as Healthy Kids mental health users (10.7 percent). 45 Table 6-4 : Percent of Children served by Type of Mental Health Providers Children Continuously Enrolled in the Health Plan of San Mateo July 2004 to June 2005 San Mateo Medical Center San Mateo County Mental Health Dept. San Mateo County Outpatient Clinics Other Hospitals/Medical Centers Other Clinics Private Providers Other N Healthy Kids (%) 43.4 27.7 11.3 18.9 6.9 10.7 5.7 159 Healthy Families (%) 29.8 31.6 10.5 17.5 * 28.1 * 57 * Fewer than 5 children Note: Percentages do not add to 100 since a child may be served by more than one type of provider. Access to Care. In spite of the emphasis on expanded mental health services for children in San Mateo County, in the second and third annual site visits (October 2004 and 2005) we learned that there are still some barriers to obtaining mental health services for low income children. According to those we interviewed, one set of barriers relates to parents’ lack of information and reluctance to bring their children for services. Parents may not be aware of the mental health services available to their children, or they may be unsure about whether their child’s behavior is sufficiently different from that of other children to require help. Although the county health department has a web site 12 and a toll- free number, the population served by Healthy Kids may not access this. Parents may avoid treatment, even while realizing the need for professional help, because it could be regarded as a personal failure. Furthermore, undocumented parents may believe that 11 The tables exclude one extremely high-cost Healthy Kids user; including this single case would have almost doubled the “other” costs for Healthy Kids children with mental health diagnoses, illustrating the potential extreme effect of a single or a few very high cost users on average program costs. 46 participation in the county mental health system could lead to identification of their legal status. Such stigma and fear may be exacerbated by the limited number of Spanishspeaking mental health counselors and therapists in the county (although there have been some improvements recently). Recruitment problems are exacerbated by San Mateo’s high cost of living. We heard several suggestions from stakeholders about how to address some of these barriers. These included improved partnerships with schools in order to identify children needing services and to provide them with more school-based services; a relaxation of the requirement to demonstrate that a child has SED in order to qualify for expanded services; and an increased emphasis on screening and early identification of problems. Respondents were also very concerned that San Mateo County’s current model of integrated care delivery be maintained in spite of the budgetary difficulties the county has experienced recently. Conclusions. About 5 percent of children enrolled in the Health Plan of San Mateo had mental health services in a given year, according to information from the database maintained by the Health Plan of San Mateo. Healthy Kids and Healthy Families users in the health plan have similar patterns of mental health diagnoses, service use, and service costs, according to these data. In both programs, enrollees with mental health diagnoses had higher average costs—both for mental health care and other care-than other enrollees. Since the data analyzed here exclude services for Healthy Families children with SED, it appears that, at this time, the children with mental health problems in the Healthy Kids program have less serious mental health problems than for other public health insurance programs. In next year’s annual report we will obtain data on the 12 The address for this website is: www.sanmateo.networkofcare.org 47 cost of Healthy Families children’s care outside the HPSM, in order to examine this issue more thoroughly. Similar to national patterns, the prevalence of mental health problems (as reported by parents) is higher for Healthy Kids enrollees than the proportion of children using mental health services. Key stakeholders indicated that there are barriers to mental health care access for children served by Healthy Kids, Healthy Families, and Medi-Cal. It is possible that, if these barriers are appropriately addressed, more children with mental health problems will seek the care that they need. As with efforts to improve dental access, however, it is also evident that this improved access could increase the overall cost to public health insurance programs. 48 Chapter 7: What Is the Role of Schools in Outreach and Enrollment? The San Mateo CHI has numerous outreach and enrollment strategies, as described in the previous two annual reports. In particular, the CHI places an emphasis on school outreach and enrollment efforts as a way to identify uninsured children who may not be reachable in county clinics or other places. School-based enrollment also increases access to enrollment assistance by establishing more locations where assistance is offered. In 2004, about 17 percent of parents responding to the client survey said that they completed the application for Healthy Kids at a school (Howell et al. 2005). During the site visit in the fall of 2005, we interviewed six key people who are involved in CHI school outreach, including a CHI school outreach coordinator, two CHIfunded Community Health Advocates (CHAs) who work primarily in schools, two school district officials, and two school employees (a principal and a teacher). The purpose of these interviews was to describe the following: how school outreach is organized in San Mateo County; the outreach/enrollment activities that take place in schools; how those activities vary from school-to-school and district-to-district; and stakeholders’ perceptions of what works best in school outreach. School Outreach in San Mateo County. Through these interviews, as well as onsite observations in two schools, we learned that the number of schools that are involved in CHI school outreach in the county continues to grow, and that outreach/enrollment activities are quite variable from school- to-school and over time within schools. We were told that each of the school districts has a somewhat different approach to school outreach, and that each school district functions independently in determining which activities to sponsor. 49 In San Mateo County there are 25 separate school districts. There are 20 elementary school districts, 4 high school districts, and 1 community college. This makes it very complex and time-consuming to implement school outreach, since it is necessary for the CHI to negotiate arrangements differently in each district. In order to facilitate school outreach, the CHI has defined four regions of the county with a designated CHIfunded CHA 13 or a Community Based Organization CAA, or both assigned to each. The regions are North County, Middle County, South County, and Coast, with about seven school districts each except on the coast where there are only two districts. While the CHI has a relationship with every school district, it has a more intensive relationship with some districts. The CHI chose to initiate intensive efforts in these districts either due to the large number of uninsured children in the district, or to especially responsive school personnel, or to both. In these districts (Cabrillo, Jefferson Elementary, Pacifica, Pascadero, Ravenswood, Redwood City, San Bruno, San MateoFoster City, Sequoia Union High, and South San Francisco) the CHI either supports a designated district staff member who coordinates CHI activities or provides CHAs to conduct periodic enrollment assistance in one or more school sites. There are currently five CHI-staffed fixed school enrollment sites, which evolved from two (Cabrillo and San Mateo-Foster City) in the first year of the CHI. The CHAs enroll children from all around the school district, not just from the school where he or she is placed. In some school districts, the role of CHAs is expanded to include outreach for other types of services and health education. For example, the CHA responsible for the Cabrillo School District coordinates with a project sponsored by Stanford University that is designed to provide a range of family services in schools. She 13 The CHAs are bi-lingual certified application assistors who take a standard training program each year. 50 reminds families to use medical and dental care and renew their child’s insurance coverage. The intensity of these efforts to maintain contact with parents and provide broader health education varies from place-to-place around the county. In all school districts (except the community college) the CHI sponsors a lessintensive form of outreach called the Request for Information (“RFI”) process. In this process, an annual letter is provided to parents asking whether they need help applying for health insurance for their child. The Consumers Union helped to design and launch the RFI process in San Mateo County, as well as in some other counties around the state. The CHI has a model RFI process that districts and schools are free to modify. A model letter to parents is sent by the County Board of Education to each district superintendent to alter and use as they see fit. The superintendent then sends the letter to each principal, asking them to include it with an RFI flyer in all back-to-school materials directed to parents. The flyer should provide basic information on insurance and a questionnaire about whether the parent needs help applying for insurance for his/her child. The principal may in turn modify the letter and flyer, and then choose whether and when to send them to parents. When visiting schools, we observed that the wording of the letter and flyer, as well as the frequency, timing, and how they are sent to parents, varies greatly from school- to-school. According to CHI staff, this is by design so that school outreach can be tailored to the needs of each school. For example, we were told that some principals may post a notice on the school’s bulletin board, rather than sending the RFI letter and flyer to parents. Some choose to send them with information at the beginning of the school year, while others send them later in the year. 51 According to the model process, the returned RFIs should be collected by each school and forwarded to a central office at the Board of Education. These then go to a CHI staff member who is responsible for coordinating the CHI response to each letter and for summarizing information on returned RFIs. In following up on the returned RFIs, the CHI seeks to assure that every parent who requests enrollment assistance will be contacted by either the assigned CHA or a Community Based Organization CAA to provide information and application assistance. Usually, the CHA or Community Based Organization CAA contacts the parent by phone and makes an appointment for him/her to come to a fixed enrollment site with the appropriate paperwork to fill out the application. We obtained the number of RFIs returned by parents for school year 2005–2006. This information is maintained by the CHI staff member responsible for coordinating school outreach. There were 2,946 returned questionnaires for the school year, with 845 “no”s and the rest (2111) “yes”s (that is, the parent requests help in applying). Of those who said “yes,” by far the largest number (90 percent) are reported to be in three school districts: San Mateo-Foster City, Jefferson, and Pacifica. While there are no comparable data for previous years, we were told that the frequency of returned RFIs is increasing. However, it is difficult to document how many parents who requested information eventually enrolled their children. The CHI staff hopes that new data from One-e-App will help with this tracking. One factor that is reportedly very important in determining the success of the RFI process in identifying uninsured children is a strong commitment to the process at both the district and school levels. For example, one reason for more RFI returns in the San 52 Mateo-Foster City district is a special project called Teachers for Healthy Kids, a project that is co-sponsored by the California Teachers Association and the California Association of Health Plans, which promotes children’s health insurance in schools. The San Mateo/Foster City School District is one of the districts in the state that is participating in this project. This has led to considerable support from the superintendent, principals and teachers for CHI efforts. The project also sponsors a special coordinator who links the CHI to district schools and promotes the RFI process. The coordinator has engaged the two district school nurses in connecting parents of children who need health insurance to the CHI. Posters and flyers are available in this district’s schools to inform parents about how to obtain assistance applying for health insurance. These posters advertise the local CHI hot line number, and teachers, administrative staff and school nurses all have additional forms to give parents if they ever learn of a child without insurance. In addition to the RFI process, CHI school outreach staff periodically do other forms of school outreach in the “less intensive” districts. In 2005, for example, staff conducted presentations at health fairs in three districts, one district sponsored a “neighborhood walk”, and two other districts sponsored outreach in high school schoolbased clinics. The CHI is beginning to use MAA funding for school outreach/enrollment activities. (See chapter 2 for a description of this funding stream.) Schools can file claims for Medi-Cal outreach if they complete a web survey of time spent with all the individuals for whom they are claiming MAA reimbursement. This has become a substantial funding stream for some school districts. In one interview, we learned of a 53 school district that anticipates receiving $100,000 for a single year. These funds go into the school district’s general fund. Conclusions. Those we interviewed are enthusiastic about school outreach. As one CHA stated: “School outreach is successful because families don’t want to go to the county clinic to enroll in a program.” Still, it is evident that the yield of children to enroll is higher (per CAA) in clinics than in schools. Consequently it is important to be aware of cost tradeoffs in planning school outreach. In particular, it is important to target the highest- need schools (since the number of uninsured is now very small in most schools), as well as to improve the tracking systems to assure that all families who need insurance enrollment assistance are contacted. Using the One-e-App for this purpose may help in improving the understanding of the most productive school outreach (in terms of successful applications and renewals of coverage for all three public programs). Such a system could also be used to track whether children identified in schools are easier (or harder) to contact for renewing coverage, and whether they are more likely to use preventive care. These are two important potential benefits of intensive school outreach. 54 Chapter 8: What Factors Are Associated with Employer Decisions to Offer Private Insurance Coverage to Low Wage Workers in San Mateo County? Has the CHI Affected Employer Decisions? Employer-sponsored health insurance coverage forms a foundation for health insurance coverage, with over half of the American population receiving health benefits from their own or a family member’s employer (Kaiser Family Foundation 2006). Between 2000 and 2004, however, the rate of children covered by employer-sponsored insurance (ESI) fell nearly 5 percent nationwide (Holahan and Cook 2005). Across the nation, there were significant increases in private insurance premiums during that time period. Premiums for family coverage increased by a national average of 59 percent compared with inflation growth of just under 10 percent and wage growth of about 12 percent (Kaiser Family Foundation and Health Research and Educational Trust 2005). Correspondingly, the percent of private-sector employees with offers of health insurance who enrolled decreased in California (from 86.7 to 82.2 percent) during the period (SHADAC and the Urban Institute 2006). Because the San Mateo County Healthy Kids program has a relatively high income limit for program eligibility (up to 400 percent of the federal poverty level), a primary concern for the CHI has been to assure that families or employers are not substituting Healthy Kids coverage for other coverage that children could have (a phenomenon termed “crowd-out’). 14 In our second annual report, we presented data from the client survey on Healthy Kids coverage before enrolling in the program and access to employer-sponsored health insurance. The analysis showed that very few Healthy Kids enrollees have access to affordable health insurance, a finding that was confirmed by 55 information obtained in focus groups with parents of program enrollees (Howell et al. 2005). To further explore the issue of crowd-out within the Healthy Kids program, and to understand more fully how local employers view ESI coverage for dependent children, the evaluation team conducted a series of interviews with employers in conjunction with the October 2005 site visit. We interviewed eight individuals representing a range of employers, including a community bank, a restaurant, a plant nursery, an environmental consulting firm, an international-chain grocery store, a public transit authority, an independent living center for the elderly, and a lumber yard. Two of the interviews were conducted via telephone; all others were conducted in person, either one-on-one or in a small group setting. We identified and recruited these local employers through recommendations by the Chambers of Commerce in San Mateo, San Carlos, and Half Moon Bay. Context. A tight labor market in San Mateo County led historically to a high rate of employer sponsored health insurance. According to employers we interviewed, it was very difficult to fill vacancies in the service sector just five years ago because of competition from growing firms in the Silicon Valley. Another factor they identified was continued strong competition for workers from the public sector, which offers very generous health insurance and other benefits. Employers also reported several consecutive years of double-digit percentage rate increases in health insurance premiums for local businesses in San Mateo County, mirroring statewide reports of yearly premium increases ranging from 10 to 15.8 percent 14 In 2005, only 35 percent of lower-wage California firms offered health benefits to employees, compared with 72 percent of higher-wage firms (California HealthCare Foundation & CSHSC 2006). 56 during the 2001–2004 period (California HealthCare Foundation & CSHSC 2006). These health premium cost increases are compounded by other cost increases, such as the cost of liability insurance. Small groups are particularly vulnerable to these increases, since they have little bargaining power with their carriers. Decision to Offer Health Insurance. The employers we interviewed believed that it is necessary to offer health insurance in order to attract and retain good workers in San Mateo County. One employer said, “Most of our employees can’t even afford to live in this county, and this is one thing that we can do for them.” Employers also noted that, “Retention is generally good [since] employees don’t want to give up…benefits;” “Workers that aren’t interested in a job with benefits are probably not the type…you want as an employee or the type…you want to retain;” and “[Our] benefits have contributed to a stable workforce with little turnover.” All the employers we interviewed offered insurance to their full time permanent employees. Still, there was variation in the generosity of health insurance benefits they offered, even among our small sample. For example, the portion of the insurance premium covered by the employer varied. While most covered 85 percent or more of the premium for their employees, one employer reported that the amount paid was dependent on longevity (with 100 percent premium sponsorship only after 10,000 hours worked). Most required employees to pay a larger share of premiums for dependents, and two of the eight employers did not contribute to premiums for dependents. In six firms health insurance was only available to full- time employees. (The definition of “full-time” varied by employer from 30 to 40 hours per week.) 57 Those interviewed indicated that offering health insurance is more important for attracting and retaining certain types of employees than others. For example, young people, who are more likely to be temporary or part-time workers, are believed to be less concerned about an offer of health insurance. In addition, while all employers thought that offering health benefits was a factor in hiring and retention, other factors, such as promotions and wage levels, were thought to be just as or more important. The decision of whether to offer health benefits (and at what level) was also affected by the industry involved. Employers said they considered the offers of their competitors when making decisions about benefit levels. For example, we heard that most businesses in the restaurant industry do not offer insurance (with an exception for higher- level management positions), and those that do have higher operating costs and make less profit. Most nursery employers offer health insurance, but costs to employees are high and dependent coverage is not usually offered. On the other hand, businesses hiring professionals said that they must offer health benefits, as “people with a professional background aren’t likely to take a position without the benefits.” Recent Changes in Employer Health Insurance Coverage. The employers in our small sample said that the recent slackening of the labor market due to the “dot-com bust” had not yet caused them to change their decisions to offer health insurance, nor were they contemplating such a radical change. However, due to health insurance premium increases, nearly all employers reported that they have made, or are contemplating, smaller benefit changes to lower their costs. Two employers stopped offering a choice between a health maintenance organization and a preferred provider 58 organization, and two others were considering this. Other employers have increased employee cost-sharing. Take-up of Insurance. In this small sample, employee take- up of health insurance offers appeared to be directly related to the level of employer contribution to coverage. Those employers who contributed 85 percent or more to an employee’s premium reported that ‘most’ or ‘nearly all’ of their workforce accepted the offer. In contrast, the employers that did not cover the premium for dependents reported that almost no employees purchased insurance for their children. Awareness of and Use of Public Health Insurance by Employees. One major purpose of the interviews was to investigate whether employers might be considering dropping coverage of dependents, since Healthy Kids is now available for children in families up to 400 percent of the federal poverty level. However, none of the employers were aware that any of their employees used the Healthy Kids program. Indeed, only two of the eight employers interviewed had heard of the CHI before they received the recruitment call for participation in our evaluation activities, and only one individual had any significant knowledge of the initiative or its purpose. One employer was aware that their employees use Healthy Families as a source of dependent coverage. Interestingly, the same employer reported that when surveyed last year, most employees indicated a disinterest in the employer subsidizing their dependent coverage, and preferred instead to remain eligible for Healthy Families (reasoning that when they signed up for employer coverage, they would no longer qualify for Healthy Families). 59 Conclusions. Although our sample was small, the employers that we interviewed as part of the October 2005 site visit represented several different industries and each had adopted unique approaches to offering health insurance benefits to employees and their dependents. The account given here represents only views of employers that offer health benefits. Even so, it is clear that small employers face many challenges in deciding whether to sponsor health insurance, and at what level, for their workforce. Rapid health insurance premium increases are of primary concern to this group, and have resulted in cost containment measures such as the narrowing of options for health plan enrollment and increases in employee cost-sharing. Despite the challenges, the majority of employers that we interviewed agreed that offering health benefits to full time permanent employees was not only a reasonable responsibility of all businesses, but was also an important factor in maintaining a stable and well-qualified workforce. There is very little evidence that employers are even aware of the Healthy Kids program, and absolutely no evidence that the presence of the program has affected their decision to offer health insurance coverage. Still, because of continued financial pressure facing employers of low wage workers, it will be important to monitor employer decisions in the future as they respond to the higher health insurance costs they are facing. 60 Chapter 9: Conclusions The San Mateo County Children’s Health Initiative continues its successful efforts to provide coverage to children in the county who would otherwise be uninsured. In addition, during 2005 the initiative took on several new challenges such as an increased focus on improving retention in public programs, increasing the use of preventive care, and improving access to dental and mental health care. This annual report provides some new data on several of these and other issues that are important to the continued development of the initiative. Enrollment Growth. The growth in the Healthy Kids program continued at a slow pace in 2005. Since funding for premiums for the youngest children (ages 0–5) is secure, the CHI strove to increase enrollment in that age group, but growth was limited. While data on the number of uninsured children in that age group are unavailable, it appears that the demand is diminishing and many of those children may now be enrolled in some form of insurance. Growth in the 6–18 age group continues at a moderate pace, creating a challenge to the premium financing for these enrollees. We did not study the growth in Healthy Families and Medi-Cal children for this annual report, a topic that will be revisited next year. The Healthy Kids population continues to have more older children than the other public programs, and the demographic composition of program enrollees (for example, age and ethnicity) did no t change very much from year to year. One change has been a moderate increase in the proportion of children who are in the higher income group (250–400 percent of the federal poverty level). It should be noted that increased penetration of coverage within this population was a specific priority for the CHI during 61 the last year. Given the early success, it is possible that there is potential for further growth among this population. Trends in Service Use. The report shows that there have been some positive trends in preventive service use for the Healthy Kids program. The use of preventive medical care, as well as dental and vision care, increased from the first to the second year of enrollment in Healthy Kids for all three services. In addition, overall us e of ambulatory care increased from those enrolled in 2003 to those enrolled in 2004. High Cost Users of Services. High cost users are a special group of children worthy of further attention by the CHI. These children are heavy users of expensive medical (although not dental) care, particularly hospitals and emergency rooms. They are more often chronically ill and have frequent contact with the health care system. Since it is possible to identify them through the claims/encounter data, this group could be targeted for more intensive contact by CAAs and/or health plan staff, to assure that they are receiving coordinated care and that they have good access to the specialty care that they need. Reducing their costs—even if only moderately through, for example, reduced hospital and emergency room use—could have an impact on the overall cost of care, and provide additional funding to cover other children. Dental Care Access and Costs. The information we obtained from interviews with stakeholders suggested that dental care access was poor for some children, especially access to private providers who do not like the paper work associated with public programs. However, this finding was not confirmed by the data analysis nor the recent survey of private dentists by health department staff. This more recent information indicates that there are private dentists who are already serving Healthy Kids and others 62 who are willing to do so. This is also possibly true for children in other public programs, although we did not have quantitative information from those programs to study the issue. Consequently one problem appears to be a lack of communication between the public and private sectors, as well as a knowledge gap among parents who may be unaware that they can use priva te dental providers. This suggests the need for more education and outreach at several levels in order to improve access and reduce waiting times for appointments. Mental Health Access and Cost. As indicated in last year’s report, Healthy Kids enrollees have emotional or behavioral problems at a rate that is comparable to national rates, and yet many children with mental health problems do not seek or get care. In addition, the most common mental health diagnoses for Healthy Kids members are consistent with the most common diagnoses for children nationally. In comparing the two public programs for which there are data from the HPSM, we found that children with mental health diagnoses are much more expensive than their peers, and these higher costs pertain to both mental health and other health services. Given that some very expensive Healthy Families children are excluded from the data base, Healthy Kids children with mental health problems are less expensive than those in the Healthy Families program. It is also clear that not all children receiving mental health services under both Healthy Kids and Healthy Families are having their care coordinated by the San Mateo Health Department Mental Health Services, but that those who are in that system are the more expensive children. The CHI should consider whether it wants to undertake an effort to link more children to the MHS when they are receiving mental health services outside that system, or whether—alternatively—having children receive services outside 63 the formal mental health system may help to overcome the stigma of receiving mental health services. There may be a need to educate primary care providers about the mental health needs of publicly insured children and about the additional services available to them through the MHS. For example, mental health screening could become a part of the required initial visit through the HPSM. Since not all children with mental health problems are receiving services, the CHI should consider how to increase use of services. One idea might be to use the linkages with schools that have been established for outreach and enrollment to advertise the availability of mental health services through the MHS. School Outreach and Enrollment. The CHI continues to experiment with innovative ways to reach and enroll uninsured children in schools around the county. Because there is so much variation in what is going on in different school districts, and schools within districts, the CHI could capitalize on this “natural experiment” to learn more about what is working well in terms of completed applications. To do this, it is important to obtain more detailed information in all school districts on, for example, the number of RFIs that are distributed and returned (with requests for help) and the number of completed applications by school where the RFIs have been distributed. The One-e-Ap system should help in learning about these patterns. After obtaining this detailed information, the CHI may want to revisit its “model” school outreach/enrollment process and refine the process accordingly. It is possible, for example, that the RFI process is not yielding any applications in some places, in spite of concerted efforts, or that it could yield more in others, if efforts were more concentrated and intense. 64 Employer Sponsored Health Insurance and Crowd-Out. Employers of low wage workers in San Mateo County face many of the financial strains of other similar employers around the country, but they are in a labor market where it is difficult to attract and retain workers (because of the high cost of living and other factors). Consequently, the employers with whom we spoke—while a small select group—felt that they need to offer health insurance benefits to their employees. However, two of the eight did not cover the dependents of their employees, and most of the businesses did not cover parttime or temporary workers. This means that the children of those working in such places may be uninsured. In no case was there any evidence that employers had changed their decisions to cover dependents because public coverage was available for low income uninsured children. Indeed, most were unaware of the CHI, and had not been exposed to the outreach activities of the initiative. The CHI may want to cautiously reach out to employees of selected businesses that do not offer dependent coverage, or that have many part-time or temporary workers, in order to provide information to parents who cannot afford to purchase coverage for their children. Given that the financ ing for children ages 6-18 is still uncertain, it might be possible to target such outreach to parents of very young children where premium financing is more secure. Next Steps in the Evaluation. In the coming year, the evaluation of the San Mateo CHI will collect new data to address a range of evaluation questions. Results from that analysis will be contained in next year’s annual report. The second wave of the client survey is currently underway, with an over-sample of children ages zero to five. Data from this survey will be used to measure the impact of the Healthy Kids program on 65 access to care, use of services, and health status. The survey will also provide information on prior insurance coverage and parent satisfaction with the program. In addition, another site visit and two client focus groups will provide qualitative information to help monitor the progress of the CHI and interpret the findings from the client survey analysis. Administrative data on enrollment trends will also be presented. Finally, the data from the HPSM, such as that included in this annual report, will be used to continue to monitor trends in enrollee characteristics and use of services across the three public health insurance programs for children in San Mateo County. 66 References Buck, Jeffrey A., Judith L. Teich, and Kay Miller. 2003. “Use of Mental Health and Substance Abuse Services Among High Cost Medicaid Enrollees.” Administration and. Policy in Mental Health and Mental Health Services Research 1(1): 3–14. California Bud get Project. 2006. Governor Releases 2006-07 May Revision. http://www.cbp.org/2006/060512_mayrevision.pdf. California HealthCare Foundation and Center for Studying Health System Change (CSHSC). 2006. California Employer Health Benefits Survey 2005. www.chcf.org/documents/insurance/EmployerBenefitSurvey05.pdf. Dental Health Foundation. 2006. “Mommy, It Hurts to Chew: The California Smile Survey. An Oral Health Assessment of California’s Kindergarten and 3rd Grade Children.” Oakland, CA: Dental Health Foundation. Department of Health and Human Services (DHHS). 1999a. Mental Health, United States, 2000. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Mental Health Services. ———. 1999b. Mental Health: A Report of the Surgeon General. Rockville, MD: Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health. http://www.surgeongeneral.gov/library/mentalhealth/home.html. Garfinkel, Steven A., Gerald F. Riley, and Vincent G. Iannacchione. 1998. “High Cost Users of Medical Care.” Health Care Financing Review. 9(4): 41–52. Holahan, John, and Allison Cook. 2005. “Changes in Economic Conditions and Health Insurance Coverage, 2000–2004.” Health Affairs web exclusive. Howell, Embry, Dana Hughes, Genevieve Kenney, Jennifer Sullivan, and Jamie Rubenstein. 2005. Evaluation of the San Mateo County Children’s Health Initiative: Second Annual Report. Developed for the San Mateo Children’s Health Initiative Coalition. Jellinek, Michael S., J. Michael Murphy, Michelle Little, Maria E. Pagano, Diane M. Comer, and Kelly J. Kelleher. 1999. “Use of the Pediatric Symptom Checklist to Screen for Psychosocial Problems in Pediatric Primary Care: A National Feasibility Study.” Archives of Pediatrics and Adolescent Medicine 153:254–60. Kaiser Family Foundation. 2006. Health Insurance Coverage of the Total Population, U.S. 2004. Urban Institute and Kaiser Commission on Medicaid and the Uninsured estimates based on the Census Bureau’s March 2004 and 2005 Current Population 67 Survey. http://www.statehealthfacts.kff.org/cgibin/healthfacts.cgi?action=compare&category=Health+Coverage+%26+Uninsured&subc ategory. Kataoka, Sheryl H., Lily Zhang, and Kenneth B. Wells. 2002. “Unmet Need for Mental Health Care Among US Children.” American Journal of Psychiatry 159(9): 1548–55. Kozyrskyj, Anita, Lisa Lix, Matthew Dahl, and Ruth-Ann Soodeen. 2005. High Cost Users of Pharmaceuticals: Who are They? Manitoba Center for Health Policy. National Center for Health Statistics. 2003. Health, United States, 2003 [with Chartbook on Trends in the Health of Americans]. Hyattsville, MD: National Center for Health Statistics. Ramey, Craig T. and Sharon L. Ramey. 1998. “Early Intervention and Early Experience.” American Psychologist 53:109–20. San Mateo County Controller. 2006. Financial Highlights. Selected Editions. http://www.co.sanmateo.ca.us/smc/department/controller/home/0,2151,4666323_407558 44,00.html. State Health Access Data Assistance Center (SHADAC) and the Urban Institute. 2006. Shifting Ground: Changes in Employer-Sponsored Health Insurance. Prepared for the Robert Wood Johnson Foundation. Zigler, Edward, Cara Taussig, and Kathryn Black. 1992. “Early Childhood Intervention. A Promising Preventative for Juvenile Delinquency.” American Psychologist 47:997– 1006. 68 APPENDIX – A Appendix A Research Questions of the Evaluation of the San Mateo Children's Health Initiative 1 Who was served by the San Mateo CHI? How did the composition of enrollees change over time? 2 Did the CHI have an impact on access to care for children who enrolled? 3 What services did Healthy Kids enrollees receive as part of the initiative? Did the CHI have animpact on where those services were received or the cost of their care? Year 1 Year 2 Year 3 Year 4 Final Report P P P P P P P P P P P 5 Did the CHI increase community-wide collaboration to address issues of the uninsured? Did public coverage replace private coverage? If so, what were the factors associated with employer and beneficiary decisions to drop private coverage? 6 Did the level of health insurance coverage change for children in San Mateo County? 7 Did the CHI have an impact on the health status of children who enrolled? 8 Did the CHI have an impact on school performance or quality of life? 9 Were parents satisfied with the new program and services? Were providers satisfied? P 10 Did the CHI enhance the delivery and stability of the community health care system? P 4 P P P P P P P P P P P P P P