Document 14777303
advertisement

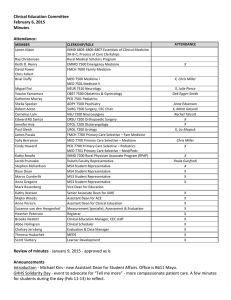
Clinical Education Committee October 3, 2014 Minutes Attendance: MEMBER James Nixon ATTENDANCE Keith D. Henry David Power Briar Duffy Miguel Fiol Yasuko Yamamura Katherine Murray Sheila Specker Robert Acton Cornelius Lam Edward RG Santos Jennifer Hsia Paul Gleich James Pacala CLERKSHIP/ROLE INMD 6805-­‐6806-­‐6807 Essentials of Clinical Medicine 3A-­‐B-­‐C; Process of Care Clerkships EMMD 7500 Emergency Medicine FMCH 7600 Family Medicine X NEUR 7510 Neurology OBST 7500 Obstetrics & Gynecology PED 7501 Pediatrics ADPY 7500 Psychiatry SURG 7500 Surgery, CEC Chair NSU 7200 Neurosurgery ORSU 7200 Orthopaedic Surgery OTOL 7200 Otolaryngology UROL 7200 Urology FMCH 7700 Primary Care Selective – Fam Medicine Sally Berryman Michael Kim MED 7700 Primary Care Selective – Medicine MED 7701 Primary Care Selective – Med/Peds Cindy Howard Kathy Brooks Jacob Prunuske Stephen Richardson Ryan Dean Maros Cunderlik Anna Gregoire Mark Rosenberg PED 7700 Primary Care Selective – Pediatrics INMD 7200 Rural Physician Associate Program (RPAP) Duluth Faculty Representative MS4 Student Representative MS4 Student Representative MS3 Student Representative MS3 Student Representative Vice Dean for Education X X X X X X Kathy Watson Majka Woods Anne Pereira Suzanne van den Hoogenhof Brooke Nesbitt Abbe Holmgren Leslie Anderson Senior Associate Dean for UME Assistant Dean for ACE Assistant Dean, Clinical Education Measurement Specialist, Assessment & Evaluation Clinical Education Manager, CEC staff Clinical Scheduler OME Chief of Staff X X X X X X X X X X, Anne Edvenson X, Mitch Gmyrek X Review of Minutes - September 6 - approved as is Student Issues: Excused Absence Policy Clerkship directors will reach out to MS4 students about interview dates. Ryan Dean shared that students have questions and concerns about the absence policies. Overall, students believe the absence policies are fair, but feel stuck in that they have required clerkships scheduled during interview season. Dr Acton asked if students understand that free-time schedules affect clerkship scheduling; taking off the summers for studying and away rotations shift the scheduled clerkships into interview seasons. Need better advice from MS4 students. Issue less about time off, but rather about the scheduling process. Dr Gleich shared that the medical school and clerkships need to advocate more to residency programs that we do not have the flexibility on this end to accommodate the current process for interviews. Dr Fiol shared that recently a student requested four days off in NEUR 7510 to present out of the country at a conference AND days off for interviews. Dr Watson asked if clerkship directors and site directors could remind their sites of the absence policies. Steve Richardson shared recent case of student who was denied excused absence that was requested for a Step exam. May be an issue of site director not understanding the policies. Dr Acton also added that students should “request” this time off, not announce or inform the clerkship. Being proactive will help both sides come to mutually agreeable schedule. Dr Watson shared that it is premature to plan tracks or prescribed schedules, but changes are and have been made to schedule advising to help students with planning initial schedules and schedule changes. Steve R shared that he met with his advisor to see if his general plan was advisable, but once into the lottery, it didn’t work out the way he planned. Communication with sites - Dr Fiol asked how to improve communication with sites. Neurology has many sites and struggles to connect with their sites. Some think that sites must be educationally comparable, therefore it should not matter what site at which students take a clerkship. But, the reality is that students want particular sites for letters of recommendation and evaluations from specific programs. Dr Specker asked if there could remain a couple clerkships that have site selection, while others become assigned. Conversation continues about the relative importance of site placements. ACTION ITEM - Dr Pereira will meet with students further to develop a strategy for moving forward - both short term and long term. LCME Update: Late Grades New registrar begins October 6, 2014 - Heather Peterson In the interim, please monitor your grade submission compliance. Discussion: Progress Report and Next Steps (Pereira) Follow up from Medical Education Retreat Critical Themes in UME -New models of clinical education -integration of basic science into clinical education - much work has been done to bring clinical into scietific foundation courses, must continue through four year curriculum -active learning -scholarship MedEd Workgroups -Public healtha nd policy -QI and Patient Safety -IPE Outcomes Major Med Ed Projects 14-15 VALUE, begins July 2015 wth emphasis on QI and Patient Safety Medicine Sub-Internship - IPE, as well as other themes EPAC, also begins in 15-16 Integration: Dyads, simulated cases Flipped classroom: Duluth’s new active learning classroom, TC’s ECM-MCI series, pathology) Questions for CEC How can you incorporate these themes into your clerkship? What do you need to know about how students are prepared in these areas BEFORE years 3-4? Dr Acton shared that he doesn’t have time to incorporate an entire lecture, but with list of themes, he could integrated some of them in existing curriculum. Dr Kim added that opportunities exist to more clearly define current objectives (like patient charts) as being part of one of these themes, like patient safety. Identify what you are already doing, and call it out. Dr Prunuske agreed and added that it could be even stronger if there was a core introduction that would lay the foundation for students to make clinical correlations later. Dr Pereira queried the students about their perspective as to how to introduce/teach these themes. Steve Richardson shared that it would be helpful to have an introduction early on. Students are eager to have early clinical experiences and show correlations to clinical practice throughout first- and second-year. Dr Acton asked if it would be useful for each clerkship to do a short-term piece of a longer project on a theme, like QI or Patient Safety. Ryan Dean added that PCS has a similar assignment. Dr Watson asked students how other clerkships are or could be integrating these themes. Ryan shared that much of the current integration is during rounds, as part of the type of questions that the attendings are asking. Its not consistent, but there are faculty that do connect these or similar themes to patient cases. Dr Fiol asked if residents are aware of or part of the work on these themes. Dr Prunuske added that the advantage is that it becomes real, versus artificially inserting bits of the themes. Having a longitudinal project that is meaningful and useful to the student and the system. Dr Power shared that he attended last week’s first MCI session in ECM 1. He was surprised at the amount of statistics that was presented. It was clear that projects, like the EBM project in FMCH, would be an extension of those objectives. If BlackBag continued through the four years, there would be better vertical, spiral integration into the clerkships of topics such as this. He also added that the increased opportunities within Longitudinal Integrated Clerkships (RPAP, VALUE, EPAC, UCAM) are fantastic settings for working more in depth over time within these themses. Dr Duffy added that individual courses are starting from the beginning each time. If there was a longitudinal sequence for each theme, would be modules or something that the students would do the next one for them, regardless of the clerkship they are on. Dr watson added that one proposal for vertical integration was to have a full week off multiple times throughout the clinical years that brought all students back together for basic science integration or addressing these themes. Dr Kim added another schedule option would be a consistent half-day off each week for this instruction. Dr Power noted that one consideration is the students that are placed geographically across the area and how to make it accessible for them. Steve Richardson added that in his current rotation, the quality is already in place; it is difficult to identify a QI project, when the environment is perfectly calibrated. Student would benefit from experiences where they have to figure out the environment themselves, versus coming new in to a system and trying to nit pick their model. Dr Gleich added that he enjoyed the opportunitiy to precept MS1 and MS2 students in ECM-POCC, but the schedule is so restrictive (two half-days only) so it has been difficult to arrange. The curriculum is not so focused on the medicine, but rather on the process of care, which opens an opportunity to look at QI, patient safety, etc. Dr Watson added later that the name - Process of Care - was intentional, but that perhaps over time, the focus on the different processes of care in various clinical environments has been lost. More reflection and expectations that patient relationships, communication, observations of safety behaviors would enhance the experience. Dr Duffy shared that in her medical school experience, she had a longitudinal continuity experience which allowed her to learn and contribute over time. At Hofstra, all students are trained as EMT’s and are challenged to apply clinical skills at the beginning of their medical school career. The opportunity to be clinically relevant enhanced the basic science curriculum and early medical school clinical experiences. Ryan Dean said that in his early simulation experiences, he can now identify more that he could have done, but that he didn’t know as much as he knows now about how and what to contribute to the team experience. Dr Gleich noted that for students coming in to his clinic, its not a simulation! Its real and the students can contribute and be useful to immediate patient care. Dr Prunuske added, though, that in simulation, students can FAIL, and learn from those failures. Dr Prunuske then queried how often students are attending faculty and business meetings at their sites while on clerkship rotations. Those meetings are often the setting for discussions about process of care and the critical themes. Dr Kim added that attending these meetings over time (during LICs) would be even more beneficial than attending one during a clerkship period. Steve Richardson also questioned the possiblity of increasing opportunities for students to observe or interact with patients outside of the structured curriculum. Dr Kim shared that there are patient advisory boards at most hospitals or in the health systems; that might be an avenue for this. Student Use of EHR AAMC article Handout - New UMMC Med Student Team Note (brought by Dr Kim; he will email to all clerkship directors) Medical Student is communication note. Resident is billing note. Resident must confirm that the student note is accurate. Attending confirms the entire note is accurate and then adds attestation. Group worked aggressively to promote this format to the other teaching hospitals. Although everyone agreed that this was a good idea, no one was able to get it past their informatics board. Coders were uncomfortable not knowing to whom to attribute things. This new has separate columns which helps to differentiate between student and resident notes. Medico-legal advisors are universally risk-averse, so even though the solution was presented clearly to address problem, it was not accepted. Dr Kim is continuing work to reconvene these groups to continue advocating. Leslie Anderson asked if there was any data from the change at UMMC that would be helpful in presenting to the other teaching hospitals. Dr Kim responded that data had not yet been collected, but agreed it would be useful. Dr Acton added that a great motivator is the national and federal efforts and compliance standards. Dr Kim concluded that focus must remain on the communication for students, while residents and attendings can focus on billing and coding. Dr Watson added that there are conversations occurring around EHR teaching and training, writing down the assessment, differential diagnosis, etc. Then, more advanced use around EHR, how to use the data, etc. We must take critical look at scope and sequence of EHR objectives in curriculum, as well as professionalism integration and applications. Increase teaching and training of EHR prior to clerkships and standardization of expectations for notes, may reduce the need for on-site training during each clerkship. Dr Kim could use help from administration and directors, as well as student input, to further initiative. Next meeting: November 7, 2014 Finish EMR discussion - what to document and how Assessment & Evaluation