Illinois State University Long Term Disability Coverage

Illinois State University
Long Term Disability Coverage
Benefit Highlights
LONG TERM DISABILITY PLAN
This long term disability plan provides financial protection for you by paying a portion of your income while you have a long period of disability. The amount you receive is based on the amount you earned before your disability began. In some cases, you can receive disability payments even if you work while you are disabled. Benefits start after the elimination period.
Program Date:
Contract Holder:
Group Contract
Number:
Covered Classes:
June 1, 2010
ILLINOIS STATE UNIVERSITY
G-92821-IL
All active full-time Faculty-Staff members who are participants in the
State Universities Retirement System, eligible for Central Management
Service benefits, and who are employed with an appointment of 50% time or more.
Minimum Hours
Requirement: Employees must be working at least 18.75 hours per week.
Elimination Period: The greater of 90 days or exhaustion of accumulated sick leave and accrued vacation time.
Benefits begin the day after the Elimination Period is completed.
Monthly Benefit: 66 2/3% of your monthly earnings, but not more than the Maximum
Monthly Benefit.
Your benefit may be reduced by deductible sources of income and disability earnings. Some disabilities may not be covered or may be limited under this coverage.
Maximum Monthly
Benefit: $12,000.
Maximum Period of Benefits: Your Age on Your Maximum Benefit
Begins
Under age 61 To your normal retirement age*, but not less than 60 months
Age 61 To your normal retirement age*, but not less than 48 months
Age 62
Age 63
Age 64
Age 65
Age 66
Age 67
Age 68
To your normal retirement age*, but not less than 42 months
To your normal retirement age*, but not less than 36 months
To your normal retirement age*, but not less than 30 months
24 months
21 months
18 months
15 months
Age 69 and over 12 months
*Your normal retirement age is your retirement age under the Social
Security Act where retirement age depends on your year of birth.
No contributions are required for your coverage while you are receiving payments under this plan.
83500
CBH-LTD-1013 (92821-14)
1
Monthly
Catastrophic
Disability Benefit: 20% of your monthly earnings, but not more than $12,000.
Your benefit will not be reduced by deductible sources of income.
Maximum Period
Of Catastrophic
Disability Benefits: Same as Maximum Period of Benefits under the long term disability coverage.
Monthly
Critical Illness
Benefit: 10% of your monthly earnings, but not more than $1,000.
Your benefit will be reduced if it, together with your monthly payment and your monthly catastrophic disability payment, exceeds your monthly earnings. Your benefit will not be reduced by any deductible sources of income.
Maximum Period of Critical Illness
Benefits: Your Age on
Date Critical
Your Maximum Period of Critical Illness Benefits
Under age 61
Age 61
Age 62
Age 63
Age 64
Age 65
Age 66
Age 67
Age 68
Age 69 and over
To your normal retirement age*, but not less than 60 months
To your normal retirement age*, but not less than 48 months
To your normal retirement age*, but not less than 42 months
To your normal retirement age*, but not less than 36 months
To your normal retirement age*, but not less than 30 months
24 months
21 months
18 months
15 months
12 months
*Your normal retirement age is your retirement age under the Social
Security Act where retirement age depends on your year of birth.
Cost of Coverage: The long term disability plan is provided to you on a contributory basis.
You will be informed of the amount of your contribution when you enroll.
The above items are only highlights of your coverage. For a full description please read this entire Group Insurance Certificate.
IMPORTANT INFORMATION FOR RESIDENTS OF CERTAIN STATES:
There are state-specific requirements that may change the provisions under the coverage(s) described in this Group Insurance Certificate. If you live in a state that has such requirements, those requirements will apply to your coverage(s) and are made a part of your Group Insurance
Certificate. Prudential has a website that describes these state-specific requirements. You may access the website at www.prudential.com/etonline. When you access the website, you will be asked to enter your state of residence and your Access Code. Your Access Code is 92821.
If you are unable to access this website, want to receive a printed copy of these requirements or have any questions, call Prudential at 1-866-439-9026.
83500
CBH-LTD-1013 (92821-14)
2
Table of Contents
BENEFIT HIGHLIGHTS - LONG TERM DISABILITY PLAN ................................................................ 1
CERTIFICATE OF COVERAGE ............................................................................................................ 4
GENERAL PROVISIONS ....................................................................................................................... 5
LONG TERM DISABILITY COVERAGE - GENERAL INFORMATION ................................................ 9
LONG TERM DISABILITY COVERAGE - BENEFIT INFORMATION ................................................ 10
LONG TERM DISABILITY - CATASTROPHIC DISABILITY BENEFIT ............................................. 21
LONG TERM DISABILITY COVERAGE - CRITICAL ILLNESS BENEFIT ........................................ 23
LONG TERM DISABILITY - OTHER BENEFITS ................................................................................ 29
LONG TERM DISABILITY COVERAGE – OTHER SERVICES ......................................................... 31
LONG TERM DISABILITY COVERAGE – REHABILITATION SERVICES ....................................... 32
LONG TERM DISABILITY COVERAGE - CLAIM INFORMATION .................................................... 33
GLOSSARY .......................................................................................................................................... 36
83500
CTC-1001 (92821-14)
3
The Prudential Insurance Company of America
Certificate of Coverage
The Prudential Insurance Company of America (referred to as Prudential) welcomes you to the plan.
This is your Certificate of Coverage as long as you are eligible for coverage and you meet the requirements for becoming insured. You will want to read this certificate and keep it in a safe place.
Prudential has written this certificate in booklet format to be understandable to you. If you should have any questions about the content or provisions, please consult Prudential’s claims paying office. Prudential will assist you in any way to help you understand your benefits.
The benefits described in this Certificate of Coverage are subject in every way to the entire
Group Contract which includes this Group Insurance Certificate.
Prudential’s Address
The Prudential Insurance Company of America
751 Broad Street
Newark, New Jersey 07102
83500
CERT-1001 (S-3)
4
General Provisions
What Is the Certificate?
This certificate is a written document prepared by Prudential which tells you:
• the coverage to which you may be entitled;
• to whom Prudential will make a payment; and
• the limitations, exclusions and requirements that apply within a plan.
General Definitions used throughout this certificate include:
You means a person who is eligible for Prudential coverage.
We, us, and our means The Prudential Insurance Company of America.
Employee means a person who is in active employment with the Employer for the minimum hours requirement.
Insured means any person covered under a coverage.
Plan means a line of coverage under the Group Contract.
When Are You Eligible for Coverage?
If you are working for your Employer in a covered class, the date you are eligible for coverage is the plan’s program date:
When Does Your Coverage Begin?
When you pay the cost of your coverage under a plan, you will be covered at 12:01 a.m. on the latest of:
• the first of the month following the date you apply for insurance, if you apply within 60 days after your eligibility date; or
• the date Prudential approves your application, if evidence of insurability is required.
83500
CGP-1001 (92821-14)
5
Evidence of insurability is required if you:
• are a late applicant, which means you apply for coverage more than 60 days after the date you are eligible for coverage; or
• voluntarily canceled your coverage and are reapplying; or
• apply after any of your coverage ended because you did not pay a required contribution; or
• have not met a previous evidence requirement to become insured under any plan the
Employer has with Prudential.
An evidence of insurability form can be obtained from your Employer.
Active employment means you are working for your Employer for earnings that are paid regularly and that you are performing the material and substantial duties of your regular occupation. You must be working at least 18.75 hours per week.
Your worksite must be:
• your Employer’s usual place of business;
• an alternate work site at the direction of your Employer other than your home unless clear specific expectations and duties are documented; or
• a location to which your job requires you to travel.
Normal vacation is considered active employment.
Temporary and seasonal workers are excluded from coverage.
Individuals whose employment status is being continued under a severance or termination agreement will not be considered in active employment.
Evidence of insurability means a statement of your medical history which Prudential will use to determine if you are approved for coverage. Evidence of insurability will be provided at your own expense.
What If You Are Absent from Work on the Date Your Coverage Would Normally
Begin?
If you are absent from work due to injury, sickness, temporary layoff or leave of absence your coverage will begin on the date you return to active employment.
Once Your Coverage Begins, What Happens If You Are Temporarily Not
Working?
If you are on a temporary layoff , and if premium is paid, you will be covered to the end of the month following 12 months in which your temporary layoff begins.
If you are on a leave of absence , and if premium is paid, you will be covered to the end of the month following 12 months in which your leave of absence begins.
83500
CGP-1001 (92821-14)
6
With respect to leave under the federal Family and Medical Leave Act of 1993 (FMLA) or similar state law, continuation of coverage under the plan during such leave will be governed by your
Employer’s policies regarding continuation of such coverage for non-FMLA leave purposes and any applicable law. Continuation of such coverage pursuant to this provision is contingent upon
Prudential’s timely receipt of premium payments and written confirmation of your FMLA leave by your Employer.
If you are working less than 18.75 hours per week, for reasons other than disability, and if premium is paid, you will be covered to the end of the month following the month in which your reduced hours begin.
Layoff or leave of absence means you are temporarily absent from active employment for a period of time that has been agreed to in advance in writing by your Employer, other than for reasons in connection with any severance or termination agreement. Your normal vacation time, any period of disability or FMLA leave is not considered a temporary layoff.
When Will Changes to Your Coverage Take Effect?
Once your coverage begins, any increased or additional coverage due to salary or age will occur on the annual renewal date for your plan, if you are in active employment or if you are on a covered layoff or leave of absence. If you are not in active employment due to injury or sickness, any increased or additional coverage will begin on the date you return to active employment. An increase in your long term disability coverage may be subject to a pre-existing condition limitation as described in the plan. Any decrease in coverage will take effect immediately upon the effective date of the change. Neither an increase nor a decrease in coverage will affect a payable claim that occurs prior to the increase or decrease.
Payable claim means a claim for which Prudential is liable under the terms of the Group
Contract.
When Does Your Coverage End?
Your coverage under the Group Contract or a plan ends on the earliest of:
• the date the Group Contract or a plan is canceled;
• the date you are no longer a member of the covered classes;
• the date your covered class is no longer covered;
• the last day of the period for which you made any required contributions;
• the last day you are in active employment except as provided under the temporary absence from work provisions; or
• the date you are no longer in active employment due to a disability that is not covered under the plan.
83500
CGP-1001 (92821-14)
7
Does the Coverage under a Plan Replace or Affect any Workers’ Compensation or
State Disability Insurance?
The coverage under a plan does not replace or affect the requirements for coverage by workers’ compensation or state disability insurance.
Does Your Employer Act as Prudential’s Agent?
For purposes of the Group Contract, your Employer acts on its own behalf. Under no circumstances will your Employer be deemed the agent of Prudential.
Does This Certificate Address Any Rights to Other Benefits or Affect Your
Employment with Your Employer?
This certificate sets forth only the terms and conditions for coverage and receipt of benefits for
Long Term Disability. It does not address and does not confer any rights, or take away any rights, if any, to other benefits or employment with your Employer. Your rights, if any, to other benefits or employment are solely determined by your Employer. Prudential plays no role in determining, interpreting, or applying any such rights that may or may not exist.
How Can Statements Made in Your Application for this Coverage be Used?
Prudential considers any statements you or your Employer make in a signed application for coverage a representation and not a warranty. If any of the statements you or your Employer make are not complete and/or not true at the time they are made, we can:
• reduce or deny any claim; or
• cancel your coverage from the original effective date.
If a statement is used in a contest, a copy of that statement will be furnished to you or, in the event of your death or incapacity, to your eligible survivor or personal representative.
A statement will not be contested after the amount of insurance has been in force, before the contest, for at least two years during your lifetime.
We will use only statements made in a signed application as a basis for doing this.
If the Employer gives us information about you that is incorrect, we will:
• use the facts to decide whether you have coverage under the plan and in what amounts; and
• make a fair adjustment of the premium.
83500
CGP-1001 (92821-14)
8
Long Term Disability Coverage
General Information
Who Is in the Covered Class(es) for the Insurance?
The Covered Classes are:
All active full-time Faculty-Staff members who are participants in the State
Universities Retirement System, eligible for Central Management
Services benefits, and who are employed with an appointment of 50% time or more.
How Many Hours Must You Work to be Eligible for Coverage?
You must be working at least 18.75 hours per week.
Who Pays for Your Coverage?
Your coverage is paid for by you. Your Employer will inform you of the amount of your contribution when you enroll.
83500
9
Long Term Disability Coverage
BENEFIT INFORMATION
How Does Prudential Define Disability?
You are disabled when Prudential determines that:
• you are unable to perform the material and substantial duties of your regular occupation due to your sickness or injury ; and
• you have a 20% or more loss in your indexed monthly earnings due to that sickness or injury .
After 60 months of payments, you are disabled when Prudential determines that due to the same sickness or injury, you are unable to perform the duties of any gainful occupation for which you are reasonably fitted by education, training or experience.
The loss of a professional or occupational license or certification does not, in itself, constitute disability.
We may require you to be examined by doctors, other medical practitioners or vocational experts of our choice. Prudential will pay for these examinations. We can require examinations as often as it is reasonable to do so. We may also require you to be interviewed by an authorized Prudential Representative. Refusal to be examined or interviewed may result in denial or termination of your claim.
Material and substantial duties means duties that:
• are normally required for the performance of your regular occupation; and
• cannot be reasonably omitted or modified.
Regular occupation means the occupation you are routinely performing when your disability begins. Prudential will look at your occupation as it is normally performed instead of how the work tasks are performed for a specific employer or at a specific location.
Gainful occupation means an occupation, including self employment, that is or can be expected to provide you with an income equal to at least 66 2/3% of your indexed monthly earnings within 12 months of your return to work.
Sickness means any disorder of your body or mind, but not an injury; pregnancy including abortion, miscarriage or childbirth. Disability must begin while you are covered under the plan.
Injury means a bodily injury that is the direct result of an accident, is independent of sickness, and occurs while you are covered under the plan. Injury which occurs before you are covered under the plan will be treated as a sickness. Disability must begin while you are covered under the plan.
GRP 99645-14
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
10
Indexed monthly earnings means your monthly earnings as adjusted on each July 1 provided you were disabled for all of the 12 months before that date. Your monthly earnings will be adjusted on that date by the lesser of 10% or the current annual percentage increase in the Consumer Price Index. Your indexed monthly earnings may increase or remain the same, but will never decrease.
The Consumer Price Index (CPI-W) is published by the U.S. Department of Labor. Prudential reserves the right to use some other similar measurement if the Department of Labor changes or stops publishing the CPI-W.
Indexing is only used to determine your percentage of lost earnings while you are disabled and working.
How Long Must You Be Disabled Before Your Benefits Begin?
You must be continuously disabled through your elimination period . Prudential will treat your disability as continuous if your disability stops for 30 days or less during the elimination period. The days that you are not disabled will not count toward your elimination period.
Your elimination period is the greater of 90 days or exhaustion of accumulated sick leave and accrued vacation time.
Elimination period means a period of continuous disability which must be satisfied before you are eligible to receive benefits from Prudential.
Can You Satisfy Your Elimination Period If You Are Working?
Yes, provided you meet the definition of disability.
When Will You Begin to Receive Disability Payments?
You will begin to receive payments when we approve your claim, providing the elimination period has been met. We will send you a payment each month for any period for which
Prudential is liable.
How Much Will Prudential Pay If You Are Disabled and Not Working?
We will follow this process to figure out your monthly payment :
1. Multiply your monthly earnings by 66 2/3%. maximum is $12,000.
3. Compare the answer in item 1 with the maximum monthly benefit. The lesser of these two amounts is your gross disability payment .
4. Subtract from your gross disability payment any deductible sources of income .
That amount figured in item 4 is your monthly payment.
After the elimination period, if you are disabled for less than 1 month, we will send you 1/30th of your payment for each day of disability.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
11
Monthly payment means your payment after any deductible sources of income have been subtracted from your gross disability payment.
Monthly benefit means the total benefit amount for which you are insured under this plan subject to the maximum benefit.
Gross disability payment means the benefit amount before Prudential subtracts deductible sources of income and disability earnings.
Deductible sources of income means income from deductible sources listed in the plan that you receive or are entitled to receive while you are disabled. This income will be subtracted from your gross disability payment.
What Are Your Monthly Earnings?
Monthly earnings means the greater of: a) your average gross monthly income from your
Employer as reported on your W-2 form for the year prior to your date of disability; it will not be reduced by deductions made for any pre-tax contributions; and b) your average monthly
SURS salary from your Employer earned during the previous two years, as reported to
Prudential by the Employer.
If you did not receive a W-2 form from your Employer for the year prior to your date of disability, monthly earnings means your average gross monthly income from your Employer during your period of employment, as reported to Prudential by the Employer.
How Much Will Prudential Pay If You Work While You Are Disabled?
We will send you the monthly payment if you are disabled and your monthly disability earnings , if any, are less than 20% of your indexed monthly earnings due to the same sickness or injury.
If you are disabled and your monthly disability earnings are 20% or more of your indexed monthly earnings, due to the same sickness or injury, Prudential will figure your payment as follows:
During the first 12 months of payments, while working, your monthly payment will not be reduced as long as disability earnings plus the gross disability payment does not exceed
100% of indexed monthly earnings.
1. Add your monthly disability earnings to your gross disability payment.
2. Compare the answer in item 1 to your indexed monthly earnings.
If the answer from item 1 is less than or equal to 100% of your indexed monthly earnings,
Prudential will not further reduce your monthly payment.
If the answer from item 1 is more than 100% of your indexed monthly earnings, Prudential will subtract the amount over 100% from your monthly payment.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
12
After 12 months of payments, while working, you will receive payments based on the percentage of income you are losing due to your disability.
1. Subtract your disability earnings from your indexed monthly earnings.
2. Divide the answer in item 1 by your indexed monthly earnings. This is your percentage of lost earnings.
3. Multiply your monthly payment by the answer in item 2.
This is the amount Prudential will pay you each month.
During the first 60 months of disability payments, if your monthly disability earnings exceed
80% of your indexed monthly earnings, Prudential will stop sending you payments and your claim will end.
Beyond 60 months of disability payments, if your monthly disability earnings exceed 60% of your indexed monthly earnings, Prudential will stop sending you payments and your claim will end.
Prudential may require you to send proof of your monthly disability earnings on a monthly basis. We will adjust your payment based on your monthly disability earnings.
As part of your proof of disability earnings, we can require that you send us appropriate financial records, including copies of your IRS federal income tax return, W-2’s and 1099’s, which we believe are necessary to substantiate your income.
Disability earnings means the earnings which you receive while you are disabled and working, plus the earnings you could receive if you were working to your greatest extent possible. This would be, based on your restrictions and limitations:
•
During the first 60 months of disability payments, the greatest extent of work you are able to do in your regular occupation, that is reasonably available.
•
Beyond 60 months of disability payments, the greatest extent of work you are able to do in any occupation, that is reasonably available, for which you are reasonably fitted by education, training or experience.
Salary continuance paid to supplement your disability earnings will not be considered payment for work performed.
What Happens If Your Disability Earnings Fluctuate?
If your disability earnings are expected to fluctuate widely from month to month, Prudential may average your disability earnings over the most recent 3 months to determine if your claim should continue subject to all other terms and conditions in the plan.
If Prudential averages your disability earnings, we will terminate your claim if:
•
During the first 60 months of disability payments, the average of your disability earnings from the last 3 months exceeds 80% of indexed monthly earnings; or
•
Beyond 60 months of disability payments, the average of your disability earnings from the last 3 months exceeds 60% of indexed monthly earnings.
We will not pay you for any month during which disability earnings exceed the above amounts.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
13
What Are Deductible Sources of Income?
Prudential will deduct from your gross disability payment the following deductible sources of income:
1. The amount that you receive or are entitled to receive as loss of time benefits under:
(a) a workers’ compensation law;
(b) an occupational disease law; or
(c) any other act or law with similar intent.
2. The amount that you receive or are entitled to receive as loss of time disability income payments under any:
(a) state compulsory benefit act or law;
(b) automobile liability insurance policy;
(c) other group insurance plan; or
(d) governmental retirement system as the result of your job with your Employer; or
(e) the State Universities Retirement System benefit.
3. The amount that you, your spouse and children receive or are entitled to receive as loss of time disability payments because of your disability under:
(a) the United States Social Security Act;
(b) the Railroad Retirement Act;
(c) the Canada Pension Plan;
(d) the Quebec Pension Plan; or
(e) any similar plan or act .
Amounts paid to your former spouse or to your children living with such spouse will not be included.
4. The amount that you receive as retirement payments or the amount your spouse and children receive as retirement payments because you are receiving payments under:
(a) the United States Social Security Act;
(b) the Railroad Retirement Act;
(c) the Canada Pension Plan;
(d) the Quebec Pension Plan; or
(e) any similar plan or act.
Benefits paid to your former spouse or to your children living with such spouse will not be included.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
14
5. The amount that you:
(a) receive as disability payments under your Employer’s retirement plan ;
(b) voluntarily elect to receive as retirement or early retirement payments under your
Employer’s retirement plan; or
(c) receive as retirement payments when you reach normal retirement age, as defined in your Employer’s retirement plan.
Disability payments under a retirement plan will be those benefits which are paid due to disability and do not reduce the retirement benefits which would have been paid if the disability had not occurred.
Retirement payments will be those benefits which are paid based on your Employer’s contribution to the retirement plan. Disability benefits which reduce the retirement benefits under the plan will also be considered as a retirement benefit.
Amounts received do not include amounts rolled over or transferred to any eligible retirement plan. Prudential will use the definition of eligible retirement plan as defined in
Section 402 of the Internal Revenue Code including any future amendments which affect the definition.
6. The amount you receive under the maritime doctrine of maintenance, wages and cure.
This includes only the “wages” part of such benefits.
7. The amount that you receive from a partnership, proprietorship or any similar draws.
With the exception of retirement payments, or amounts that you receive from a partnership, proprietorship or any similar draws, Prudential will only subtract deductible sources of income which are payable as a result of the same disability.
We will not reduce your payment by your Social Security income if your disability begins after age 65 and you were already receiving Social Security retirement payments.
Law, plan or act means the original enactment of the law, plan or act and all amendments.
Retirement plan means a defined contribution plan or defined benefit plan. These are plans which provide retirement benefits to employees and are not funded entirely by employee contributions.
What Are Not Deductible Sources of Income?
Prudential will not deduct from your gross disability payment income you receive from, but not limited to, the following sources:
•
401(k)
•
profit sharing plans;
•
thrift
•
tax sheltered annuities;
•
stock ownership plans;
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
15
•
non-qualified plans of deferred compensation;
•
pension plans for partners;
•
military pension and disability income plans;
•
credit disability insurance;
•
franchise disability income plans;
•
a retirement plan from another Employer;
•
individual retirement accounts (IRA).
What If Subtracting Deductible Sources of Income Results in a Zero Benefit?
(Minimum Benefit)
The minimum monthly payment is $100.00.
Prudential may apply this amount toward an outstanding overpayment.
What Happens When You Receive a Cost of Living Increase from Deductible
Sources of Income?
Once Prudential has subtracted any deductible source of income from your gross disability payment, Prudential will not further reduce your payment due to a cost of living increase from that source.
What If Prudential Determines that You May Qualify for Deductible Income
Benefits?
If we determine that you may qualify for benefits under item 1, 2 or 3 in the deductible sources of income section, we will estimate your entitlement to these benefits. We can reduce your payment by the estimated amount if such benefits have not been awarded.
However, we will NOT reduce your payment by the estimated amount under item 1, 2 or 3 in the deductible sources of income section if you:
•
apply for the benefits;
•
appeal any denial to all administrative levels Prudential feels are necessary; and
•
sign Prudential’s Reimbursement Agreement form. This form states that you promise to pay us any overpayment caused by an award.
If your payment has been reduced by an estimated amount, your payment will be adjusted when we receive proof:
•
of the amount awarded; or
•
that benefits have been denied and all appeals Prudential feels are necessary have been completed. In this case, a lump sum refund of the estimated amount will be made to you.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
16
What Happens If You Receive a Lump Sum Payment?
If you receive a lump sum payment from any deductible source of income, the lump sum will be pro-rated on a monthly basis over the time period for which the sum was given. If no time period is stated, we will use a reasonable one.
How Long Will Prudential Continue to Send You Payments?
Prudential will send you a payment each month up to the maximum period of payment .
Your maximum period of payment is:
Your Age on Date Your Maximum Period
Under age 61
Age 61
Age 62
Age 63
Age 64
Age 65
Age 66
Age 67
To your normal retirement age*, but not less than 60 months
To your normal retirement age*, but not less than 48 months
To your normal retirement age*, but not less than 42 months
To your normal retirement age*, but not less than 36 months
To your normal retirement age*, but not less than 30 months
24 months
21 months
18 months
Age 68
Age 69 and over
15 months
12 months
*Your normal retirement age is your retirement age under the Social Security Act where retirement age depends on your year of birth.
We will stop sending you payments and your claim will end on the earliest of the following:
1. During the first 60 months of payments, when you are able to work in your regular occupation on a part-time basis but you choose not to; after 60 months of payments, when you are able to work in any gainful occupation on a part-time basis but you choose not to.
2. The end of the maximum period of payment.
3. The date you are no longer disabled under the terms of the plan.
4. The date you fail to submit proof of continuing disability satisfactory to Prudential.
5. The date your disability earnings exceed the amount allowable under the plan.
6. The date you die.
Maximum period of payment means the longest period of time Prudential will make payments to you for any one period of disability.
Part-time basis means the ability to work and earn 20% or more of your indexed monthly earnings.
What Disabilities Have a Limited Pay Period Under Your Plan?
Disabilities which, as determined by Prudential, are due in whole or part to mental illness have a limited pay period during your lifetime.
The limited pay period for mental illness is 24 months during your lifetime.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
17
Prudential will continue to send you payments for disabilities due in whole or part to mental illness beyond the 24 month period if you meet one or both of these conditions:
1. If you are confined to a hospital or institution at the end of the 24 month period,
Prudential will continue to send you payments during your confinement .
If you are still disabled when you are discharged, Prudential will send you payments for a recovery period of up to 90 days.
If you become reconfined at any time during the recovery period and remain confined for at least 14 days in a row, Prudential will send payments during that additional confinement and for one additional recovery period up to 90 more days.
2. In addition to item 1, if, after the 24 month period for which you have received payments, you continue to be disabled and subsequently become confined to a hospital or institution for at least 14 days in a row, Prudential will send payments during the length of the confinement.
Prudential will not pay beyond the limited pay period as indicated above, or the maximum period of payment, whichever occurs first.
Prudential will not apply the mental illness limitation to dementia if it is a result of:
•
stroke;
•
trauma;
•
viral
•
Alzheimer’s disease; or
•
other conditions not listed which are not usually treated by a mental health provider or other qualified provider using psychotherapy, psychotropic drugs, or other similar methods of treatment as standardly accepted in the practice of medicine.
Mental illness means a psychiatric or psychological condition regardless of cause. Mental illness includes but is not limited to schizophrenia, depression, manic depressive or bipolar illness, anxiety, somatization, substance related disorders and/or adjustment disorders or other conditions. These conditions are usually treated by a mental health provider or other qualified provider using psychotherapy, psychotropic drugs, or other similar methods of treatment as standardly accepted in the practice of medicine.
Confined or confinement for this section means a hospital stay of at least 8 hours per day.
Hospital or institution means an accredited facility licensed to provide care and treatment for the condition causing your disability.
What Disabilities Are Not Covered Under Your Plan?
Your plan does not cover any disabilities caused by or resulting from your:
•
intentionally self-inflicted injuries;
•
active participation in a riot; or
•
commission of a crime for which you have been convicted under state or federal law.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
18
Your plan does not cover a disability which:
•
begins within 24 months of the date your coverage under the plan becomes effective; and
•
is due to a pre-existing condition.
Your plan does not cover a disability due to war, declared or undeclared, or any act of war.
Prudential will not make a payment for any period of disability during which you are incarcerated as a result of a conviction.
What Is a Pre-Existing Condition?
You have a pre-existing condition if:
1. You received medical treatment, consultation, care or services including diagnostic measures, took prescribed drugs or medicines, or followed treatment recommendation in the 6 months just prior to your effective date of coverage or the date an increase in benefits would otherwise be available; or
2. You had symptoms for which an ordinarily prudent person would have consulted a health care provider in the 6 months just prior to your effective date of coverage or the date an increase in benefits would otherwise be available.
But, a condition will no longer be considered a pre-existing condition if, after the date your coverage under the plan becomes effective, there is a period of 6 months or more during which you do not:
• receive medical treatment, consultation, care or services, including diagnostic measures, take prescribed drugs or medicines of follow treatment recommendation for that condition; and
• have symptoms related to that condition for which an ordinarily prudent person would have consulted a health care provider; or
• you remain actively insured in the plan for 24 consecutive months.
How Does a Pre-Existing Condition Affect an Increase in Your Benefits?
If there is an increase in your benefits due to an amendment of the plan; or your enrollment in another plan option, a benefit limit will apply if your disability is due to a pre-existing condition.
You will be limited to the benefits you had on the day before the increase if your disability begins during the 24 month period starting with the date the increase in benefits would have been effective. The increase will not take effect until your disability ends.
How Does the Pre-Existing Condition Work If You Were Covered Under Your
Employer’s Prior Plan?
Special rules apply to pre-existing conditions, if this long term disability plan replaces your
Employer’s prior plan and:
• you were covered by that plan on the day before this plan became effective; and
• you became covered under this plan within thirty-one days of its effective date.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
19
The special rules are:
1. If the Employer’s prior plan did not have a pre-existing condition exclusion or limitation, then a pre-existing condition will not be excluded or limited under this plan.
2. If the Employer’s prior plan did have a pre-existing condition exclusion or limitation, then the limited time does not end after the first 24 months of coverage. Instead it will end on the date any equivalent limit would have ended under the Employer’s prior plan.
3. If the change from your Employer’s prior plan to this plan of coverage would result in an increase in your amount of benefits, the benefits for your disability that is due to a preexisting sickness or injury will not increase. Instead the benefits are limited to the amount you had on the day before the plan change.
GRP 99545-7
What Happens If You Return to Work Full Time and Your Disability Occurs
Again?
If you have a recurrent disability , as determined by Prudential, we will treat your disability as part of your prior claim and you will not have to complete another elimination period if:
•
you were continuously insured under this plan for the period between your prior claim and your current disability; and
•
your recurrent disability occurs within 6 months of the end of your prior claim.
Your recurrent disability will be subject to the same terms of the plan as your prior claim. Any disability which occurs after 6 months from the date your prior claim ended will be treated as a new claim. The new claim will be subject to all of the plan provisions.
If you become covered under any other group long term disability plan, you will not be eligible for payments under the Prudential plan.
Recurrent disability means a disability which is:
•
caused by a worsening in your condition; and
•
due to the same cause(s) as your prior disability for which Prudential made a Long Term
Disability payment.
83500
CBI-LTD-1057 (as modified by GRP 99645-14 and GRP 99545-7) (92821-14)
20
Long Term Disability Coverage
CATASTROPHIC DISABILITY BENEFIT
How Does Prudential Define Catastrophic Disability?
You are catastrophically disabled when Prudential determines that, due to the same sickness or injury that caused your disability, you:
• are unable to perform, without substantial assistance , at least two activities of daily living ; or
• have a severe cognitive impairment , which requires substantial supervision to protect you from threats to health and safety.
Substantial assistance means:
• the physical assistance of another person without which you would not be able to perform an activity of daily living; or
• the constant presence of another person within arm’s reach which is necessary to prevent, by physical intervention, injury to you while you are performing an activity of daily living.
Activities of daily living means:
•
Bathing - washing oneself by sponge bath, or in either a tub or shower, including the task of getting into or out of the tub or shower;
•
Continence - the ability to maintain control of bowel and bladder function; or, when unable to maintain control of bowel and bladder function, the ability to perform associated personal hygiene (including caring for catheter or colostomy bag);
•
Dressing - putting on and taking off all items of clothing and any necessary braces, fasteners or artificial limbs;
•
Eating - feeding oneself by getting food into the body from a receptacle (such as a plate, cup or table) or by feeding tube or intravenously;
•
Toileting - getting to and from the toilet, getting on and off the toilet, and performing associated personal hygiene;
•
Transferring - sufficient mobility to move into or out of a bed, chair or wheelchair or to move from place to place, either by walking, using a wheelchair or by other means.
Cognitive impairment means a loss or deterioration in intellectual capacity that is:
• comparable to and includes Alzheimer’s disease and similar forms of irreversible dementia; and
83500
CDB-LTD-1002 (92821-14)
21
• measured by clinical evidence and standardized tests that reliably measure impairment in the individual’s short-term or long-term memory, orientation as to person, place or time; and deductive or abstract reasoning.
Substantial supervision means continual oversight that may include cueing by verbal prompting, gestures, or other demonstrations by another person, and which is necessary to protect you from threats to your health or safety.
When Will You Begin to Receive Payments for Your Catastrophic Disability?
You will begin to receive catastrophic disability payments when we approve your claim, providing:
• you are receiving long term disability benefits under the plan; and
• you have had your catastrophic disability for a period of at least 30 consecutive days.
How Much Will Prudential Pay When You Have a Catastrophic Disability?
Your monthly catastrophic disability payment is equal to 20% of your monthly earnings, but not more than $12,000. It will not be reduced by any deductible sources of income.
How Long Will Prudential Continue to Send You Catastrophic Disability
Payments?
Prudential will send you a catastrophic disability payment each month up to the maximum period of catastrophic disability payment .
We will stop sending you payments and your catastrophic disability claim will end on the earliest of the following:
1. The date you no longer have a catastrophic disability under the terms of the plan.
2. The date you fail to submit proof of continuing catastrophic disability satisfactory to
Prudential.
3. The date you are no longer receiving long term disability benefits under the plan.
83500
CDB-LTD-1002 (92821-14)
22
Long Term Disability Coverage
CRITICAL ILLNESS BENEFIT
What Benefits Will be Provided If You Have a Critical Illness?
Prudential will pay a critical illness benefit to you when we determine that, due to the same sickness or injury that caused your disability: you have a covered critical illness ; and you are under the regular care of a doctor .
We may require you to be examined by doctors or other medical practitioners of our choice.
Prudential will pay for these examinations. We can require examinations as often as it is reasonable to do so. We may also require you to be interviewed by an authorized Prudential
Representative. Refusal to be examined or interviewed may result in denial or termination of your claim.
Covered critical illness means heart attack, life-threatening cancer, major organ or tissue transplant, renal failure or stroke.
Heart attack means the infarction (death) of a portion of heart muscle, as a result of inadequate blood supply due to obstruction in one or more coronary arteries. To be a covered critical illness, a new occurrence of heart attack (or myocardial infarction) must be demonstrated by the following: electrocardiographic changes consistent with and supporting a diagnosis of new heart attack
(myocardial infarction); a concurrent diagnostic elevation of cardiac enzymes; and imaging studies such as thallium scans, MUGA scans or stress echocardiograms.
Heart attack does not mean: congestive heart failure, atherosclerotic heart disease, angina, or coronary artery disease; or other dysfunction of the cardiovascular system.
Life-threatening cancer means a malignant neoplasm which is: characterized by uncontrolled growth and spread of malignant cells and the invasion of tissue; and is not specifically excluded below.
The term can include leukemia or lymphoma which has been diagnosed as life-threatening.
83500
CIB-LTD-1007 (92821-14)
23
The diagnosis of a life-threatening cancer must be: made by a doctor; based on pathological evidence; and supported by a clinical evaluation.
A pathological diagnosis of cancer is based on microscopic study of fixed tissue or preparations from the hemic (blood) system. This type of diagnosis must be confirmed by a certified pathologist, whose diagnosis of malignancy is in keeping with the standards set up by the
American Board of Pathology.
Life-threatening cancer does not include: early prostate cancer diagnosed as T1N0M0 or equivalent staging. carcinoma in situ. This is a diagnosis of cancer where the tumor cells: lie within the tissue of the site of origin; have not invaded neighboring tissue; and are diagnosed as stage TisN0M0. all stages of basal cell carcinoma and squamous cell carcinoma. stage 1 T1N0M0 melanoma with a Breslow thickness less than 1.0 mm. This exclusion does not apply to invasive or metastatic malignant melanoma. stage 1 Hodgkin’s Lymphoma. conditions with the potential to become malignant, pre-malignant lesions, benign tumors or polyps.
Major organ or tissue transplant means end stage major organ or tissue failure that requires your malfunctioning organ or tissue to be replaced with that of a suitable donor by generally accepted medical procedures. Transplanted organs or tissue covered by this definition are limited to liver, kidney, lung, heart, small intestine, pancreas and bone marrow tissue.
For a major organ or tissue transplant to be a covered critical illness under this benefit, you must also be registered in an organ registry as a potential recipient.
Renal (kidney) failure (or “end stage renal disease”) means chronic and irreversible failure of both kidneys, which requires weekly or more frequent dialysis treatment. To be a covered critical illness under this benefit, the diagnosis of renal failure must be: made by a doctor who is a board certified nephrologist; and supported by objective testing and treatment.
Stroke means a cerebrovascular accident resulting in permanent neurological impairment from infarction (death) of brain tissue as a result of cerebral hemorrhage, embolism or thrombosis that results in: significant impairment in cognition or mobility;
83500
CIB-LTD-1007 (92821-14)
24
complete or partial loss of function involving motion or sensation of part of the body; and measurable and documented permanent neurological deficits.
The diagnosis of stroke must be confirmed by neuroimaging studies such as CAT scan or MRI.
Stroke does not include head injury, transient ischemic attack (TIA) or other cerebrovascular insufficiency.
Regular care means: you personally visit a doctor as frequently as is medically required, according to generally accepted medical standards, to effectively manage and treat your critical illness; and you are receiving the most appropriate treatment and care, which conforms with generally accepted medical standards, for your critical illness by a doctor whose specialty or experience is the most appropriate for your critical illness, according to generally accepted medical standards.
Doctor means: person who is performing tasks that are within the limits of his or her medical license; and is licensed to practice medicine and prescribe and administer drugs or to perform surgery; or has a doctoral degree in Psychology (Ph.D. or Psy.D.) whose primary practice is treating patients; or is a legally qualified medical practitioner according to the laws and regulations of the governing jurisdiction.
Prudential will not recognize any relative including, but not limited to, you, your spouse, or a child, brother, sister, or parent of you or your spouse as a doctor for a claim that you send to us.
How Long Must You Have a Critical Illness Before Your Benefits Begin?
You must have a critical illness through your critical illness elimination period .
Your elimination period is the greater of 90 days or exhaustion of accumulated sick leave and accrued vacation time.
Critical Illness elimination period means a period of consecutive days which you have survived and which must be satisfied before you are eligible to receive benefits from Prudential.
Your critical illness elimination period begins on the date your covered critical illness begins.
Can You Satisfy Your Critical Illness Elimination Period If You Are Working?
Yes, provided you meet the definition of critical illness.
When Will You Begin to Receive Critical Illness Payments?
You will begin to receive critical illness payments when we approve your claim, providing: the critical illness elimination period has been met, and you are receiving long term disability benefits under the plan.
We will send you a payment each month for any period for which Prudential is liable.
83500
CIB-LTD-1007 (92821-14)
25
How Much Will Prudential Pay When You Have a Critical Illness?
Your monthly critical illness payment is equal to 10% of your monthly earnings , but not more than $1,000. Your monthly critical illness payment, together with your monthly long term disability payment and your monthly catastrophic disability payment, will not exceed your monthly earnings. Your monthly critical illness payment will not be reduced by any deductible sources of income.
Monthly earnings means the greater of: a) your average gross monthly income from your
Employer as reported on your W-2 form for the year prior to your date of disability; it will not be reduced by deductions made for any pre-tax contributions; and b) your average monthly SURS salary from your Employer earned during the previous two years, as reported to Prudential by the Employer.
If you did not receive a W-2 form from your Employer for the year prior to your date of disability, monthly earnings means your average gross monthly income from your Employer during your period of employment, as reported to Prudential by the Employer.
How Long Will Prudential Continue to Send You Critical Illness Payments?
Prudential will send you a critical illness payment each month up to the maximum period of critical illness payment .
Your maximum period of critical illness payment is:
Your Age on Date
Critical Illness
Begins
Your Maximum Period of Critical Illness Benefits
Under age 61
Age 61
Age 62
Age 63
Age 64
Age 65
Age 66
Age 67
Age 68
Age 69 and over
To your normal retirement age*, but not less than 60 months
To your normal retirement age*, but not less than 48 months
To your normal retirement age*, but not less than 42 months
To your normal retirement age*, but not less than 36 months
To your normal retirement age*, but not less than 30 months
24 months
21 months
18 months
15 months
12 months
*Your normal retirement age is your retirement age under the Social Security Act where retirement age depends on your year of birth.
We will stop sending you payments while you are incarcerated as a result of a conviction.
We will stop sending you payments and your critical illness claim will end on the earliest of the following:
1. The end of the maximum period of critical illness payment.
2. The date you are no longer have a critical illness under the terms of the plan.
3. The date you fail to submit proof of continuing critical illness satisfactory to Prudential.
83500
CIB-LTD-1007 (92821-14)
26
4. The date you die.
5. The date you are no longer receiving long term disability benefits under the plan.
Maximum period of critical illness payment means the longest period of time Prudential will make critical illness payments to you for your critical illness.
What Critical Illnesses Have a Limited Pay Period Under Your Plan?
Critical illness which, as determined by Prudential, is due to heart attack has a limited pay period during your lifetime.
The limited pay period for heart attack is 12 months during your lifetime.
When Is This Critical Illness Benefit Not Payable?
This benefit is not payable for more than one period of critical illness during your lifetime, regardless of the number of times you have a critical illness.
This benefit is not payable for a critical illness due to a pre-existing condition.
This benefit is not payable for your critical illness which begins after you begin receiving long term disability benefits under the plan, unless your critical illness begins within 24 months of the date you meet the elimination period for your disability.
This benefit is not payable for a critical illness which begins after the date you attain age 65.
What Is a Pre-Existing Condition?
You have a pre-existing condition if both 1. and 2. are true:
1. (a) You received medical treatment, consultation, care or services, including diagnostic measures, or took prescribed drugs or medicines, or followed treatment recommendation in the 6 months just prior to the date your coverage for this benefit began or the date an increase in critical illness benefits would otherwise be available; or
(b) you had symptoms for which an ordinarily prudent person would have consulted a health care provider in the 6 months just prior to the date your coverage for this benefit began or the date an increase in critical illness benefits would otherwise be available.
2. Your critical illness begins within 24 months of the date your coverage for this benefit begins.
But you do not have a pre-existing condition if, after the date your coverage for this benefit begins, there is a period of 6 months or more during which you do not: receive medical treatment, consultation, care or services, including diagnostic measures, take prescribed drugs or medicines, or follow treatment recommendation for that condition; and have symptoms related to that condition for which an ordinarily prudent person would have consulted a health care provider.
83500
CIB-LTD-1007 (92821-14)
27
How Does a Pre-Existing Condition Affect an Increase in Your Critical Illness
Benefits?
If there is an increase in your critical illness benefits due to an amendment of the plan; or your enrollment in another plan option, a benefit limit will apply if your critical illness is due to a preexisting condition.
You will be limited to the critical illness benefits you had on the day before the increase.
How Do You File a Critical Illness Claim?
The claim rules that apply to your Long Term Disability coverage also apply to this Critical Illness
Benefit. See the Claim Information page for details.
83500
CIB-LTD-1007 (92821-14)
28
Long Term Disability Coverage
OTHER BENEFIT FEATURES
What Benefits Will be Provided to Your Family If You Die?
(Survivor Benefit)
When Prudential receives proof that you have died, we will pay your eligible survivor a lump sum benefit equal to 6 months of your gross disability payment if, on the date of your death:
• your disability had continued for 180 or more consecutive days; and
• you were receiving or were entitled to receive payments under the plan.
If you have no eligible survivors, payment will be made to your estate.
However, we will first apply the survivor benefit to any overpayment which may exist on your claim.
Eligible survivor means your spouse, if living; otherwise, your children under age 25.
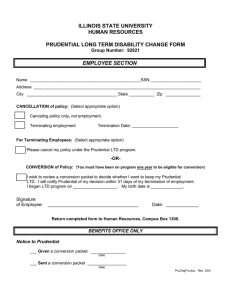
What Insurance Is Available If You End Employment?
(Conversion)
If you end employment with your Employer, your coverage under the plan will end. You may be eligible to purchase insurance under Prudential’s group conversion policy. To be eligible, you must have been insured under your Employer’s group plan for at least 12 consecutive months.
We will consider the amount of time you were insured under the Prudential plan and the plan it replaced, if any.
You are not eligible to apply for coverage under Prudential’s group conversion policy if:
• you are or become insured under another group long term disability plan within 31 days after your employment ends;
• you are disabled under the terms of the plan;
• you are age 70 or more when your employment ends;
• your coverage under the plan ends for any of the following reasons:
-- the plan is canceled;
-- the plan is changed to exclude the group of employees to which you belong;
-- you are no longer in an eligible group;
-- you retire;
83500
COTB-LTD-1001 (S-10)(92821-14)
29
-- you fail to pay the required premium under this plan.
You must apply for insurance under the conversion policy and pay the first premium to
Prudential within 60 days after the date your employment ends. Evidence of insurability will be required for certain higher amounts of monthly payments.
Prudential will determine the coverage you will have under the conversion policy. The conversion policy may not be the same coverage we offered you under your Employer’s group plan. It may be any form of conversion plan that we then make available. The benefits will comply with any state laws or regulations that may apply.
Your amount of coverage under the conversion plan will not be more than your amount under this plan when your coverage ends. It may be lower than under this plan.
Your rates for the conversion plan will be based on Prudential’s rate as it applies to the form and amount of insurance it provides, the premium period and your age at the time of conversion.
Your premiums will not be due less often than quarterly, unless you agree to another frequency.
83500
COTB-LTD-1001 (S-10)(92821-14)
30
Long Term Disability Coverage
OTHER SERVICES
How Can Prudential Help Your Employer Identify and Provide Worksite
Modification?
A worksite modification might be what is needed to allow you to perform the material and substantial duties of your regular occupation with your Employer. One of our designated professionals will assist you and your Employer to identify a modification we agree is likely to help you remain at work or return to work. This agreement will be in writing and must be signed by you, your Employer and Prudential.
When this occurs, Prudential will reimburse your Employer for the cost of the modification up to the greater of:
•
$1,000;
• the equivalent of two months of your gross disability payment.
This benefit is available to you on a one time only basis.
How Can Prudential’s Social Security Claimant Assistance Program Help You
With Obtaining Social Security Disability Benefits?
Prudential can arrange for expert advice regarding your Social Security disability benefits claim and assist you with your application or appeal, if you are disabled under the plan.
Receiving Social Security disability benefits may enable:
• you to receive Medicare after 24 months of disability payments;
• you to protect your retirement benefits; and
• your family to be eligible for Social Security benefits.
We can assist you in obtaining Social Security disability benefits by:
• helping you find appropriate legal representation;
• obtaining medical and vocational evidence; and
• reimbursing pre-approved case management expenses.
83500
COTS-LTD-1010 (92821-14)
31
Long Term Disability Coverage
REHABILITATION SERVICES
How Can Prudential’s Rehabilitation Program Help You Return to Work?
Prudential has a rehabilitation program available.
As your file is reviewed, medical and vocational information will be analyzed to determine if rehabilitation services might help you return to work.
Once the initial review is completed by our rehabilitation program specialists working along with your doctor and other appropriate specialists, Prudential may elect to offer you and pay for a rehabilitation program. If the rehabilitation program is not developed by Prudential’s rehabilitation program specialists, you must receive written approval from Prudential for the program before it begins.
The rehabilitation program may include, but is not limited to, the following services:
• coordination with your Employer to assist you to return to work;
• evaluation of adaptive equipment to allow you to work;
• vocational evaluation to determine how your disability may impact your employment options;
• job placement services;
•
resume
• job seeking skills training;
• retraining for a new occupation; or
• assistance with relocation that may be part of an approved rehabilitation program.
Rehabilitation program means a program designed to assist you to return to work.
83500
CRS-LTD-1001 (92821-14)
32
Long Term Disability Coverage
CLAIM INFORMATION
When Do You Notify Prudential of a Claim?
We encourage you to notify us of your claim as soon as possible, so that a claim decision can be made in a timely manner. Written notice of a claim should be sent within 30 days after the date your disability or critical illness begins. However, you must send Prudential written proof of your claim no later than 90 days after your elimination period or critical illness elimination period ends.
If it is not possible to give proof within 90 days, it must be given no later than 1 year after the time proof is otherwise required except in the absence of legal capacity.
The claim form is available from your Employer, or you can request a claim form from us. If you do not receive the form from Prudential within 15 days of your request, send Prudential written proof of claim without waiting for the form.
You must notify us immediately when you return to work in any capacity.
How Do You File a Claim?
You and your Employer must fill out your own section of the claim form and then give it to your attending doctor. Your doctor should fill out his or her section of the form and send it directly to
Prudential.
What Information Is Needed as Proof of Your Claim?
Your proof of claim, provided at your expense, must show:
•
That you are under the regular care of a doctor .
•
Appropriate documentation of your monthly earnings.
•
The date your disability or critical illness began.
•
Appropriate documentation of the disabling disorder or critical illness.
•
The extent of your disability, including restrictions and limitations preventing you from performing your regular occupation or any gainful occupation.
•
The name and address of any hospital or institution where you received treatment, including all attending doctors.
•
The name and address of any doctor you have seen.
83500
CCLM-1002 (92821-14)
33
For your Long Term Disability claim, we may request that you send proof of continuing disability, satisfactory to Prudential, indicating that you are under the regular care of a doctor. In some cases, you will be required to give Prudential authorization to obtain additional medical information, and to provide non-medical information (e.g., copies of your IRS federal income tax return, W-2’s and 1099’s) as part of your proof of claim, or proof of continuing disability. This proof, provided at your expense, must be received within 30 days of a request by us. Prudential will deny your claim or stop sending you payments if the appropriate information is not submitted.
For your Critical Illness claim, we may request that you send proof of continuing critical illness, satisfactory to Prudential, indicating that you are under the regular care of a doctor. In some cases, you will be required to give Prudential authorization to obtain additional medical information as part of your proof of claim, or proof of continuing critical illness. This proof, provided at your expense, must be received within 30 days of a request by us. Prudential will deny your claim or stop sending you payments if the appropriate information is not submitted.
Regular care means:
• you personally visit a doctor as frequently as is medically required, according to generally accepted medical standards, to effectively manage and treat your disabling condition(s) or critical illness; and
• you are receiving the most appropriate treatment and care, which conforms with generally accepted medical standards, for your disabling condition(s) or critical illness by a doctor whose specialty or experience is the most appropriate for your disabling condition(s) or critical illness, according to generally accepted medical standards.
Doctor means: a person who is performing tasks that are within the limits of his or her medical license; and
• is licensed to practice medicine and prescribe and administer drugs or to perform surgery; or
• has a doctoral degree in Psychology (Ph.D. or Psy.D.) whose primary practice is treating patients; or
• is a legally qualified medical practitioner according to the laws and regulations of the governing jurisdiction.
Prudential will not recognize any relative including, but not limited to, you, your spouse, or a child, brother, sister, or parent of you or your spouse as a doctor for a claim that you send to us.
Hospital or institution means an accredited facility licensed to provide care and treatment for the condition causing your disability or critical illness.
Who Will Prudential Make Payments To?
Prudential will make payments to you.
83500
CCLM-1002 (92821-14)
34
What Happens If Prudential Overpays Your Claim?
Prudential has the right to recover any overpayments due to:
•
fraud;
• any error Prudential makes in processing a claim; and
• your receipt of deductible sources of income.
You must reimburse us in full. We will determine the method by which the repayment is to be made.
Prudential will not recover more money than the amount we paid you.
What Are the Time Limits for Legal Proceedings?
You can start legal action regarding your claim 60 days after proof of claim has been given and up to 3 years from the time proof of claim is required, unless otherwise provided under federal law.
How Will Prudential Handle Insurance Fraud?
Prudential wants to ensure you and your Employer do not incur additional insurance costs as a result of the undermining effects of insurance fraud. Prudential promises to focus on all means necessary to support fraud detection, investigation and prosecution.
In some jurisdictions, if you knowingly and with intent to defraud Prudential, file an application or a statement of claim containing any materially false information or conceal for the purpose of misleading, information concerning any fact material thereto, you commit a fraudulent insurance act, which is a crime and subjects you to criminal and civil penalties. These actions will result in denial or termination of your claim, and, where such laws apply, are subject to prosecution and punishment to the full extent under any applicable law. Prudential will pursue all appropriate legal remedies in the event of insurance fraud.
83500
CCLM-1002 (92821-14)
35
Glossary
Active employment means you are working for your Employer for earnings that are paid regularly and that you are performing the material and substantial duties of your regular occupation. You must be working at least 18.75 hours per week. If you are a partner or proprietor of the Employer, that work must be in the conduct of the Employer’s business.
Your worksite must be:
•
your Employer’s usual place of business;
• an alternate work site at the direction of your Employer other than your home unless clear specific expectations and duties are documented; or
• a location to which your job requires you to travel.
Normal vacation is considered active employment.
Temporary and seasonal workers are excluded from coverage.
Individuals whose employment status is being continued under a severance or termination agreement will not be considered in active employment.
Activities of daily living means:
•
Bathing - washing oneself by sponge bath, or in either a tub or shower, including the task of getting into or out of the tub or shower;
•
Continence - the ability to maintain control of bowel and bladder function; or, when unable to maintain control of bowel and bladder function, the ability to perform associated personal hygiene
(including caring for catheter or colostomy bag);
•
Dressing - putting on and taking off all items of clothing and any necessary braces, fasteners or artificial limbs;
•
Eating - feeding oneself by getting food into the body from a receptacle (such as a plate, cup or table) or by feeding tube or intravenously;
•
Toileting - getting to and from the toilet, getting on and off the toilet, and performing associated personal hygiene;
•
Transferring - sufficient mobility to move into or out of a bed, chair or wheelchair or to move from place to place, either by walking, using a wheelchair or by other means.
Cognitive impairment means a loss or deterioration in intellectual capacity that is:
• comparable to and includes Alzheimer’s disease and similar forms of irreversible dementia; and
• measured by clinical evidence and standardized tests that reliably measure impairment in the individual’s short-term or long-term memory, orientation as to person, place or time; and deductive or abstract reasoning.
Confined or confinement for this section means a hospital stay of at least 8 hours per day.
83500
CGL-1001 (92821-14)
36
Contract holder means the Employer to whom the Group Contract is issued.
Covered critical illness means heart attack, life-threatening cancer, major organ or tissue transplant, renal failure or stroke.
Critical Illness elimination period means a period of consecutive days which you have survived and which must be satisfied before you are eligible to receive benefits from Prudential. Your critical illness elimination period begins on the date your covered critical illness begins.
Deductible sources of income means income from deductible sources listed in the plan that you receive or are entitled to receive while you are disabled. This income will be subtracted from your gross disability payment.
Disability earnings means the earnings which you receive while you are disabled and working, plus the earnings you could receive if you were working to your greatest extent possible as explained in the plan.
Salary continuance paid to supplement your disability earnings will not be considered payment for work performed.
Doctor means a person who is performing tasks that are within the limits of his or her medical license; and
• is licensed to practice medicine and prescribe and administer drugs or to perform surgery; or
• has a doctoral degree in Psychology (Ph.D. or Psy.D.) whose primary practice is treating patients; or
• is a legally qualified medical practitioner according to the laws and regulations of the governing jurisdiction.
Prudential will not recognize any relative including but not limited to you, your spouse, or a child, brother, sister, or parent of you or your spouse as a doctor for a claim that you send to us.
Eligible survivor means your spouse, if living; otherwise, your children under age 25.
Elimination period (LTD) means a period of continuous disability which must be satisfied before you are eligible to receive benefits from Prudential. If you become covered under a group long term disability plan that replaces this plan during your elimination period, your elimination period under this plan will not be met.
Employee means a person who is in active employment with the Employer for the minimum hours requirement.
Employer means the Contract Holder, and includes any division, subsidiary or affiliate who is reported to Prudential in writing for inclusion under the Group Contract, provided that Prudential has approved such request.
Evidence of insurability means a statement of your medical history which Prudential will use to determine if you are approved for coverage.
Gainful occupation means an occupation, including self employment, that is or can be expected to provide you with an income equal to at least 66 2/3% of your indexed monthly earnings within 12 months of your return to work.
83500
CGL-1001 (92821-14)
37
Gross disability payment means the benefit amount before Prudential subtracts deductible sources of income and disability earnings.
Heart attack means the infarction (death) of a portion of heart muscle, as a result of inadequate blood supply due to obstruction in one or more coronary arteries. To be a covered critical illness, a new occurrence of heart attack (or myocardial infarction) must be demonstrated by the following:
• electrocardiographic changes consistent with and supporting a diagnosis of new heart attack
(myocardial infarction);
• a concurrent diagnostic elevation of cardiac enzymes; and
• imaging studies such as thallium scans, MUGA scans or stress echocardiograms.
Heart attack does not mean:
• congestive heart failure, atherosclerotic heart disease, angina, or coronary artery disease; or
• other dysfunction of the cardiovascular system.
Hospital or institution means an accredited facility licensed to provide care and treatment for the condition causing one’s disability or critical illness.
Indexed monthly earnings means your monthly earnings as adjusted on each July 1 provided you were disabled for all of the 12 months before that date. Your monthly earnings will be adjusted on that date by the lesser of 10% or the current annual percentage increase in the Consumer Price
Index. Your indexed monthly earnings may increase or remain the same, but will never decrease.
The Consumer Price Index (CPI-W) is published by the U.S. Department of Labor. Prudential reserves the right to use some other similar measurement if the Department of Labor changes or stops publishing the CPI-W.
Indexing is only used to determine your percentage of lost earnings while you are disabled and working.
Injury means a bodily injury that:
• is the direct result of an accident;
• is independent of sickness;
• occurs while you are covered under the plan; and
• results in immediate disability.
Disability must begin while you are covered under the plan.
Insured means any person covered under a coverage.
Law, plan or act means the original enactment of the law, plan or act and all amendments.
Leave of absence means you are temporarily absent from active employment for a period of time that has been agreed to in advance in writing by your Employer, other than for reasons in connection with any severance or termination agreement. Your normal vacation time or any period of disability is not considered a leave of absence.
83500
CGL-1001 (92821-14)
38
Life-threatening cancer means a malignant neoplasm which is:
• characterized by uncontrolled growth and spread of malignant cells and the invasion of tissue; and
• is not specifically excluded below.
The term can include leukemia or lymphoma which has been diagnosed as life-threatening.
The diagnosis of a life-threatening cancer must be:
•
made by a doctor;
•
based on pathological evidence; and
•
supported by a clinical evaluation.
A pathological diagnosis of cancer is based on microscopic study of fixed tissue or preparations from the hemic (blood) system. This type of diagnosis must be confirmed by a certified pathologist, whose diagnosis of malignancy is in keeping with the standards set up by the American Board of Pathology.
Life-threatening cancer does not include:
•
early prostate cancer diagnosed as T1N0M0 or equivalent staging.
•
carcinoma in situ. This is a diagnosis of cancer where the tumor cells: lie within the tissue of the site of origin; have not invaded neighboring tissue; and are diagnosed as stage TisN0M0.
• all stages of basal cell carcinoma and squamous cell carcinoma.
• stage 1 T1N0M0 melanoma with a Breslow thickness less than 1.0 mm. This exclusion does not apply to invasive or metastatic malignant melanoma.
• stage 1 Hodgkin’s Lymphoma.
• conditions with the potential to become malignant, pre-malignant lesions, benign tumors or polyps.
Major organ or tissue transplant means end stage major organ or tissue failure that requires your malfunctioning organ or tissue to be replaced with that of a suitable donor by generally accepted medical procedures. Transplanted organs or tissue covered by this definition are limited to liver, kidney, lung, heart, small intestine, pancreas and bone marrow tissue.
For a major organ or tissue transplant to be a covered critical illness under this benefit, you must also be registered in an organ registry as a potential recipient.
Material and substantial duties means duties that:
•
are normally required for the performance of your regular occupation; and
•
cannot be reasonably omitted or modified.
83500
CGL-1001 (92821-14)
39
Maximum monthly benefit means the maximum benefit amount for which you are insured under this plan as shown in the Benefits Highlights.
Maximum period of catastrophic disability payment means the longest period of time Prudential will make catastrophic disability payments to you for any one period of catastrophic disability.
Maximum period of critical illness payment means the longest period of time Prudential will make critical illness payments to you for your critical illness.
Maximum period of payment means the longest period of time Prudential will make payments to you for any one disability.
Mental illness means a psychiatric or psychological condition regardless of cause. Mental illness includes but is not limited to schizophrenia, depression, manic depressive, or bipolar illness, anxiety, somatization, substance related disorders, and/or adjustment disorders or other conditions. These conditions are usually treated by a mental health provider or other qualified provider using psychotherapy, psychotropic drugs, or other similar methods of treatment as standardly accepted in the practice of medicine.
Monthly earnings means your gross monthly income from your Employer as defined in the plan.
Monthly payment means your payment after any deductible sources of income have been subtracted from your gross disability payment.
Part-time basis (LTD) means the ability to work and earn 20% or more of your indexed monthly earnings.
Payable claim means a claim for which Prudential is liable under the terms of the Group Contract.
Plan means a line of coverage under the Group Contract.
Recurrent disability means a disability which is:
• caused by a worsening in your condition; and
• due to the same cause(s) as your prior disability for which Prudential made a Long Term
Disability payment.
Reduced hours means you are working less than the number of hours required to be considered in active employment.
Regular care means:
•
one personally visits a doctor as frequently as is medically required, according to generally accepted medical standards, to effectively manage and treat one’s disabling condition(s); and
•
one is receiving the most appropriate treatment and care, which conforms with generally accepted medical standards, for one’s disabling condition(s) by a doctor whose specialty or experience is the most appropriate for one’s disabling condition(s), according to generally accepted medical standards.
Regular occupation means the occupation you are routinely performing when your disability begins.
Prudential will look at your occupation as it is normally performed instead of how the work tasks are performed for a specific employer or at a specific location.
Rehabilitation program means a program designed to assist you to return to work.
83500
CGL-1001 (92821-14)
40
Renal (kidney) failure (or “end stage renal disease”) means chronic and irreversible failure of both kidneys, which requires weekly or more frequent dialysis treatment. To be a covered critical illness under this benefit, the diagnosis of renal failure must be:
•
made by a doctor who is a board certified nephrologist; and
•
supported by objective testing and treatment.
Retirement plan means a defined contribution plan or defined benefit plan. These are plans which provide retirement benefits to employees and are not funded entirely by employee contributions.
Sickness means any disorder of your body or mind, but not an injury; pregnancy including abortion, miscarriage or childbirth. Disability must begin while you are covered under the plan.
Stroke means a cerebrovascular accident resulting in permanent neurological impairment from infarction (death) of brain tissue as a result of cerebral hemorrhage, embolism or thrombosis that results in:
•
significant impairment in cognition or mobility;
•
complete or partial loss of function involving motion or sensation of part of the body; and
•
measurable and documented permanent neurological deficits.
The diagnosis of stroke must be confirmed by neuroimaging studies such as CAT scan or MRI.
Stroke does not include head injury, transient ischemic attack (TIA) or other cerebrovascular insufficiency.
Substantial assistance means:
• the physical assistance of another person without which one would not be able to perform an activity of daily living; or
• the constant presence of another person within arm’s reach which is necessary to prevent, by physical intervention, injury to oneself while one is performing an activity of daily living.
Substantial supervision means continual oversight that may include cueing by verbal prompting, gestures, or other demonstrations by another person, and which is necessary to protect one from threats to one’s health or safety.
Temporary layoff means you are temporarily absent from active employment for a period of time that has been agreed to in advance in writing by your Employer, other than for reasons in connection with any severance or termination agreement. Your normal vacation time, any period of disability or
FMLA leave is not considered a temporary layoff.
Terminally ill Employee means an employee whose life expectancy is within the period of time stated in the plan.
We, us, and our means The Prudential Insurance Company of America.
You means a person who is eligible for Prudential coverage.
83500
CGL-1001 (92821-14)
41
The Claims and Appeals section is not part of the
Group Insurance Certificate.
Claims and Appeals (92821-14)
Plan Benefits Provided by
The Prudential Insurance Company of America
751 Broad Street
Newark, New Jersey 07102
This Group Contract underwritten by The Prudential Insurance Company of America provides insured benefits. For all purposes of this Group Contract, the Employer/Policyholder acts on its own behalf or as an agent of its employees. Under no circumstances will the
Employer/Policyholder be deemed the agent of The Prudential Insurance Company of America, absent a written authorization of such status executed between the Employer/Policyholder and
The Prudential Insurance Company of America. Nothing in these documents shall, of themselves, be deemed to be such written execution.
Claim Procedures
1. Determination of Benefits
Prudential shall notify you of the claim determination within 45 days of the receipt of your claim. This period may be extended by 30 days if such an extension is necessary due to matters beyond the control of the plan. A written notice of the extension, the reason for the extension and the date by which the plan expects to decide your claim, shall be furnished to you within the initial 45-day period. This period may be extended for an additional 30 days beyond the original 30-day extension if necessary due to matters beyond the control of the plan. A written notice of the additional extension, the reason for the additional extension and the date by which the plan expects to decide on your claim, shall be furnished to you within the first 30-day extension period if an additional extension of time is needed.
However, if a period of time is extended due to your failure to submit information necessary to decide the claim, the period for making the benefit determination by Prudential will be tolled (i.e., suspended) from the date on which the notification of the extension is sent to you until the date on which you respond to the request for additional information.
If your claim for benefits is denied, in whole or in part, you or your authorized representative will receive a written notice from Prudential of your denial. The notice will be written in a manner calculated to be understood by you and shall include:
(a) the specific reason(s) for the denial,
(b) references to the specific plan provisions on which the benefit determination was based,
(c) a description of any additional material or information necessary for you to perfect a claim and an explanation of why such information is necessary,
(d) a description of Prudential’s appeals procedures and applicable time limits, and
(e) if an adverse benefit determination is based on a medical necessity or experimental treatment or similar exclusion or limit, an explanation of the scientific or clinical judgment for the determination will be provided free of charge upon request.
Claims and Appeals (92821-14)
2. Appeals of Adverse Determination
If your claim for benefits is denied or if you do not receive a response to your claim within the appropriate time frame (in which case the claim for benefits is deemed to have been denied), you or your representative may appeal your denied claim in writing to Prudential within 180 days of the receipt of the written notice of denial or 180 days from the date such claim is deemed denied. You may submit with your appeal any written comments, documents, records and any other information relating to your claim. Upon your request, you will also have access to, and the right to obtain copies of, all documents, records and information relevant to your claim free of charge.
A full review of the information in the claim file and any new information submitted to support the appeal will be conducted by Prudential, utilizing individuals not involved in the initial benefit determination. This review will not afford any deference to the initial benefit determination.
Prudential shall make a determination on your claim appeal within 45 days of the receipt of your appeal request. This period may be extended by up to an additional 45 days if
Prudential determines that special circumstances require an extension of time. A written notice of the extension, the reason for the extension and the date that Prudential expects to render a decision shall be furnished to you within the initial 45-day period. However, if the period of time is extended due to your failure to submit information necessary to decide the appeal, the period for making the benefit determination will be tolled (i.e., suspended) from the date on which the notification of the extension is sent to you until the date on which you respond to the request for additional information.
If the claim on appeal is denied in whole or in part, you will receive a written notification from Prudential of the denial. The notice will be written in a manner calculated to be understood by the applicant and shall include:
(a) the specific reason(s) for the adverse determination,
(b) references to the specific plan provisions on which the determination was based,
(c) a statement that you are entitled to receive upon request and free of charge reasonable access to, and make copies of, all records, documents and other information relevant to your benefit claim upon request,
(d) a description of Prudential’s review procedures and applicable time limits,
(e) a statement that you have the right to obtain upon request and free of charge, a copy of internal rules or guidelines relied upon in making this determination, and
(f) a statement describing any appeals procedures offered by the plan.
If a decision on appeal is not furnished to you within the time frames mentioned above, the claim shall be deemed denied on appeal.
If the appeal of your benefit claim is denied or if you do not receive a response to your appeal within the appropriate time frame (in which case the appeal is deemed to have been denied), you or your representative may make a second, voluntary appeal of your denial in writing to Prudential within 180 days of the receipt of the written notice of denial or 180 days from the date such claim is deemed denied. You may submit with your second appeal any written comments, documents, records and any other information relating to your claim.
Claims and Appeals (92821-14)
Upon your request, you will also have access to, and the right to obtain copies of, all documents, records and information relevant to your claim free of charge.
Prudential shall make a determination on your second claim appeal within 45 days of the receipt of your appeal request. This period may be extended by up to an additional 45 days if Prudential determines that special circumstances require an extension of time. A written notice of the extension, the reason for the extension and the date by which Prudential expects to render a decision shall be furnished to you within the initial 45-day period.
However, if the period of time is extended due to your failure to submit information necessary to decide the appeal, the period for making the benefit determination will be tolled from the date on which the notification of the extension is sent to you until the date on which you respond to the request for additional information.
Your decision to submit a benefit dispute to this voluntary second level of appeal has no effect on your right to any other benefits under this plan. If you elect to initiate a lawsuit without submitting to a second level of appeal, the plan waives any right to assert that you failed to exhaust administrative remedies. If you elect to submit the dispute to the second level of appeal, the plan agrees that any statute of limitations or other defense based on timeliness is tolled during the time that the appeal is pending.
If the claim on appeal is denied in whole or in part for a second time, you will receive a written notification from Prudential of the denial. The notice will be written in a manner calculated to be understood by the applicant and shall include the same information that was included in the first adverse determination letter. If a decision on appeal is not furnished to you within the time frames mentioned above, the claim shall be deemed denied on appeal.
Claims and Appeals (92821-14)
92821, LTD, Faculty-Staff Members, Ed 06-2010, 14