INTERFACE MICROMOTION FAILURE SIMULATION OF CEMENTLESS HIP PROSTHESIS (SIMULASI KEGAGALAN PERGERAKAN MIKRO
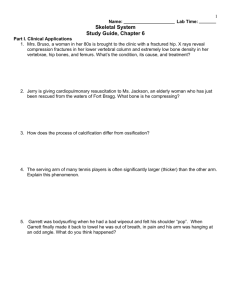
advertisement

INTERFACE MICROMOTION FAILURE SIMULATION OF CEMENTLESS HIP PROSTHESIS (SIMULASI KEGAGALAN PERGERAKAN MIKRO ANTARAMUKA IMPLAN TULANG PINGGUL MENGGUNAKAN KAEDAH TANPA SIMEN) MOHAMMED RAFIQ BIN DATO’ ABDUL KADIR RESEARCH VOTE NO: 78057 PUSAT PENGURUSAN PENYELIDIKAN UNIVERSITI TENOLOGI MALAYSIA 2007 INTERFACE MICROMOTION FAILURE SIMULATION OF CEMENTLESS HIP PROSTHESIS (SIMULASI KEGAGALAN PERGERAKAN MIKRO ANTARAMUKA IMPLAN TULANG PINGGUL MENGGUNAKAN KAEDAH TANPA SIMEN) MOHAMMED RAFIQ BIN DATO’ ABDUL KADIR RESEARCH VOTE NO: 78057 Jabatan Kejuruteraan Bahan Fakulti Kejuruteraan Mekanikal Universiti Teknologi Malaysia 2007 Acknowledgements I would like to acknowledge the Ministry of Higher Education for providing the research grant of RM15,000. Thank you also to all staff at the Research Management Centre, UTM, for providing all the support so that the research can be completed successfully. Lampiran 20 UTM/RMC/F/0024 (1998) UNIVERSITI TEKNOLOGI MALAYSIA BORANG PENGESAHAN LAPORAN AKHIR PENYELIDIKAN TAJUK PROJEK : Saya Interface Micromotion Failure Simulation of Cementless Hip Prosthesis MOHAMMED RAFIQ BIN DATO’ ABDUL KADIR (HURUF BESAR) Mengaku membenarkan Laporan Akhir Penyelidikan ini disimpan di Perpustakaan Teknologi Malaysia dengan syarat-syarat kegunaan seperti berikut : Universiti 1. Laporan Akhir Penyelidikan ini adalah hakmilik Universiti Teknologi Malaysia. 2. Perpustakaan Universiti Teknologi Malaysia dibenarkan membuat salinan untuk tujuan rujukan sahaja. 3. Perpustakaan dibenarkan membuat penjualan Penyelidikan ini bagi kategori TIDAK TERHAD. 4. * Sila tandakan ( / ) salinan Laporan Akhir SULIT (Mengandungi maklumat yang berdarjah keselamatan atau Kepentingan Malaysia seperti yang termaktub di dalam AKTA RAHSIA RASMI 1972). TERHAD (Mengandungi maklumat TERHAD yang telah ditentukan oleh Organisasi/badan di mana penyelidikan dijalankan). TIDAK TERHAD TANDATANGAN KETUA PENYELIDIK Mohammed Rafiq bin Dato’ Abdul Kadir Ketua Projek 78057 Tarikh : 31 Disember 2007 CATATAN : * Jika Laporan Akhir Penyelidikan ini SULIT atau TERHAD, sila lampirkan surat daripada pihak berkuasa/organisasi berkenaan dengan menyatakan sekali sebab dan tempoh laporan ini perlu dikelaskan sebagai SULIT dan TERHAD. Lampiran 13 UTM/RMC/F/0014 (1998) UNIVERSITI TEKNOLOGI MALAYSIA Research Management Centre PRELIMINARY IP SCREENING & TECHNOLOGY ASSESSMENT FORM (To be completed by Project Leader submission of Final Report to RMC or whenever IP protection arrangement is required) 1. PROJECT TITLE IDENTIFICATION : INTERFACE MICROMOTION FAILURE SIMULATION OF CEMENTLESS HIP PROSTHESISng Learning Styles: Their Impact On University Student's Learning Orientations Study Skills and Academic Achievements 2. Vote No: 780571 PROJECT LEADER : Name : MOHAMMED RAFIQ BIN ABDUL KADIR Address : DEPARTMENT OF MATERIALS ENGINEERING, FACULTY OF MECHANICAL ENGINEERING, UNIVERSITI TEKNOLOGI MALAYSIA. Tel 3. : 07-5534806 Fax : 07-5566159 e-mail : rafiq@fkm.utm.my DIRECT OUTPUT OF PROJECT (Please tick where applicable) Scientific Research Applied Research Algorithm Structure Product/Process Development Method/Technique Product / Component Demonstration / Process Prototype Data Other, please specify 4. Software Other, please specify Other, please specify ___________________ __________________ ___________________________ ___________________ __________________ ___________________________ ___________________ __________________ ___________________________ INTELLECTUAL PROPERTY (Please tick where applicable) Not patentable Technology protected by patents Patent search required Patent pending Patent search completed and clean Monograph available Invention remains confidential Inventor technology champion No publications pending Inventor team player No prior claims to the technology 1 Industrial partner identified UTM/RMC/F/0014 (1998) 5. LIST OF EQUIPMENT BOUGHT USING THIS VOT COMPUTER PRINTER EXTERNAL BACKUP HARD DRIVE 6. 7. STATEMENT OF ACCOUNT a) APPROVED FUNDING RM : 15,000.00 b) TOTAL SPENDING RM : 14,999.55 c) BALANCE RM : 0.45 TECHNICAL DESCRIPTION AND PERSPECTIVE Please tick an executive summary of the new technology product, process, etc., describing how it works. Include brief analysis that compares it with competitive technology and signals the one that it may replace. Identify potential technology user group and the strategic means for exploitation. a) Technology Description The project involves the establishment of techniques to simulate failure after femoral replacement. The following steps have been recognized as one of the methods for simulation: Reconstruction of human joint either from CT dataset or from three dimension bone banks, design of a suitable hip prosthesis to fit the bone model, virtual reaming of the bone to represent bone bed preparation, and finally analyzing failure using finite element. b) Market Potential This technique can be widely used in the design and development of new hip prosthesis. With the increase of imported orthopaedic products nationwide, the technique can be used by local implant manufacturer to develop a locally made femoral prosthesis. 2 UTM/RMC/F/0014 (1998) c) Commercialisation Strategies This project has already established a method to analyse failure of hip replacement. This method can be used by implant manufacturers for their newly developed hip stem. However, the technique should already be well established for international implant manufacturers. The best way to proceed is to do consultation services to local manufacturers, and at the same time develop the tools into a standalone software for commercialization. 8. Signature of Projet Leader :- Date :- ______________________ __________________ RESEARCH PERFORMANCE EVALUATION a) FACULTY RESEARCH COORDINATOR Research Status Spending Overall Status ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) Excellent Very Good Good Satisfactory ( ) ( ) ( ) Fair Weak Comment/Recommendations : _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ ………………………………………… Signature and stamp of JKPP Chairman Name : ……………………………………… Date 3 : ……………………………………… UTM/RMC/F/0014 (1998) RE b) RMC EVALUATION Research Status Spending Overall Status ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) Excellent Very Good Good ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) ( ) Satisfactory Fair Weak Comments :_____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ Recommendations : Needs further research Patent application recommended Market without patent No tangible product. Report to be filed as reference ……………………………………….. Name : …………………………………………… Signature and Stamp of Dean / Deputy Dean Research Management Centre Date : …………………………………………… 4 ABSTRACT The most commonly reported failure modes of cementless hip stems are loosening and thigh pain; both are attributed to the relative motion at the bone-implant interface due to failure to achieve sufficient primary fixation. Accurate predictions of hip stems’ stability are therefore crucial to the pre-clinical analyses of hip arthroplasty. This study uses finite element technique to analyse the effect of muscle forces on the predicted micromotion and therefore stability of cementless femoral components. An in-house experimentally validated micromotion algorithm was used in analyses simulating two of the most common physiological activities – walking and stair-climbing. The results showed that models where muscle loads were included had ten times larger micromotion than those modelled without muscle loads. Ignoring muscle forces in any pre-clinical evaluation of femoral stems are therefore not advisable as it will overestimate the stability of the stem. Keywords: Hip arthroplasty, Cementless stem, Finite element, Muscle loadings, Primary stability, Interface micromotion. ABSTRAK Mod kegagalan yang selalu dilaporkan apabila pembedahan tulang tanpa menggunakan simen adalah kelonggaran dan sakit peha; kedua-duanya disebabkan gerakan antara implan relatif kepada tulang disebabkan kegagalan untuk mencapai ikatan pertama yang kuat. Ramalan yang tepat terhadap kestabilan implan tulang peha adalah amat penting dalam menganalisa sebelum pembedahan dibuat. Kajian ini menggunakan kaedah unsure terhingga untuk menganalisa kesan beban otot terhadap ramalan gerakan mikro dan sekaligus menentukan kestabilan implan tanpa menggunakan kaedah simen. Satu algoritma gerakan mikro yang telah divalidasi secara eksperimen telah digunakan di dalam analisa dua gerakan fisiologi – berjalan dan menaiki tangga. Keputusan menunjukkan simulasi dimana beban otot dimasukkan mempunyai 10 kali ganda gerakan mikro daripada simulasi dimana beban otot tidak dimasukkan. Semua analisis untuk mengenalpasti gerakan mikro dengan itu mestilah memasukkan beban otot untuk memberikan ramalan yang tepat. Kata Kunci: Pembedahan tulang peha, Implant tulang peha tanpa simen, Kaedah unsure terhingga, Beban otot, Kestabilan pertama, Gerakan mikro antaramuka.. Chapter 1 Introduction and Literature Review The number of people undergoing hip joint replacement surgery has increased over the past decades. In the UK alone, more than 60,000 total hip arthroplasties (THA) are performed annually, 15% of which are performed in the younger age group (less than 57 years old) (Tennent & Goddard 2000). Most hip replacements are performed on patients suffering from osteoarthritis, a joint disease associated with the wearing away of the cartilage covering the bone ends. Other degenerative hip disorders that could require THA include rheumatoid arthritis and avascular necrosis. The primary aim of the replacement surgery is to relieve pain and regain mobility. Pioneered in 1962 by the renowned English surgeon, Sir John Charnley, the development of orthopaedic implants used in hip arthroplasty has improved steadily, making it one of the most successful surgical procedures. However, with the increase in the number of hip replacements performed, the scope and frequency of complications appear to be increasing. Complications such as stress-shielding, osteolysis and aseptic loosening remain some of the major problems in hip arthroplasty (Macdonald 1998). There are mainly two types of hip arthroplasty in use today – cemented and cementless. Hip prostheses with the use of cement are the most commonly used but 1 the cementless techniques are gaining popularity. Fixation of these femoral components is a major concern because bone growth could only be achieved on stable implants (Pilliar 1991; Simmons, Valiquette & Pilliar 1999). Failure to achieve a strong fixation will result in the formation of fibrous tissue layer at the bone-implant interface and the eventual loosening of the implant (Pilliar, Lee & Maniatopoulos 1986). PMMA is used in the cemented type prostheses to provide strong primary fixation. However, cement debris can cause complications such as inflammation and bone lysis. One of the solutions to this problem is to abolish the use of cement, thus the cementless femoral component. However, without the cement these implants could not achieve initial fixation, unless the design is modified so that proper and adequate stability could be achieved. The design of femoral prostheses, together with the surgical techniques of implantation, continues to receive much attention in the hip biomechanics community. Degenerative hip disorders are the major reason for hip joint arthroplasty. The disease can become so severe that replacement surgery is the only way to remove pain and regain mobility. In this section several major hip disorders are discussed, as well as a brief introduction to a common skeletal disorder of osteoporosis. Osteoarthritis is a degenerative condition associated with the wearing away of the cartilage covering the bone-ends. Cartilage is used to absorb the stresses put on a joint, and protects the bones from damage. Osteoarthritis occurs when the cartilage deteriorates, either due to age or injury. With age, human joints slowly lose the ability to regenerate and repair the cartilage. Bone growths develop as the cartilage degenerates, and the bones that make up the joint rub together, causing pain and restriction of movement. It is a progressive disease that can affect any or all of the joints in the human body, with the weight-bearing joints such as the hips and the knees being more susceptible than the others. Currently, no cure exists for osteoarthritis. Treatment options centre on prevention, if possible, and control of the disease. At its worst, the disease can cause constant pain and severely reduced mobility. Rheumatoid arthritis is another form of arthritis that is chronic and affects many different joints. It begins with an inflammation and thickening of the synovial 2 membrane, which causes pain and swelling, followed by bone and cartilage degeneration and disfigurement. The disease is considered to be an autoimmune condition that is acquired, and in which genetic factors appear to play a role. It appears more frequently in older people, with more women being affected than men. Avascular Necrosis (AVN) is a skeletal disease that occurs when bone tissues die off, resulting in the collapse of the bone. It is caused by the loss of blood to the bone. Hips are one of the areas most commonly affected by the disease. Common names for this disease include osteonecrosis, aseptic necrosis and ischemic bone necrosis. The disease can be caused by excessive use of drugs and alcohol or by injury. A joint that has been injured through fracture or dislocation has an increase risk of AVN because blood vessels may be damaged, and blood circulation to the bone is disrupted resulting in trauma-related AVN. Arthritis and AVN affect both men and women at higher rates as they age. The majority of cases involve people between the ages of 30 and 50 years. However, it can affect people of all ages. Osteoporosis is a major skeletal disorder in which nutrition plays a role and can be prevented and treated. It is characterised by a significant loss of cancellous bone stock and structural deterioration of bone tissue, causing it to become fragile and more likely to fracture. If left untreated, the disease can progress without symptoms until the bones became so weak that a sudden strain, bump, or fall causes a fracture. Fractures occur typically in the hip, spine and wrist. Women are more likely to suffer from osteoporosis than men. Osteoporosis is not a cause for joint replacement, but if a replacement is required due to fracture for example, then it affects the decision made by the surgeon because of the structural deterioration of the bone. There are two major types of artificial hip replacements: cemented and uncemented. Both are widely used. The superiority of one compared to the other remains a topic of debate. The choice made by orthopaedic surgeons is usually based on the patient’s age, type of disease, anatomy, lifestyle, and the surgeon's experience. The surgeon's criteria of a suitable hip implant include: Shape and design for optimum fit within the patient's anatomy. Shape and design which allow for optimum surgical technique. 3 The implant’s clinical history of stability – called fixation. The exterior coating of the stem, which contributes to optimum fixation. The type of surgery – primary, revision or fracture. Cemented prostheses are the oldest form of hip arthroplasty. They are held in place by a type of epoxy cement that attaches the stem to the bone. Good clinical results at 10 years are achievable through this method (Emery et al. 1997). There are, however, complications arising from this conventional method of fixing artificial joints, mainly from the use of the cement itself. PMMA degrades over time and the built-up of cement debris causes inflammation of the surrounding bone and loosening at the interface (El-Warrak et al. 2001). Revision surgery, if required, will also be a problem due to the significant removal of bulk cancellous bone during the first surgery. Despite these complications cemented techniques are still widely used depending on the condition of the patients. It has been suggested for use in the older patients above 65 years (Dorr, Wan & Gruen 1997), or on patients with osteoporotic bone condition or poor bone stock to ensure strong primary fixation (Haber & Goodman 1998). However, Harris (1997) strongly believed that cemented techniques not only worked well with the elderly, but also for younger patients. Early total hip arthroplasty using the cementing technique in the late 1960s and early 1970s showed an incidence of femoral component loosening of 30%-40% at 10 years (Stauffer 1982; Sutherland et al. 1982). These disappointing results led to revised cementing techniques (Rasquinha et al. 2003), and the use of bioactive cement to encourage rapid bone ingrowth (Oonishi 1991). Some authors also suggested limiting the cement to the proximal area only (sometimes called the hybrid option) (Monti, Cristofolini & Viceconti 2001). The cementless alternative is used to eliminate the problems associated with the use of cement. The diameter of the stem is generally larger than its cemented counterpart in order to fill the canal, and the surface is usually roughened with particles through grit-blasting or plasma-spraying. Roughened surfaces are not recommended in cemented stems; they are usually polished in order to reduce cement wear debris (Duffy et al. 2001). Some cementless designs also have macro-features at the proximal part such as a porous coating or fibre meshing. These features are beneficial 4 in cementless implants because they provide a medium for biological attachment that secures the implant onto its place. The roughened surface encourages bone attachment and the macro-features allow new bone to attach and grow into, creating a strong bond between the patient’s own natural tissue and the implant (Whiteside et al. 1993). Besides the promising results of cementless stems, old complications associated with the cemented technique are still not entirely eliminated. Stress-shielding, for example, still occurs in hip replaced with cementless stems (Nourbash & Paprosky 1998). Osteolysis also occurs in cementless arthroplasty due to wear debris. It was previously thought that migration of cement debris along the bone-cement interface was the cause of osteolysis, due to the detection of particles of PMMA of various sizes found in failed interface membranes. However, a study by Boss et al. (1990) showed that the release and deposition of wear products, of whatever nature, were apparently responsible for osteolysis. Aseptic loosening is a major concern in cementless hip stems, and it is a failure associated with the lack of stability. It can be divided into 2 categories (Horikoshi et al. 1994). The 1st category is a late failure due to osteolysis which can be explained by excessive wear particles that migrate along the implant-bone interface and result in formation of the activated interfacial membranes. Early failure, on the other hand, can be explained by the lack of initial implant stability or catastrophic failure of metal or polyethylene materials. Aseptic loosening is still a major problem in cementless design. This could be seen in a recent follow-up report of a carbon fibre-reinforced composite stems, where 92% of the stems were revised due to aseptic loosening at 6 years (Adam et al. 2002). The authors blamed the high rate of loosening on deficient primary stability due to the bad design. Finite element models of joint anatomy can help surgeons understand trauma from repetitive stress, degenerative diseases such as osteoarthritis, and acute injuries. FE models of prosthetic joint implants can provide surgeons and biomechanical engineers with the analytical tools to improve the life-span of implants and improve the clinical outcomes of total hip replacement surgeries (O’Toole et al. 1995). These models are created from many small “elements” of triangular or rectangular shapes. When these 5 finite element (FE) models are loaded with proper boundary conditions, their responses are obtained by solving a set of simultaneous equations that represent the behaviour of the model under load. FE analyses have been widely used in the study of hip joint arthroplasty and in particular the study of hip stem stability. FEA is used to complement the experimental work on micromotion and could even become a useful tool to assess the suitability of implants before surgery (Huiskes et al. 1998; McNamara et al. 1997). One advantage of using FE methods in analysing the stability of hip stems is that it is a non-destructive assessment that can measure the distribution of micromotion along the entire surface of the stem. In-vitro experiments, on the other hand, could only measure micromotion at certain points, and the drilling of holes during specimen preparation could damage and weaken the surrounding bone, thus overestimating the relative motion. FE analysis gives a clearer picture of the stem being analysed and could pointed out ways of improving the stability further. Finite elements have been shown to predict experimental findings and long-term failure mechanisms in orthopaedic surgery with excellent accuracy (Stolk et al. 2003; Tanner et al. 1995). With faster computers and more reliable software, computer simulation is becoming an important tool in orthopaedic research. Future research programmes will use computer simulation to reduce the reliance on animal experimentation, and to complement clinical trials (Prendergast 1997). 1.1 Aims and Objectives Cementless hip stems are widely used and gaining popularity over its cemented counterpart, but the major concern is their stability. Analysing factors that could compromise the stability is crucial to its success, and the valuable information obtained from these analyses could be used to improve the stability and therefore improve the confidence of patients and surgeons alike. This study will concentrate on issues surrounding the stability of cementless hip stems using finite element analyses. 6 It is hoped that this study will provide quantitative and qualitative data to help both surgeons and engineers on issues related to the stability of cementless hip stems, in order to improve its short-term and long-term successes. 7 Chapter 2 Technical Paper Published 1 Conclusions and Recommendations Cementless hip stems are gaining popularity in hip joint arthroplasty but the issues related to their stability are a major concern. This research uses Finite Element Analyses to study various factors that could affect the stability of cementless hip stems. The effect of muscle forces affecting the FE predictions was analysed. Muscle forces should be included in all FE analyses because ignoring them will underestimate the magnitude of micromotion and the surface area unfeasible for bone growth. Another FE parameter studied was the bone material properties. The bone’s elastic modulus was gradually reduced to simulate weaker bone mass. The results showed that as the modulus was reduced, the interface micromotion increased. This project has achieved its objective of simulating failure of cementless hip prostheses. However, there are many areas where further improvements could be made. The analyses were conducted on a standard commercially available finite element package. As such, the results that can be shown are limited to those available within the 8 package. An algorithm tailored to study the micromotion of bone-implant interface would be further analysed. With such a code, there are many aspects of replacement surgery that could be analysed, which includes: • The effect of surface roughness of cementless stems. • The effect of the overall geometry. • The effect of proximal vs distal fixation concept. • The effect of surgical error such as misalignment. • The effect of macrofeatures. • The effect of bone pathology. 9 Bibliography Boss, J. H., Shajrawi, I., Soudry, M., & Mendes, D. G. 1990, "Histological Features of the Interface Membrane of Failed Isoelastic Cementless Prostheses", International Orthopaedics, vol. 14, no. 4, pp. 399-403. Dorr, L. D., Wan, Z. N., & Gruen, T. 1997, "Functional results in total hip replacement in patients 65 years and older", Clinical Orthopaedics and Related Research no. 336, pp. 143-151. Duffy, G. P., Berry, D. J., Rowland, C., & Cabanela, M. E. 2001, "Primary uncemented total hip arthroplasty in patients [lt ]40 years old: 10- to 14-year results using firstgeneration proximally porous-coated implants", The Journal of Arthroplasty, vol. 16, no. 8, Supplement 1, pp. 140-144. Duffy, G. P., Muratoglu, O. K., Biggs, S. A., Larson, S. L., Lozynsky, A. J., & Harris, W. H. 2001, "A critical assessment of proximal macrotexturing on cemented femoral components", Journal of Arthroplasty, vol. 16, no. 8, pp. 42-48. El Warrak, A. O., Olmstead, M. L., von Rechenberg, B., & Auer, J. A. 2001, "A review of aseptic loosening in total hip arthroplasty", Veterinary and Comparative Orthopaedics and Traumatology, vol. 14, no. 3, pp. 115-124. Emery, D., Britton, A., Clarke, H., & Grover, M. 1997, "The Stanmore total hip arthroplasty - A 15- to 20-year follow- up study", Journal of Arthroplasty, vol. 12, no. 7, pp. 728-735. Haber, D. & Goodman, S. B. 1998, "Total hip arthroplasty in juvenile chronic arthritis A consecutive series", Journal of Arthroplasty, vol. 13, no. 3, pp. 259-265. Harris, W. H. 1997, "Options for primary femoral fixation in total hip arthroplasty Cemented stems for all", Clinical Orthopaedics and Related Research no. 344, pp. 118123. Horikoshi, M., Macaulay, W., Booth, R. E., Crossett, L. S., & Rubash, H. E. 1994, "Comparison of Interface Membranes Obtained from Failed Cemented and Cementless Hip and Knee Prostheses", Clinical Orthopaedics and Related Research no. 309, pp. 6987. Huiskes, R., Verdonschot, N., & Nivbrant, B. 1998, "Migration, stem shape, and surface finish in cemented total hip arthroplasty", Clinical Orthopaedics and Related Research no. 355, pp. 103-112. Macdonald, D. A. 1998, "Mini Symposium: Total hip replacement - (i) Risks versus rewards of total hip replacement", Current Orthopaedics, vol. 12, no. 4, pp. 229-231. Mallory, T. H., Lombardi, A. V., Leith, J. R., Fujita, H., Hartman, J. F., Capps, S. G., Kefauver, C. A., Adams, J. B., & Vorys, G. C. 2002, "Why a taper?", Journal of Bone and Joint Surgery-American Volume, vol. 84A, pp. 81-89. McNamara, B. P., Cristofolini, L., Toni, A., & Taylor, D. 1997, "Relationship between bone-prosthesis bonding and load transfer in total hip reconstruction", Journal of Biomechanics, vol. 30, no. 6, pp. 621-630. Nourbash, P. S. & Paprosky, W. G. 1998, "Cementless femoral design concerns Rationale for extensive porous coating", Clinical Orthopaedics and Related Research no. 355, pp. 189-199. Oonishi, H. 1991, "Interfacial reactions to bioactive and non-bioactive bone cements," in The Bone-Biomaterial Interface, J. E. Davies, ed., University of Toronto Press, pp. 321333. Otani, T., Whiteside, L. A., White, S. E., & Mccarthy, D. S. 1993, "Effects of femoral component material properties on cementless fixation in total hip arthroplasty", Journal of Arthroplasty, vol. 8, no. 1, pp. 67-74. O'Toole, I. I. I., Jaramaz, B., DiGioia, I. I. I., Visnic, C. D., & Reid, R. H. 1995, "Biomechanics for preoperative planning and surgical simulations in orthopaedics", Computers in Biology and Medicine, vol. 25, no. 2, pp. 183-191. Pilliar, R. M. 1991, "Quantitative evaluation of the effect of movement at a porous coated implant-bone interface," in The Bone-Biomaterial Interface, 1st edn, J. E. Davies, ed., University of Toronto Press, pp. 380-387. Pilliar, R. M., Lee, J. M., & Maniatopoulos, C. 1986, "Observations on the Effect of Movement on Bone Ingrowth Into Porous-Surfaced Implants", Clinical Orthopaedics and Related Research no. 208, pp. 108-113. Prendergast, P. J. 1997, "Finite element models in tissue mechanics and orthopaedic implant design", Clinical Biomechanics, vol. 12, no. 6, pp. 343-366. Rasquinha, V. J., Dua, V., Rodriguez, J. A., & Ranawat, C. S. 2003, "Fifteen-year survivorship of a collarless, cemented, normalized femoral stem in primary hybrid total hip arthroplasty with a modified third-generation cement technique", Journal of Arthroplasty, vol. 18, no. 7, pp. 86-94. Simmons, C. A., Valiquette, N., & Pilliar, R. M. 1999, "Osseointegration of sintered porous-surfaced and plasma spray- coated implants: An animal model study of early postimplantation healing response and mechanical stability", Journal of Biomedical Materials Research, vol. 47, no. 2, pp. 127-138. Stauffer, R. N. 1982, "10-Year Follow-Up-Study of Total Hip-Replacement - with Particular Reference to Roentgenographic Loosening of the Components", Journal of Bone and Joint Surgery-American Volume, vol. 64, no. 7, pp. 983-990. Stolk, J., Maher, S. A., Verdonschot, N., Prendergast, P. J., & Huiskes, R. 2003, "Can finite element models detect clinically inferior cemented hip implants?", Clinical Orthopaedics and Related Research no. 409, pp. 138-150. Sutherland, C. J., Wilde, A. H., Borden, L. S., & Marks, K. E. 1982, "A 10-Year FollowUp of 100 Consecutive Muller Curved-Stem Total Hip-Replacement Arthroplasties", Journal of Bone and Joint Surgery-American Volume, vol. 64, no. 7, pp. 970-982. Tanner, K. E., Yettram, A. L., Loeffler, M., Goodier, W. D., Freeman, M. A. R., & Bonfield, W. 1995, "Is stem length important in uncemented endoprostheses?", Medical Engineering & Physics, vol. 17, no. 4, pp. 291-296. Tennent, T. D. & Goddard, N. J. 2000, "Current attitudes to total hip replacement in the younger patient: results of a national survey", Annals of the Royal College of Surgeons of England, vol. 82, no. 1, pp. 33-38. Viceconti, M., Monti, L., Muccini, R., Bernakiewicz, M., & Toni, A. 2001, "Even a thin layer of soft tissue may compromise the primary stability of cementless hip stems", Clinical Biomechanics, vol. 16, no. 9, pp. 765-775.