Document 14777309
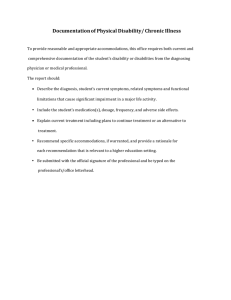
advertisement

Clinical Education Committee March 7, 2014 Minutes Review of Minutes – 2.7.14 -­‐ approved as is Attendance: MEMBER Cullen Hegarty James Nixon ATTENDANCE X X Gary Beaver Yasuko Yamamura Katherine Murray Sheila Specker Robert Acton Cornelius Lam Edward RG Santos Jennifer Hsia Paul Gleich James Pacala CLERKSHIP/ROLE Chair INMD 6805-­‐6806-­‐6807 Essentials of Clinical Medicine 3A-­‐B-­‐C; Process of Care Clerkships EMMD 7500 Emergency Medicine FMCH 7600 Family Medicine MED 7500 Medicine I MED 7501 Medicine II NEUR 7510 Neurology OBST 7500 Obstetrics & Gynecology PED 7501 Pediatrics ADPY 7500 Psychiatry SURG 7500 Surgery NSU 7200 Neurosurgery ORSU 7200 Orthopaedic Surgery OTOL 7200 Otolaryngology UROL 7200 Urology FMCH 7700 Primary Care Selective – Fam Medicine Sally Berryman Michael Kim MED 7700 Primary Care Selective – Medicine MED 7701 Primary Care Selective – Med/Peds X Kathy Brooks Jacob Prunuske Johnathan Valesano Kacia Lee Michael Bambenek Anne Belzowski Mark Rosenberg PED 7700 Primary Care Selective – Pediatrics INMD 7200 Rural Physician Associate Program (RPAP) Duluth Faculty Representative MS4 Student Representative (D) MS4 Student Representative (TC) MS3 Student Representative (D) MS3 Student Representative (TC) Vice Dean for Education X X X X X X Kathy W atson Majka W oods Brooke Nesbitt Chelsey Jernberg Mary Tate Mark Hilliard Barb Blacklock Senior Associate Dean for UME Assistant Dean for ACE Clinical Education Manager, CEC staff Clinical Scheduler Minority Affairs & Diversity Instructional Develpoer Disability Services Keith D. Henry David Power Briar Duffy X X X X X X X X X X X X guest ANNOUNCEMENTS: Best Practices in Medical Education Day -­‐ The Best Practices in Medical Education Day on May 8, 2014 promises to be a day for collaboration and a celebration of all great educational practices we currently have on both the Duluth and Twin Cities Campuses. This is a chance for busy medical educators to network and learn from each other. This year’s event will focus on quality improvement across the continuum of medical education. The Best Practices Day is free and open to all University of Minnesota Medical School faculty, fellows, residents, staff and students. Goals: Share innovations in medical education teaching and learning Offer networking opportunities for medical educators across campuses and affiliate sites Provide an opportunity for the formation of collaboration for educational scholarship All are encouraged to submit proposals, which are still being accepted. For questions, contact Dr Woods. UPDATES: Search Committee for Asst. Dean Clinical Education – The two final candidates will be announced on Monday, March 10. Candidates are coming March 27 2-­‐3pm MT 2-­‐520 and March 28 2-­‐3pm MT 2-­‐520. Streaming will not available, but sessions will be recorded. Please send your comments to Drs Watson or Rosenberg. New Models for Clinical Education -­‐ VA LIC-­‐ Progress continues with discussions both within VALIC group and with related clerkships. SubInternship -­‐ Work underway to partner with sites and other ICU specialities. IPE is also being included as a curriculum item. Class of 2016 will be first group through new SubIntership. EMR Guidelines (Kim) -­‐ Working with informatics at health systems to create standard policies across education sites. DISCUSSION: Disability Services (Barbara Blacklock) Handouts = PPT presentation, Information about Disabilities, Responsibilities for Faculty and Staff, and Medical Students with Disabilities Policy Background: Provide CEC with overview of Disability Services and discuss how stakeholders can work together to provide medical students with disabilities to continue to maximize learning opportunities. DS is part of the Office for Equity and Diversity. Please refer to PPT slides. Interactive Process: DS starts with students making needs known to DS. DS gathers all medical information from licensed providers to determine if student has a disability and gathers information about courses (including clinical courses) to determine potential reasonable accommodations. If at anytime you receive a letter from a student requesting accommodations that seem unreasonable or not feasible, please contact DS to brainstorm options so that student will still meet requirements of course/program. Structure: DS has offices for Student Services (incl. medical students) and Employee Services/UReturn (incl. residents and fellows). Four support units cover both groups -­‐ Testing Center, Document Conversion, Interpreting and Captioning Unit, and Computer Accommodations. Definition of Disability: ADAA. Health providers are asked about impairment AND impact on life activities. Medical Students registered with DS: Numbers have remained consistent since 2009 at around 50 per year. Referral brochures available. Types of Disabilities: Largest amount fall within Mental Health, ADHD, Learning Disabilities, and Chronic Health. Other types include Physical, Sensory, and Brain Injury. -­‐Apparent -­‐Nonapparent Determining Reasonable Accommodations: questions that are asked by DS -­‐ including "Would the accommodations compromise the essential elements of the curriculum or present a safety concern?" Meaningful Access: Environments = physical, informational, program/policy, attitudinal. **Common Accommodations: Vary based on disability need, but in clinical courses commonly include testing accommodations (including Shelf exams), modified schedule (time away for appointments, etc), flexibility to stand/sit, extra time for communication (processing, speech impediments), sites on bus routes. Student must still meet all essential requirements of the course. Role of DS: medical documentation, determinations of disability, assist with implementation of accommodations, communications, modifications as needed, consultation and problem-­‐solving with faculty, staff, and providers. Role of Faculty: participate in process to determine and implement accommodations based on requirements of course/clerkship, communicate the essential elements of course, contact DS with issues and concerns. Role of Student: make needs known, provide documentation, engage in process, discuss accommodation needs with faculty, inform DS of changes if needs change or accommodations are ineffective. DS located in McNamara. Links and resources on the meded.umn.edu website also for students. Q&A -­‐ Dr Hsia asked how and when students are to initiate discussion with clerkship about their accommodation request. Please refer the the Medical School's Medical Students with Disabilities policy for student procedure. Deb Egger-­‐Smith asked about privacy concerns; if coordinator receives letter, it is understood that that information will be shared with site director or necessary educators (residents, attendings, etc). Dr Kim asked how long the process takes. Ms Blacklock shared that it can go as quickly as first contact Monday, documentation received Wednesday, accommodations scripted on Thursday. In other cases, it will vary on how long it takes to receive documentation or if initial testing is still underway. Generally, it does not take very long. Sometimes the need for an accommodation is not identified until the student is already underway with a clinical rotation. DS does have a referral tool that clerkships could use to determine if they should refer a current student to DS or other services to address potential health concerns that could necessitate accommodations. Dr Prunuske asked to confirm that DS provides services to pre-­‐clinical students (Yes). What is process for current Duluth students preparing for TC clinical rotations? Thank you to Ms. Blacklock for her presentation and resources. UPDATES (cont): PxDx -­‐ Procedure and Diagnosis tracking being converted from EValue to new LMS system, LCMS+. That "patient encounter tracking" is much more streamlined and easy to use/track. Dr Woods will continue to collect procedures and diagnoses from clerkships to create list that will be used by students. Dr Hegarty asked for clarification on the purpose of the procedure/diagnosis tracking -­‐ graduation requirement? Dr Woods says that discussion is still open on the purpose of procedure/diagnosis training. The Medical School has never historically tracked procedures/diagnoses -­‐ if we are going to do this, it must be easy for students, appropriately designed (both the list and the tool), and use of data. Kacia Lee asked that tool be designed specifically as yes/no, to what extent, location, simulation vs. actual patient, etc. Intent must be clear. Dr Brooks added that it must be clear to students that there are a set of procedures/diagnoses that are general graduation requirement AND/OR specific to one clerkship. Students need to know where to track their patient encounters. Dr Kim pondered if a different approach could be as a professional perspective. Kacia Lee shared problem with professionalism equaling quantity. Some sites don't have as many opportunities; Dr Kim countered that as a clerkship director, he would want to know if a student was not having enough patient encounters. Dr Hegarty asked for game plan between now and when new system is ready. Dr Woods wants to return in May to continue discussion on Patient Encounter Tracking. Dr Duffy also asked for clerkships to then receive an annual report of the patient encounters inputted by students in their clerkship/site. **Dr Gleich asked for progress update on LCMS+. Mark Hilliard and Brooke Nesbitt are coordinating the training model for coordinators and their respective clerkships. Mark updated group that access, servers, x500 sign-­‐on, MedIS links have all progressed. Coordinators have had "student access" and will receive course director/coordinator level access shortly. Med Ed Retreat Follow-­‐Up -­‐ Constituents from Medical School and the community convened at the State of Med Ed Retreat in February. Retreat was designed to bring groups together to discuss current state of healthcare, current curriculum, and innovations for bringing two closer together to improve medical education (quality improvement, integration, interprofessionalism, etc). A pre-­‐retreat survey showed mostly consensus on topics like patient safety and integration. Dr Rosenberg shared that a 42-­‐page report was collected based on the retreat discussions; this has been summarized into shorter themes report that will be disseminated. Work and discussions on these themes will be communicated to all constituents. Thank you to everyone who attended and/or have signed up for work groups. Please send any questions or ideas to Dr Rosenberg. STUDENT ISSUES/CONCERNS: Match Day in TWO WEEKS! Monday students hear yes/no; on Friday, yes-­‐students will receive actual placements. Thursday and Friday are excused absences for MS4 students (pre-­‐Match day and Match day). Next meeting: April 4, 2014 = Joint Session CEC/SFC 3.7.14 BWN