Document 14777304
advertisement

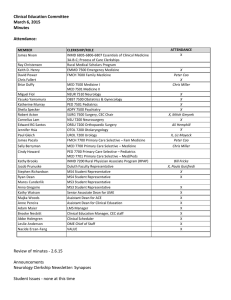
Clinical Education Committee September 5, 2014 Minutes MEMBER James Nixon Miguel Fiol Yasuko Yamamura Katherine Murray Sheila Specker Robert Acton Cornelius Lam Edward RG Santos Jennifer Hsia Paul Gleich James Pacala CLERKSHIP/ROLE INMD 6805-­‐6806-­‐6807 Essentials of Clinical Medicine 3A-­‐B-­‐C; Process of Care Clerkships EMMD 7500 Emergency Medicine FMCH 7600 Family Medicine MED 7500 Medicine I MED 7501 Medicine II NEUR 7510 Neurology OBST 7500 Obstetrics & Gynecology PED 7501 Pediatrics ADPY 7500 Psychiatry SURG 7500 Surgery, CEC Chair NSU 7200 Neurosurgery ORSU 7200 Orthopaedic Surgery OTOL 7200 Otolaryngology UROL 7200 Urology FMCH 7700 Primary Care Selective – Fam Medicine Sally Berryman Michael Kim MED 7700 Primary Care Selective – Medicine MED 7701 Primary Care Selective – Med/Peds Cindy Howard Kathy Brooks Jacob Prunuske Stephen Richardson Ryan Dean Maros Cunderlik Anna Gregoire Mark Rosenberg PED 7700 Primary Care Selective – Pediatrics INMD 7200 Rural Physician Associate Program (RPAP) Duluth Faculty Representative MS4 Student Representative MS4 Student Representative MS3 Student Representative MS3 Student Representative Vice Dean for Education Kathy Watson Anne Pereira Majka Woods Suzanne van den Hoogenhof W. Scott Slattery Brooke Nesbitt Senior Associate Dean for UME Assistant Dean for Clinical Education Assistant Dean for ACE Measurement Specialist, Assessment & Evaluation Director, Learner Development Clinical Education Manager, CEC staff Keith D. Henry David Power Briar Duffy ATTENDANCE X X X X X X X X X, Mitch Gmyrek X X Chrissy Redding X Bill Fricke X, Paula Guisfredi X X X X X X X X Minutes -­‐ Approved as is. No announcements at this time. OB Clerkship Pilot Update Triggered by lack of enough capacity at OB sites. Established a new rotation schedule that upped capacity from 7 to 12. Began in January 2014, data = please refer to handouts. Now that change has been made, how are students doing? Comparing comments from 14-­‐15 evaluations, compared to previous years does not show significant difference. Grades, shelf scores, and feedback remain consistent with previous schedule format. With this change, Dr Yamamura anticipates being able to accommodate all MS3 students in ~ five years. Discussions continue about whether the schedule is as good for learning, so it is uncertain at this time if this will be a long term change. Dr Kim asked if students interested in OB as specialty feel they are getting enough experiences? Dr Yamamura indicated that the OB Sub-­‐Internship is bursting at the seams with full enrollment. If a student wanted more time within L&D, or with particular preceptor, they would have to get that experience outside of the core clerkship. Dr Acton inquired if any of the OB sites could increase their capacity (like those that take one student). Dr Yamamura responded that those placements are with an individual preceptor (private practitioners), not the whole site, so increasing capacity is not likely. Ryan Dean inquired if larger sites, like HCMC and Regions, could insert education week in order to increase capacity. Dr Yamamura responded that they were asked, but declined to implement an education week. Dr Acton commended Dr Yamamura on her creativity to crunch the numbers and adjust the clerkship in order to ensure all students get the OB clerkship experience they need for graduation. Dr Pereira indicated that she has met with most of the clerkship directors and is cognizant of the need for increased capacity, though not at the risk of making precepting more difficult. She is reaching out to site directors and groups to brainstorm options. ACS/ASE -­‐ see flyer. Group at ASC (including Dr Acton) created 25 modules for simulation-­‐based surgical skills curriculum. Each module includes assessment of the hands-­‐on component and can be implemented as large group or small groups. Can be used individually or as a longer curriculum. Dr Acton shared that some of the content was being taught in the Surgery core clerkship, and will be transitioning to using the actual ACS modules for those areas (2 and 3) starting period 4. Students will do them in the simulation center during the clerkship. Curriculum supplements the content in the advanced surgery rotation. The ACS modules could be integrated into any clerkships; nationally, authors intend for schools to decide where it fits best in the curriculum. Dr Nixon indicated that several content areas in ECM could be enhanced by using one or more of these modules, such as the male/genital/rectal exam. Dr Acton added that the modules can be implemented at incredibly low cost. Workgroup Update -­‐ Public Health and Health Policy Survey was sent to course and clerkship directors to assess thoughts about Public Health and Health Policy. Students and residency directors were also surveyed. ECM, FIPCC, and some clerkships and electives were indicated as areas of public health and public policy. Universally, the biggest limitation to integrating public health and health policy was TIME. There isn't extra time waiting in the curriculum to be filled. EXPERTISE, FACULTY, and STUDENT ATTENTION SPANS/INTEREST war also indicated as limitations. Other comments include: "Trying to cover too much in the curriculum makes it difficult to learn any one topic thoroughly" and "Covering topics like public health and health policy distracts from the real work of being a medical student -­‐ namely learning about health and disease and how to practice clinical medicine. " Clearly some students do not view this a core curriculum for medicine. "Adding much more material on public health would require eliminating additional basic science content beyond that already eliminated." "…Why is this important?" Dr Kim noted that one implication of the negative comments may be that as a school, we are not discussing public health enough, given the incredible implication on patient health that public health initiatives do have. Examples of Initiatives currently underway to increase: ECM 1 -­‐ Health Policy module -­‐ 6 hours (Tyler Winkelmen, Ezra Golberstein PhD, David Satin) -­‐ ACTUALLY IN 3A? [Note: this was an innovations contest winner] Family Medicine clerkship -­‐ Process of care assignment -­‐ Innovations Competition committee ideas 2013-­‐2014: FIPCC integration? FCT integration? Elective Curricular: dual degrees, like MD/MPH. (Though MPA not an easy option) and elective courses Non-­‐curricular: Phillips Neighborhood Clinic (acknowledgement by Badge?), interest groups, introduction to Urban Health Equity for incoming MS1s Resources: Health Care Handbook The UW School of Medicine AND Public Health is the epitome of integration; the goal at UMN is not that large-­‐scale, but to make differences to current school with impact. Vision: integration in MS1-­‐MS2 course content and integration into core clerkships (not lecture, but addressing issues during rotation). Dr Prunuske added that more direction is needed from Dr Rosenberg to define the scope for this project -­‐ acknowledge what is already being done and identify the gaps/opportunities to add or integrate public health competencies. Dr Duffy indicated that at UW, students are pulled out every so often to have large group opportunities for teaching/learning; there are current days when our MS3's are pulled out (like MS3 Reflections with FAs) that could be amended to included sessions or opportunities to address public health. Dr Power added that new opportunities that would allow MD-­‐MPH without taking time away from training or to get minor/certificate in PH while doing MD curriculum. Other areas to address beyond the current and gaps, is to define public health objectives more concisely and list and address those objectives in all core clerkships. Dr Prunuske wondered to how best to evaluate public health objectives -­‐ questions on clerkship evaluation? Dr Nixon stated that it IS measured currently on the AAMC Graduation Questionnaire. Dr Prunuske noted that student perception may not be the best item. Student Issues/Questions/Concerns What flexibility in Periods 5 and 6 for interviews? Many students are forced to take required rotations during those periods. Dr Acton indicated that he received many requests for absences (weddings, family activities, etc). He acknowledged that students are put into a bind by the scheduling situation, but that students also can be as mindful and prepared to take absences only when needed and as minimally per absence as needed. Several clerkship directors indicated that in a 6-­‐week period a student could have FIVE DAYS off. Mindful planning must be in place to make best use of those days. Dr Nixon also shared that students can be proactive and communicate with the clerkship to determine what the student can do to make it work. Dr Pereira indicated that interviews may increase per student as some programs become more competitive. Other advice is to be sure to take requireds in Periods 1 and 2. Students may be getting mixed messages about what to schedule during period 5 and what NOT to schedule. Interview season is more than just period 5, even if students may have limited options for when invited to interview. The pre-­‐lottery presentations, specifically about residency planning, may need to be adjusted. Students may be over-­‐stressed because of the mixed messages. Update: Pre-­‐matriculation Course (Dr Scott Slattery) -­‐ please refer to handout 16 total participants participated in an enrichment opportunity designed to optimize academic performance through promotion of protective factors and mitigate the transition flush (academically and culturally) for incoming students, both those that were identified as disadvantaged or from general class population. Program also designed to provide longitudinal support. Nature of pilot program necessitated an assessment of the efficacy of this approach and cost-­‐ effectiveness of program structure. Schedule included welcome, academic strategies, campus exploration, fall course introductions (sample lectures), and applications (resources). Additional elements included "connections" luncheons with MedEd Administration, student groups/councils, and course directors/managers. Assessment/Evaluation based on belonging, self-­‐efficacy, within group comparison, and matched sample exploration. Touchpoints, data, and comments from students included in handout. Dr Acton inquired how this enrichment course was different from the standard MS1 Orientation. The MS1 Orientation has less focus on academic preparation, but does have small sessions on well-­‐being. Dr Acton also mentioned how a similar course could be useful between MS2 and MS3 to help those students that seem to be less prepared for Period 1 and 2 (credentialing, etc). Next meeting: October 3, 2014