1 What is an Atypical Parkinsonian Disorder? Irene Litvan Classification
advertisement

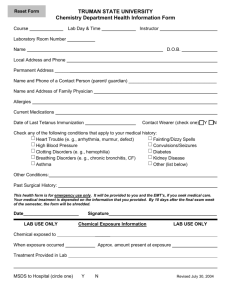
Classification 1 1 What is an Atypical Parkinsonian Disorder? Irene Litvan INTRODUCTION A parkinsonism is a syndrome defined by akinesia associated with rigidity or rest tremor. The akinesia can be expressed as motor slowness (bradykinesia) or as a paucity of movement (hypokinesia), i.e., difficulty in the initiation of or decreased amplitude of movements such as arm swing or facial expression. This syndrome is usually the result of a dysfunctional nigrostriatal pallidal pathway. Impairment of postural reflexes is not included as one of the features of the parkinsonian syndrome since abnormal postural reflexes are generally the consequence of dysfunction of other motor pathways. There are a variety of causes of parkinsonism, but Parkinson’s disease (PD) is the most common (Fig. 1). Although there is extensive literature on PD, this is one of the few books dedicated to the remaining atypical parkinsonian disorders.To appropriately diagnose PD, one should be aware of when to suspect that a patient does not have PD and may be suffering from one of these atypical disorders. The “atypical parkinsonian disorders” (previously known as “Parkinson plus syndromes”) are characterized by a rapidly evolving parkinsonism that has a poor or transient response to dopaminergic therapy and often associates with one or more atypical features for PD. Some of these features include early presence of postural instability, early autonomic failure, vertical supranuclear gaze palsy, pyramidal or cerebellar signs, alien limb syndrome, and apraxia (Table 1; see corresponding video segments on accompanying DVD). Making the distinction between these two major groups of disorders is critical for both clinical practice and research because the prognosis and treatment of patients with an atypical parkinsonian disorder and those with PD differ (1–4). In the clinical setting, although patients with PD may have an almost normal life-span if treated appropriately (4–6), those with atypical parkinsonian disorders have a shorter survival time and more complications occur at early stages and are frequently more severe (3,7–10) (see Table 2 for an example). Moreover, indicated therapies (particularly surgical approaches) differ significantly since some may not be indicated to treat patients with atypical parkinsonian disorders. Until recently, clinicians would “lump” all the atypical parkinsonian disorders together and would only distinguish between this group and PD. However, the need for early identification of the different atypical parkinsonian disorders is becoming increasingly recognized (11), as their prognosis, complications, and survival differ (3,7,8,12–19). For research, this distinction is crucial; homogenous groups are a necessity for studies that lead to firm conclusions. Genetic, analytical, epidemiological, and clinical trials require the inclusion of accurately diagnosed patients. However, diagnosis of the atypical parkinsonian disorders can be at times challenging (20–25) since these disorders may have similar presentations at early disease stages From: Current Clinical Neurology: Atypical Parkinsonian Disorders Edited by: I. Litvan © Humana Press Inc., Totowa, NJ 1 2 Litvan Fig. 1. PSP, progressive supranuclear palsy; CBD, corticobasal degeneration; MSA, multiple system atrophy; DLB, dementia with Lewy bodies; FTDP-17, frontotemporal dementia with parkinsonism linked to chromosome 17; SCAs, spinocerebellar atrophy; NBIA, Neurodegeneration With Brain Iron Accumulation, previously called Hallervorden–Spatz Syndrome; HIV, human immunodeficiency virus. Table 1 When Should an Atypical Parkinsonian Disorder be Suspected? Features suggestive of an atypical parkinsonian disorder Motor Rapid disease progression Early instability and falls Absent, poor, or not maintained response to levodopa therapy Myoclonus Pyramidal signs Cerebellar signs Early dysarthria and/or dysphagia Early dystonia/contractures (unrelated to treatment) Autonomic Features Impotence/decreased genital sensitivity in females Early orthostatic hypotension unrelated to treatment Early and/or severe urinary disturbances Oculomotor Marked slowing of saccades Difficulty initiating saccades, gaze (oculomotor apraxia) Supranuclear gaze palsy Nystagmus Cognitive and behavioral Early and severe frontal or cortical dementia Visual hallucinations not induced by treatment Ideomotor apraxia Sensory or visual neglect/cortical disturbances Classification 3 Table 2 Progression of Various Parkinsonian Disorders Disorder PD CBD DLB MSA PSP Sample Size (N) Median Age at Onset (yr) 18 13 11 15 24 60 64 65 56 65 Median HY II Latencies (mo) 36* 25 12 0 — Median HY III Latencies (mo) 66** 42 43 3 0 Median HY IV Latencies (mo) 166** 55 45 56 38 Median HY Median survival V Latencies After HY V Onset (mo) (mo) 179** 62 59 73 56 12 43 12 10 9 Modified from Muller et al., with permission (17). *p < 0.05; **p < 0.001 Parkinson‘s disease (PD) vs atypical parkinsonian disorders (CBD, DLB, MSA, PSP), (Mann– Whitney U Test). PD patients had a significantly longer latency to each Hoehn and Yahr (HY) stage than those with atypical parkinsonian disorders, confirming the more rapid progression of motor disability in patients with atypical parkinsonian disorders. Most MSA and PSP patients developed postural instability with or without falls significantly earlier than those with CBD and DLB. Postural instability and falls are the most common initial symptoms in PSP, and almost all PSP patients developed an HY stage III within 1 yr of motor onset. The majority of MSA (67%), the majority of DLB (55%), and 38% of CBD patients also reached this stage early. (i.e., progressive falls, parkinsonism not responsive to dopaminergic therapy). Tell-tale signs may take 2 to 4 yr after symptom onset to develop, or early features may be either disregarded or misdiagnosed by clinicians. Misdiagnosis of these disorders is frequent, as patients exhibit a variety of symptoms that may lead them to be initially evaluated by internists or specialists (e.g., ophthalmologists, urologists, neurologists, psychiatrists, neurosurgeons). For example, it is not unusual for a patient with progressive supranuclear palsy (PSP) to be evaluated by several ophthalmologists (and have their glasses changed several times) or to have multiple unnecessary studies for evaluating the cause of their falls prior to being seen by a neurologist. Similarly, patients with corticobasal degeneration (CBD) may present after unsuccessful carpal tunnel surgery, or those with multiple system atrophy (MSA) may present only after failed prostate surgery; in both cases these types of surgery can worsen the patients’ symptoms. Diagnostic accuracy would greatly improve, however, if clinicians from different disciplines would have a broader knowledge of the typical and atypical presentations of these disorders and use proposed clinical diagnostic criteria (26). In the absence of biological markers and known pathogenesis, current diagnosis requires the presence of certain clinical features that allow for clinical diagnosis and eventual pathologic verification. As a result, diagnostic accuracy requires that both clinical and pathological sets of diagnostic criteria be valid and reliable (27,28). Neuropathologic diagnostic criteria for most parkinsonian disorders have been validated and standardized (27,29); the exceptions are those for dementia with Lewy bodies (DLB) and PD with later onset dementia (PDD). Similarly, recently the clinical diagnostic criteria have undergone the same process of rigorous operationalization and validation for most of these disorders (26,30–35). Though consensus for the diagnosis of several of these disorders has been put forward (30–33), and validation studies of diagnostic criteria have been performed for most of the atypical parkinsonian disorders (36), refinement of the criteria is still needed (36). In practice, clinicians are exposed to patients who exhibit different parkinsonian disorders, and so validation studies should compare the accuracy of several sets of criteria with neuropathology. The Scientific Issue Committee of the Movement Disorder Society created a task force to critically review the accuracy of different sets of diagnostic criteria for parkinsonian disorders (36). The task force analyzed how well each set of diagnostic criteria identified all subjects with the disease as having the disease (i.e., sensitivity); identified sub- 4 Litvan Table 3 Validity of the Clinical Diagnostic Criteria for PSP, MSA, DLB, and VaD Disorder Criteria PSP MSA Blin et al. (47) Probable/Possible Blin et al. (47) Probable/Possible-1st visit Probable/Possible-last visit Clinician’s own criteria First visit Last visit Collins et al. (51) Probable/Possible Golbe et al. (49) First visit Last visit Golbe et al. (49) Lees (48) First visit Last visit Lees (48) NINDS-SPSP Probable/Possible NINDS-SPSP Probable/Possible Queen Square Movement Disorder neurologists diagnosis Tolosa et al. (50) Probable/Possible Clinician’s own criteria First visit Last visit Clinician’s prospective diagnosis in life First visit Last visit Consensus Criteria (55) Probable/Possible Consensus Criteria (55) Probable/Possible Queen Square movement disorder neurologist’s diagnosis Quinn (54) Probable/Possible Quinn (54) Probable/Possible Sensitivity (%) Specificity (%) Positive Predictive Value (%) 21/63 100/85 100/63 Litvan et al. (29) 24/83 13/34 55/89 100/98 94/74 100/85 73/50 Litvan (19) 24/105 72 80 93 92 76 76 25/42 100/92 100/67 Litvan et al. (19) Litvan et al. (29) 49 67 50 97 94 98 85 76 92 53 78 95 87 77 65 Author Litvan et al. (19) n/n TOTAL 24/105 24/83 24/105 24/83 24/105 Litvan (29) Litvan et al. (29) Lopez (25) 58 95 82 24/83 50/83 100/93 100/83 62/75 100/98.5 100/96 84.2 96.8 80 54/54 98/98 93/93 Hughes (52)* Litvan (19) 56 69 96.6 97 75.5 80 Litvan et al. (21) 16/105 22 100 92 86 Oaski et al. (33) 51/59 16/28 100/93 63/92 91/86 88 86 Hughes et al. (52)* 34/143 37/63 95/82 94/98 87/86 24/83 8/40 20/143 24/83 (continued) Classification 5 Table 3 (continued) Validity of the Clinical Diagnostic Criteria for PSP, MSA, DLB, and VaD Disorder Criteria DLB VaD Quinn (54) Probable/Possible First visit CERAD CDLB (30) CDLB (30) First visit Last visit CDLB(30) CDLB(30) CDLB (30) Probable/Possible CDLB (30) Probable/Possible CDLB (30) Probable/Possible CDLB (30) Probable/Possible CDLB (30) Clinician’s own criteria First visit Last visit Clinicians own criteria First visit Last visit Queen Square movement disorder neurologists’ diagnosis Sensitivity (%) Specificity (%) Positive Predictive Value (%) Author n/n TOTAL 44/53 97/79 68/30 Litvan et al. (53) 16/105 75 75 50 79 100 Mega (56) Mega (56) 4/24 4/24 17.8 28.6 22 57 NR 100 90 75 55.8 100 91 14/105 9/80 35/56 61/89 84/23 48/23 Litvan (62) Holmes (57) Luis (58) Verghese (59) 0/34 100/94 NA/55 8/40 83/83 95/91 96/92 Lopez (25) McKeith (64) 100/100 30.7 8/0 100 83/NA Hohl (60) Lopez (34)* 5/10 13/26 17.8 28.6 99 99 75 55.8 Litvan (61) 14/105 35 48 99.6 99.6 80 100 Litvan (62) 10/105 25 98.6 33.3 Hughes et al. (52)* 3/143 18/94 29/50 Revised from Litvan et al. (36). *Prospective studies. Note that all other studies are retrospective. CDLB, consensus criteria for dementia with Lewy bodies. jects without the disease as not having the disease (i.e., specificity); and provided reasonable estimates of disease risk (i.e., positive predictive value or PPV). See summary table (Table 3) and refer to the actual publication (36) and specific disease-related chapters in this book for detailed comments. Overall, most of these criteria are specific but not very sensitive. It is worth noting that a validation of pathologic and clinical diagnostic criteria for PD is still needed. Standardization of diagnostic criteria, clinical scales, and identification of outcome measures (37,38) set the stage for conducting appropriate clinical trials. CLASSIFICATION OF ATYPICAL PARKINSONIAN DISORDERS Atypical parkinsonian disorders can be caused by primary or secondary diseases (see Fig. 1). The primary causes consist of neurodegenerative processes such as PSP, CBD, MSA, DLB, and PDD. Interestingly, one of the earlier historical cases thought to have the typical features of PSP was recently found to have a midbrain tumor through autopsy examination. As discussed in Chapter 23, secondary causes also include drugs, infections, toxins, or vascular disease (21,23,39–44). 6 Litvan Table 4 Classification of Atypical Parkinsonian Disroders Tauopathies Progressive supranuclear palsy Corticobasal degeneration Lytico-bodig disease West-French Indies parkinsonian disorder Frontotemporal dementias with parkinsonism linked to chromosome 17 Synucleinopathies Parkinson’s disease Multiple system atrophy Dementia with Lewy bodies Parkinson disease and dementia Neurodegeneration with brain iron accumulation An alternative classification (mostly helpful for research and future therapeutic approaches rather than for clinical use) considers the type of aggregated proteins in the brain lesions and classifies these disorders as tauopathies and synucleinopathies (Table 4; see also Chapters 4 and 8). Commonalities in clinical, biological, or genetic findings question the nosological classification of some of these disorders; for further information the reader is referred to Chapters 8 and 9. PSP and DLB/PDD are the most frequent neurodegenerative primary cause of an atypical parkinsonian disorders (31,45–47). A good history and physical examination will rule out drug-induced atypical parkinsonian disorders and supports the diagnosis of these specific disorders (Chapter 10). Each disorder is specifically covered in Chapters 18–23. The role of ancillary and laboratory tools to assist in the diagnosis of these disorders is discussed in Chapters 11–16 and 24–27. Ancillary tests (e.g., neuroradiologic or cerebrospinal studies) also help with the diagnosis of disorders caused by vascular diseases, tumors, or infection (e.g., Whipple’s disease, Creutzfeldt–Jakob disease, human immunodeficiency virus). Specific therapeutic and rehabilitation approaches for all of these disorders are provided in each disease chapter and an overview of future biologic and rehabilitation approaches is provided in Chapters 28 and 29. It is our expectation that this book will continue to improve the accuracy of the diagnosis of these disorders by raising awareness of their different presentations and by increasing diagnosticians’ index of suspicion. An early and accurate diagnosis will allow better management of these patients and increase research potential. There has been a tremendous increase in our knowledge concerning the proteins that characterize and aggregate in the brain in each of these disorders. Moreover, animal models are now available to help test potential new therapies (see Chapters 5 and 6). Hence, in addition to serving as a reference source, it is hoped that this book will stimulate new investigators to join us in the search for answers to the multiple questions raised throughout the book and in the battle against these disorders. It is anticipated that a better understanding of these diseases, their nosology, and etiopathogenesis (see Chapters 3–9) will lead to better management, quality of life (see Chapter 17), and treatment for patients who suffer them. We anticipate that the eradication of these devastating diseases from the face of the earth will occur in not such a remote future. VIDEOTAPE Postural Instability: Video segment shows a patient with a history of falls and an impaired postural reflex with the backward pull test. The patient would have fallen, unless aided by the examiner. The gait is stable but slightly wide-based. Supranuclear gaze palsy: This patient shows a severe limitation in the range of ocular motor movements observed, which affects more upward than downward voluntary and pursuit gaze. As observed, the oculocephalic reflex is preserved when the the doll’s head maneuver is performed. Slowing of vertical saccades: Patient shows markedly slow vertical saccades and relatively preserved horizontal saccades. Classification 7 Ocular motor apraxia: The patient shows difficulty initiating the voluntary gaze and saccades but exhibits a preserved pursuit and optokinetic nystagmus. Once the saccades are initiated their speed is normal. Corticosensory deficits: This patient shows right sensory neglect and agraphesthesia. These lateralized cognitive features in conjunction with the progressive development of a right ideomotor apraxia, dystonia, and stimulus sensitive myoclonus led to the diagnosis of corticobasal degeneration (corticobasal syndrome). Limb kinetic apraxia: The performance of this patient does not improve with imitation. Movements are coarse and do not represent the intended action. Blepharospasm: Difficulty opening the eyes because of inhibition of eyelid opening, which is followed by blepharospasm. REFERENCES 1. Litvan I. Parkinsonian features: when are they Parkinson disease? JAMA 1998;280:1654–1655. 2. Wenning GK, Ebersbach G, Verny M, et al. Progression of falls in postmortem-confirmed parkinsonian disorders. Mov Disord 1999;14:947–950. 3. Muller J, Wenning GK, Verny M, et al. Progression of dysarthria and dysphagia in postmortem-confirmed parkinsonian disorders. Arch Neurol 2001;58:259–264. 4. Elbaz A, Bower JH, Peterson BJ, et al. Survival study of Parkinson disease in Olmsted County, Minnesota. Arch Neurol 2003;60:91–96. 5. Mortality in DATATOP: a multicenter trial in early Parkinson’s disease. Parkinson Study Group. Ann Neurol 1998;43:318–325. 6. Scigliano G, Musicco M, Soliveri P, et al. Mortality associated with early and late levodopa therapy initiation in Parkinson’s disease. Neurology 1990;40:265–269. 7. Wenning GK, Ben-Shlomo Y, Magalhaes M, Daniel SE, Quinn NP. Clinicopathological study of 35 cases of multiple system atrophy. J Neurol Neurosurg Psychiatry 1995;58:160–166. 8. Wenning GK, Litvan I, Jankovic J, et al. Natural history and survival of 14 patients with corticobasal degeneration confirmed at postmortem examination. J Neurol Neurosurg Psychiatry 1998;64:184–189. 9. Ben-Shlomo Y, Wenning GK, Tison F, Quinn NP. Survival of patients with pathologically proven multiple system atrophy: a meta-analysis. Neurology 1997;48:384–3893. 10. Nath U, Ben-Shlomo Y, Thomson RG, Lees AJ, Burn DJ. Clinical features and natural history of progressive supranuclear palsy: A clinical cohort study. Neurology 2003;60:910–916. 11. Siderowf A, Quinn NP. Progressive supranuclear palsy: setting the scene for therapeutic trials. Neurology 2003;60:892–893. 12. Litvan I, Mangone CA, McKee A, et al. Natural history of progressive supranuclear palsy (Steele–Richardson– Olszewski syndrome) and clinical predictors of survival: a clinicopathological study. J Neurol Neurosurg Psychiatry 1996;60:615–6120. 13. Maher ER, Lees AJ. The clinical features and natural history of the Steele–Richardson–Olszewski syndrome (progressive supranuclear palsy). Neurology 1986;36:1005–1008. 14. Watanabe H, Saito Y, Terao S, et al. Progression and prognosis in multiple system atrophy: an analysis of 230 Japanese patients. Brain 2002;125:1070–1083. 15. Wenning GK, Geser F, Stampfer-Kountchev M, Tison F. Multiple system atrophy: an update. Mov Disord 2003;18(Suppl 6):S34–S42. 16. Wenning GK, Braune S. Multiple system atrophy: pathophysiology and management. CNS Drugs 2001;15:839–852. 17. Muller J, Wenning GK, Jellinger K, McKee A, Poewe W, Litvan I. Progression of Hoehn and Yahr stages in Parkinsonian disorders: a clinicopathologic study. Neurology 2000;55:888–891. 18. Wenning GK, Ben Shlomo Y, Magalhaes M, Daniel SE, Quinn NP. Clinical features and natural history of multiple system atrophy. An analysis of 100 cases. Brain 1994;117(Pt 4):835–845. 19. Golbe LI. The epidemiology of PSP. J Neural Transm Suppl 1994;42:263–273. 20. Litvan I, Agid Y, Jankovic J, et al. Accuracy of clinical criteria for the diagnosis of progressive supranuclear palsy (Steele–Richardson–Olszewski syndrome). Neurology 1996;46:922–930. 21. Litvan I, Agid Y, Goetz C, et al. Accuracy of the clinical diagnosis of corticobasal degeneration: a clinicopathologic study. Neurology 1997;48:119–125. 22. Litvan I, Goetz CG, Jankovic J, et al. What is the accuracy of the clinical diagnosis of multiple system atrophy? A clinicopathologic study. Arch Neurol 1997;54:937–944. 8 Litvan 23. Boeve BF, Maraganore DM, Parisi JE, et al. Pathologic heterogeneity in clinically diagnosed corticobasal degeneration. Neurology 1999;53:795–800. 24. Wenning GK, Ben-Shlomo Y, Hughes A, Daniel SE, Lees A, Quinn NP. What clinical features are most useful to distinguish definite multiple system atrophy from Parkinson’s disease? J Neurol Neurosurg Psychiatry 2000;68:434–440. 25. Bhatia KP, Lee MS, Rinne JO, et al. Corticobasal degeneration look-alikes. Adv Neurol 2000;82:169–182. 26. Lopez OL, Litvan I, Catt KE, et al. Accuracy of four clinical diagnostic criteria for the diagnosis of neurodegenerative dementias. Neurology 1999;53:1292–1299. 27. Litvan I, Hauw JJ, Bartko JJ, et al. Validity and reliability of the preliminary NINDS neuropathologic criteria for progressive supranuclear palsy and related disorders. J Neuropathol Exp Neurol 1996;55:97–105. 28. Litvan I. Methodological and research issues in the evaluation of biological diagnostic markers for Alzheimer’s disease. Neurobiol Aging 1998;19:121–123. 29. Dickson DW, Bergeron C, Chin SS, et al. Office of Rare Diseases neuropathologic criteria for corticobasal degeneration. J Neuropathol Exp Neurol 2002;61:935–946. 30. Litvan I, Agid Y, Calne D, et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele– Richardson–Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology 1996;47:1–9. 31. McKeith IG, Galasko D, Kosaka K, et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology 1996;47:1113–1124. 32. McKeith IG, Perry EK, Perry RH. Report of the second dementia with Lewy body international workshop: diagnosis and treatment. Consortium on Dementia with Lewy Bodies. Neurology 1999;53:902–905. 33. Gilman S, Low P, Quinn N, et al. Consensus statement on the diagnosis of multiple system atrophy. American Autonomic Society and American Academy of Neurology. Clin Auton Res 1998;8:359–362. 34. Osaki Y, Wenning GK, Daniel SE, et al. Do published criteria improve clinical diagnostic accuracy in multiple system atrophy? Neurology 2002;59:1486–1491. 35. Lopez OL, Becker JT, Kaufer DI, et al. Research evaluation and prospective diagnosis of dementia with Lewy bodies. Arch Neurol 2002;59:43–46. 36. Litvan I, Bhatia KP, Burn DJ, et al. SIC Task Force appraisal of clinical diagnostic criteria for parkinsonian disorders. Mov Disord 2003;18:467–486. 37. Goetz CG, Leurgans S, Lang AE, Litvan I. Progression of gait, speech and swallowing deficits in progressive supranuclear palsy. Neurology 2003;60:917–922. 38. Tison F, Yekhlef F, Balestre E, et al. Application of the International Cooperative Ataxia Scale rating in multiple system atrophy. Mov Disord 2002;17:1248–1254. 39. Averbuch-Heller L, Paulson GW, Daroff RB, Leigh RJ. Whipple’s disease mimicking progressive supranuclear palsy: the diagnostic value of eye movement recording. J Neurol Neurosurg Psychiatry 1999;66:532–535. 40. Siderowf AD, Galetta SL, Hurtig HI, Liu GT. Posey, Spiller and progressive supranuclear palsy: an incorrect attribution. Mov Disord 1998;13:170–174. 41. Berger JR, Arendt G. HIV dementia: the role of the basal ganglia and dopaminergic systems. J Psychopharmacol 2000;14:214–221. 42. Mirsattari SM, Power C, Nath A. Parkinsonism with HIV infection. Mov Disord 1998;13:684–689. 43. Wojcieszek J, Lang AE, Jankovic J, Greene P, Deck J. What is it? Case 1, 1994: rapidly progressive aphasia, apraxia, dementia, myoclonus, and parkinsonism. Mov Disord 1994;9:358–366. 44. Amarenco P, Roullet E, Hannoun L, Marteau R. Progressive supranuclear palsy as the sole manifestation of systemic Whipple’s disease treated with pefloxacine. J Neurol Neurosurg Psychiatry 1991;54:1121–1122. 45. Nath U, Ben-Shlomo Y, Thomson RG, et al. The prevalence of progressive supranuclear palsy (Steele–Richardson– Olszewski syndrome) in the UK. Brain 2001;124:1438–1449. 46. Bower JH, Maraganore DM, McDonnell SK, Rocca WA. Incidence of progressive supranuclear palsy and multiple system atrophy in Olmsted County, Minnesota, 1976 to 1990. Neurology 1997;49:1284–1288. 47. Bower JH, Maraganore DM, McDonnell SK, Rocca WA. Incidence and distribution of parkinsonism in Olmsted County, Minnesota, 1976-1990. Neurology 1999;52:1214–1220. 48. Blin J, Baron JC, Dubois B, et al. Positron emission tomography study in progressive supranuclear palsy. Brain hypometabolic pattern and clinicometabolic correlations. Arch Neurol 1990;47:747–752. 49. Lees A. The Steele–Richardson–Olszewski sydrome (progressive supranuclear palsy). In: Marsden CD, Fahn S, eds. Movement Disorders 2. London: Butterworths, 1987;272–287. 50. Golbe LI. Progressive supranuclear palsy. In: Jankovic J, Tolosa E, eds. Parkinson’s Disease and Movement Disorders. Baltimore: Williams & Wilkins, 1993;145–161. 51. Tolosa E, Valldeoriola F, Marti MJ. Clinical diagnosis and diagnostic criteria of progressive supranuclear palsy (Steele– Richardson–Olszewski syndrome). J Neural Transm Suppl 1994;42:15–31. 52. Collins SJ, Ahlskog JE, Parisi JE, Maraganore DM. Progressive supranuclear palsy: neuropathologically based diagnostic clinical criteria. J Neurol Neurosurg Psychiatry 1995;58:167–173. 53. Hughes AJ, Daniel SE, Ben-Shlomo Y, Lees AJ. The accuracy of diagnosis of parkinsonian syndromes in a specialist movement disorder service. Brain 2002;125:861–870. Classification 9 54. Litvan I, Booth V, Wenning GK, et al. Retrospective application of a set of clinical diagnostic criteria for the diagnosis of multiple system atrophy. J Neural Transm 1998;105:217–227. 55. Quinn N. Multiple system atrophy. In: Marsden CD, Fahn S, eds. Movement Disorders 3. London: Butterworths, 1994:262–281. 56. Gilman S, Low PA, Quinn N, et al. Consensus statement on the diagnosis of multiple system atrophy. J Neurol Sci 1999;163:94–98. 57. Mega MS, Masterman DL, Benson DF, et al. Dementia with Lewy bodies: reliability and validity of clinical and pathologic criteria. Neurology 1996;47:1403–1409. 58. Ballard C, Holmes C, McKeith I, et al. Psychiatric morbidity in dementia with Lewy bodies: a prospective clinical and neuropathological comparative study with Alzheimer’s disease. Am J Psychiatry 1999;156:1039–1045. 59. Duara R, Barker W, Luis CA. Frontotemporal dementia and Alzheimer’s disease: differential diagnosis. Dement Geriatr Cogn Disord 1999;10:37–42. 60. Verghese J, Crystal HA, Dickson DW, Lipton RB. Validity of clinical criteria for the diagnosis of dementia with Lewy bodies. Neurology 1999;53:1974–1982. 61. Hohl U, Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J. Diagnostic accuracy of dementia with Lewy bodies. Arch Neurol 2000;57:347–351. 62. Litvan I, MacIntyre A, Goetz CG, et al. Accuracy of the clinical diagnoses of Lewy body disease, Parkinson disease, and dementia with Lewy bodies: a clinicopathologic study. Arch Neurol 1998;55:969–978. 63. Litvan I, Agid Y, Goetz C, et al. Accuracy of the clinical diagnosis of corticobasal degeneration: a clinicopathological study. Neurology 1997;48:119–125. 64. McKeith IG, Ballard CG, Perry RH, et al. Prospective validation of consensus criteria for the diagnosis of dementia with Lewy bodies. Neurology 2005;54:1050–1058.