Oligosaccharidoses and Related Disorders 19
advertisement

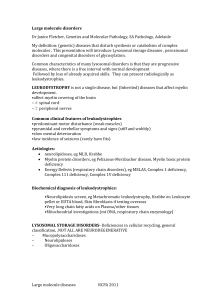
19 Oligosaccharidoses and Related Disorders Generoso Andria, Giancarlo Parenti 19.1 Introduction The oligosaccharidoses are a group of lysosomal storage disorders characterized by defects of glycoprotein degradation due to the deficiency of specific lysosomal enzymes (Fig. 19.1). All are inherited as autosomal recessive traits. The diagnosis is suggested by the clinical picture. Two general features of lysosomal storage diseases need to be considered. First, although some signs are quite specific or even pathognomonic, an overlap in the clinical presentation often exists between the oligosaccharidoses and other lysosomal storage disorders, and the mucopolysaccharidoses (see Chap. 17). Second, the same enzymatic defect can be responsible for different clinical presentations, variable age of onset, severity and organ involvement. Section 19.4 summarizes the clinical features observed in oligosaccharidoses and related disorders with an early (infantile) presentation, and symptoms described in the late onset types. The same enzymes are responsible for both the early and late onset variants. Once a lysosomal storage disorder has been considered in a differential diagnosis, a laboratory evaluation must be initiated in order to define biochemically the diagnosis. Two types of urinary screening tests are easily accessible to look for the abnormal excretion of either oligosaccharides or mucopolysaccharides. If positive, this suggests either a disorder in the metabolism of oligosaccharides or of the mucopolysaccharides. The final diagnosis always requires specific enzymatic confirmation in the appropriate biological material (generally leukocytes or cultured skin fibroblasts extracts, rarely plasma). When the screening tests are negative but suspicion is still high, the resolution of the diagnosis may be provided by various assays of lysosomal enzymes, selected on the basis of a thorough clinical examination. A clinical approach, combined with simple laboratory tests, is suggested in the diagnostic flow-charts (see Figs. 19.2, 19.3). Due to the extreme phenotypic variability of many of these disorders, all proposed diagnostic flow-charts cannot replace the critical evaluation of the astute clinician. 400 Oligosaccharidoses and Related Disorders The features of lysosomal storage disorders do not meet the requirements for mass screening programs of patients. However, an approach based on the detection of markers, such as lysosomal-associated membrane proteins (LAMP-1 and LAMP-2), has been recently proposed for mass screening of patients with lysosomal storage diseases. Carrier screening programs have been proposed or implemented in populations where a certain disorder is particularly frequent. Examples are aspartylglucosaminuria in Finland or Tay-Sachs disease and Gaucher disease, quite common among Ashkenazi Jews (carrier frequency of 0.032 and 0.10, respectively). Until a few years ago no efficacious treatment was available for lysosomal storage disorders and a biochemically defined diagnosis was requested only for the genetic counseling, eventually leading to a prenatal diagnosis in pregnancies at risk. Recently, exciting progresses have been made in the treatment of lysosomal storage disorders, based on bone marrow transplantation or enzyme replacement, as in Gaucher disease and other lysosomal storage disorders. In this respect, any patient with a suspicion of lysosomal storage disease is a potential candidate for new therapeutic strategies and deserves a precise diagnosis. 19.2 Nomenclature No. Disorder Oligosaccharidoses 19.1.1 a-Mannosidosis type I 19.1.2 a-Mannosidosis type II 19.2.1 b-Mannosidosis infantile 19.2.2 b-Mannosidosis juvenile/adult 19.3 Fucosidosis 19.4.1 Sialidosis severe infantile 19.4.2 Sialidosis mild infantile (mucolipidosis I) 19.4.3 Sialidosis adult 19.5.1 Galactosialidosis (early infantile) Enzyme/protein defect Chromosome localization McKusick number a-Mannosidase 19cen-q12 248500 b-Mannosidase 4q22-q25 248510 a-Fucosidase a-Neuraminidase 1p34 6p21.3 230000 256550 “Protective protein”/cathepsin 20q13.1 A deficiency (Secondary b-galactosidase and a-neuraminidase deficiencies) 19.5.2 Galactosialidosis (late infantile) 19.5.3 19.6 19.7.1 19.7.2 Galactosialidosis (juvenile/adult) Aspartylglucosaminuria Aspartylglucosaminidase a-NAGA deficiency type I (Schindler disease) a-N-acetylgalactosaminidase a-NAGA deficiency type II (Kanzaki disease) 4q32-q33 22q11 256540 208400 104170 Nomenclature No. Disorder Related disorders 19.8.1 GM1 gangliosidosis (early infantile) 19.8.2 GM1 gangliosidosis (late infantile) 19.8.3 GM1 gangliosidosis (adult) 19.9.1 GM2 gangliosidosis variant B, infantile (Tay-Sachs disease) 19.9.2 Variant B, late onset 19.9.3 Variant 0, infantile (Sandhoff disease) 19.9.4 Variant 0, juvenile/adult 19.9.5 Variant AB 19.10 Mucolipidosis II (I-cell disease) 19.11 Mucolipidosis III 19.12 Mucolipidosis IV 19.13.1 19.13.2 19.13.3 19.13.4 19.14.1 19.14.2 19.14.3 19.15.1 Gaucher disease Type 1 (“adult”, chronic nonneuronopathic) Type 2 (acute neuronopathic) Type 3 (subacute neuronopathic) Gaucher disease (SAPC deficiency) Niemann-Pick disease type A Niemann-Pick disease type B Niemann-Pick disease type B (adult) Niemann-Pick disease type C (acute) 19.15.2 19.15.3 19.16.1 19.16.2 19.17 Niemann-Pick disease type C (classic) Niemann-Pick disease type C (adult) Krabbe disease infantile Krabbe disease late onset Multiple sulfatase deficiency Enzyme/protein defect Chromosome localization McKusick number b-Galactosidase 3p21.33 230500 b-Hexosaminidase A (b-subunit) 15q23-q24 272800 b-Hexosaminidase A and B (a-subunit) b-Hexosaminidase activator N-acetylglucosamine 1-phosphotransferase (secondary multiple lysosomal enzyme deficiencies) N-acetylglucosamine 1-phosphotransferase (secondary multiple lysosomal enzyme deficiencies) Mucolipidin (receptor-stimulated cation channel) b-Glucocerebrosidase 5q13 268800 5q31.3-q33.1 4q21-q23 272750 252500 4q21-q23 252500 19p13.3-p13.2 252650 1q21 230800 SAPC Sphingomyelinase 10q22.1 11p15.4-p15.1 176801 257200 Abnormal intracellular cholesterol transport 18q11-q12 257220 b-Galactocerebrosidase 14q31 245200 Posttranslational modification of a cysteine in at least 12 sulfatases 272200 401 402 Oligosaccharidoses and Related Disorders 19.3 Metabolic Pathway Fig. 19.1. Degradation of complex oligosaccharides The degradation of a hypothetical complex oligosaccharide by lysosomal enzymes known to be deficient in human diseases. This is only an example of a complex molecule which can accumulate in oligosaccharidoses. The numbers in bold indicate the diseases (listed in Sect. 19.2) in which the defect in the cleavage of a specific glycosidic bond (in italics) is present. A variety of oligosaccharides can accumulate in body fluids and tissues as a consequence of the enzymatic defects; however, structural studies of the storage compound are not relevant to the diagnosis. The demonstration of an abnormal oligosacchariduria by thin-layer chromatography (TLC) is the only established screening test for this group of diseases. The final diagnosis relies upon the demonstration of the specific enzyme defect. Asn = asparagine; Fuc = fucose; GlcNAc = N-acetylglucosamine; Man = mannose; Gal = galactose; SA = sialic acid (modified according to ref. [1]). Signs and Symptoms 403 19.4 Signs and Symptoms Table 19.1. Oligosaccharidoses with early infantile presentation System Symptoms/markers Disorders 19.1.1 19.2.1 19.3 19.4.1 19.4.2 19.5.1 19.5.2 19.6 Clinical Age (yr) at onset course Age (yr) at death Frequency <1 <10 100 cases 1–2 a 10 cases <1–2 <10–a 100 cases <0.5 <1–7 <20 cases <1–3 10–20 <50 cases <0.3 <2 20 cases 1–3 a <20 cases Facies ++ + + + ++ ± ++ ± ++ ± ++ + 1–5 <1 a 100 very cases; rare Finnish: 1:17000 + ± ± + + + ++ + ± ± ++ ++ + + ++ ++ ++ ++ + + + + ± + + + ± + + ± ± + ++ + ± ± ± ± + ± ++ + Skeleton Eye Ear CNS Cardiac Hurler-like phenotype Macrocephaly Microcephaly Short stature/growth disturbance Disostosis multiplex Vertebral changes Osteolysis/osteonecrosis Corneal opacities Lens opacities Cherry-red spot Optic atrophy Hearing loss Mental retardation Progressive neurological course/dementia Seizures Startle reaction to sound Myoclonus Ataxia Pyramidal signs spasticity Hypotonia Ophthalmoplegia/strabismus Hypertrophy/valvular thickening Kidney involvement/edema Hepatomegaly Splenomegaly Hernias Angiokeratoma Renal Liver Spleen GI Dermatologic Special Vacuolar lymphocytes/foamy laboratory bone marrow histiocytes Reduced nerve conduction velocity Increased acid phosphatase a, Adulthood; blank, not reported. ++ + + ++ + ± + + ± ++ + ++ + + + + + + + + + + + + + + + + + + ± ± ± + + + + + + + ± ± ± + + + + ++ ++ ++ + + + + ++ + + + + + + + ++ ++ ++ ++ + + 19.7.1 + + ++ ++ + ± + + + + + 404 Oligosaccharidoses and Related Disorders Table 19.2. Other lysosomal storage disorders with early (infantile) presentation System Symptoms/markers Disorders 19.8.1 19.8.2 19.9.1 Clinical course Age (yr) at onset Age (yr) at death Frequency <0.5 <2 rare 0.5–2 3–10 <0.5 <0.5 2–4 2–4 1:300000 1:300000 Non-Jewish 1:4000 Jewish Facies + ± Skeleton Eye Ear CNS Cardiac Renal Liver Spleen GI Dermatologic Special laboratory Hurler-like phenotype Macrocephaly Microcephaly Short stature/growth disturbance Disostosis multiplex Vertebral changes Osteolysis/osteonecrosis Chondrodysplasia punctata Corneal opacities Lens opacities Cherry-red spot Optic atrophy Retinal degeneration Hearing loss Mental retardation Progressive neurological course/dementia Seizures Startle reaction to sound Myoclonus Ataxia Pyramidal signs/spasticity Hypotonia Ophthalmoplegia/strabismus Hypertrophy/valvular thickening Kidney involvement/edema Hepatomegaly Splenomegaly Hernias Angiokeratoma Ichthyosis Vacuolar lymphocytes/foamy bone marrow histiocytes Reduced nerve conduction velocity Increased acid phosphatase a, Adulthood; blank, not reported. 19.9.3 19.9.5 19.10 <0.5 2–4 very rare 0–1 5–8 rare ++ + + + + + ++ ± + ++ + + + + + + ++ ++ ++ + ++ ++ ++ ++ ++ ++ + + + + ++ ++ ++ ++ ++ ++ ++ + + + + + + + ++ ± + + + + ± ± ++ ± + ± + Signs and Symptoms 405 19.11 19.12 19.13.2 19.13.3 19.14.1 19.14.2 19.15.1 19.15.2 19.16.1 19.17 2–4 a rare 0–1 <1 <2 1:500000 <1–20 0–1 <5 rare 0.3 0.2 <8 1:150000 0–20 <1–a <0.5 1–2 1:100000 <1 3–10 50 cases rare 1:100000 ± + + + + + + + + + + ± ++ ± + ++ + ± + + + ± ± ± + + ++ ++ ++ ++ + ++ + ± ++ + ++ ++ + + + + ++ ++ + + + + ++ + ++ ++ ± ± ++ ++ ++ ++ ++ ++ ++ ++ + + + + + ++ ++ ++ ++ ++ ++ + + ++ + + + + + ++ ++ 406 Table 19.3. Oligosaccharidoses and related disorders with late (juvenile/adult) presentation Symptoms/markers Disorders 19.1.2 19.2.2 19.4.3 19.5.3 19.7.2 19.8.3 19.9.2 19.9.4 19.13.1 Clinical Age (yr) at onset course Age (yr) at death Frequency 1–4 a 100 cases 10–20 a 10 cases 10–20 a <20 cases 10–20 a 50 cases >20 <10 >20 rare 2–15 10–20 rare 3–30 <1–a >20 a 1:60000 rare non-Jewish 1:600 Jewish Facies ± ++ + Skeleton Eye Ear CNS Hurler-like phenotype Macrocephaly Microcephaly Short stature/growth disturbance Disostosis multiplex Vertebral changes Osteolysis/osteonecrosis Chondrodysplasia punctata Corneal opacities Lens opacities Cherry-red spot Optic atrophy Retinal degeneration Hearing loss Mental retardation Progressive neurological course/dementia Seizures Startle reaction to sound Myoclonus Ataxia Pyramidal signs/ spasticity Hypotonia Ophthalmoplegia/ strabismus very rare rare 19.14.3 19.15.3 19.16.2 >20 3–10 1:150000 rare + + + + ± + ++ + ++ + + ++ ++ + + + ± ± ± ++ + ± ± ++ + ± + + + + + + ++ + + ++ + ± + + ± + + + + ± + + ± + + + + + ± + + + + + + Oligosaccharidoses and Related Disorders System Table 19.3 (continued) System Symptoms/markers Disorders 19.1.2 Cardiac Renal Liver Spleen GI Dermatologic Hypertrophy/valvular thickening Kidney involvement/ edema Hepatomegaly + Splenomegaly + Hernias Angiokeratoma Ichthyosis Special Vacuolar lympholaboratory cytes/foamy bone marrow histiocytes Reduced nerve conduction velocity Increased acid phosphatase + 19.2.2 19.4.3 19.5.3 19.7.2 19.8.3 19.9.2 19.9.4 19.13.1 19.14.3 19.15.3 ++ ++ + + ± ± ++ ++ ± 19.16.2 ++ + + ± + ++ + ± ± ++ a, Adulthood; blank, not reported. Signs and Symptoms 407 408 Oligosaccharidoses and Related Disorders 19.5 Laboratory Diagnosis The diagnosis of oligosaccharidoses and related disorders relies upon the assay of the deficient enzymatic activities. For all of them DNA analysis is also available and, if required, can be used. For mucolipidosis IV an enzymatic assay is not available, but molecular analysis is feasible and can be used for prenatal diagnosis. Disorder Enzyme defect c Oligosaccharides (U) d Material Postnatal diagnosis Prenatal diagnosis 19.1 19.2 19.3 19.4 19.5 19.6 19.7 19.8 19.9 19.10 19.11 19.13 19.14 19.15 19.16 19.17 a a-Mannosidase b-Mannosidase a-Fucosidase a-Neuraminidase a-Neuraminidase and b-galactosidase (secondary deficiencies) Aspartylglucosaminidase a-N-Acetylgalactosaminidase b-Galactosidase b-Hexosaminidase A and B N-Acetylglucosamine 1-phosphotransferase Multiple lysosomal enzyme activities (secondary deficiencies) N-Acetylglucosamine 1-phosphotransferase Multiple lysosomal enzyme activities (secondary deficiencies) b-Glucocerebrosidase Sphingomyelinase Abnormal cholesterol esterification b-Galactocerebrosidase Multiple sulfatase activities WBC, FB WBC, FB WBC, FB FB FB b CV, AFC CV, AFC CV, AFC CCV, AFC CCV, AFC : : : : : WBC, FB WBC, FB WBC, FB P, WBC, FB FB FBb CV, AFC CV, AFC CV, AFC CV, AFC CV CCV, AFC : : : :a : FB FBb CV CCV, AFC : WBC, FB WBC, FB FB WBC, FB P, WBC, FB CV, AFC CCV, AFC CCV, AFC CV, AFC CV, AFC Only in GM2 gangliosidosis, variant 0 (Sandhoff disease). Diagnosis is also based on high levels of some extracellular enzyme activities (b-hexosaminidase, arylsulfatase A, a-mannosidase, etc.) in plasma or amniotic fluid supernatant. c Diagnostic tests. The diagnosis of this group of lysosomal storage disorders relies upon the demonstration of a profound deficiency of a specific enzymatic activity, assayed in the appropriate material (as indicated in this table). Since assay conditions are very variable in relation to type of substrate, source of enzyme, etc. no reference values are given here. The physician should refer to the normal range of enzymatic activity under established assay conditions, as provided by the diagnostic laboratory. The interpretation of the results is generally clear-cut, since enzymatic activities in controls are much higher than in patients, but can overlap with the heterozygote range. An apparently normal enzymatic activity can be found in vitro for some variants of lysosomal disorders due to in vivo deficiency of an activator of the enzyme: this is seen, for example, in some cases of Sandhoff disease and Gaucher disease and requires a more complex and careful laboratory workup. Enzymatic pseudodeficiencies have also been reported for some lysosomal storage diseases, such as metachromatic leukodystrophy and GM2 gangliosidosis. d Screening tests: Thin-layer chromatography of urinary oligosaccharides is the most useful, simple and reliable screening test for this group of diseases (see Chap. D for the interpretation). b Diagnostic Flow Charts 409 19.6 Diagnostic Flow Charts Clues to the diagnosis Clinical presentations Mental retardation a Mental retardation Visceromegaly Vacuolated lymphocytes foamy histiocytes Mental retardation Hurler-like phenotype b Mental retardation Visceromegaly Visceromegaly Visceromegaly Visceromegaly Vacuolated lymphocytes foamy histiocytes Vacuolated lymphocytes foamy histiocytes Vacuolated lymphocytes foamy histiocytes Vacuolated lymphocytes foamy histiocytes Hurler-like phenotype Hurler-like phenotype Macular cherry-red spot d Y Suggested Diagnoses c • GM2 gangl. 0 (100 %) • GM2 gangl. B (100 %) N Y N Y N Y • Sialidosis • Niemann • α-NAGA • Niemann-Pick d. Pick d. B • Gaucher sev. inf. (25 %) def. type I A (50 %) (rare) d. type 1 • Sialidosis • Krabbe d. mild. inf. (100 %) • Gaucher d. • Metachromatic • Galactosialidosis types 2, 3 leukodysrophy early inf. (30 %) • Niemann-Pick d. • GM1 gangl. C acute, classic early inf. (50 %) N • α-Mannosidosis • • Fucosidosis • Aspartylglucosaminuria e • GM1 gangl. late inf. e • Mucolipidosis II, III • MPS IH, II, III, VII • Multiple sulf. def. • Infantile sialic acid storage d. Y N Galacto- • MPS IS, sialidosis VI Late inf. (50 %) Fig. 19.2. Clinical approach to the diagnosis of oligosaccharidoses and related lysosomal disorders with early (infantile) onset. a Associated with CNS involvement of various types. b Facial dysmorphism and/or skeletal (vertebral) involvement suggestive of dysostosis multiplex. c Bold: conditions associated with abnormal oligosacchariduria; italics: conditions associated with abnormal mucopolysacchariduria. d The percentage of patients showing macular cherry-red spot (when present) is indicated in parentheses. e Absence of visceromegaly 410 Oligosaccharidoses and Related Disorders Coarse Hurler-like face Abnormal mucopolysacchariduria Y N Mucopolysaccharidoses Abnormal oligosacchariduria Y Oligosaccharidoses and related disorders N Other non-metabolic disorders * Fig. 19.3. Diagnostic flow-chart for patients with coarse Hurler-like face. *Coffin-Lowry syndrome (MIM 303300); Coffin-Siris syndrome (MIM 135900); frontometaphyseal dysplasia (MIM 305620); Sotos syndrome (MIM 117550); Williams syndrome (MIM 194050); multiple neuroma syndrome (MIM 171400); pachydermoperiostosis (MIM 167100); acromegaloid facial appearance syndrome (MIM 102150); Costello syndrome (MIM 218040); Patterson David syndrome (MIM 169170); Schinzel-Giedeon syndrome (MIM 269150); Fountain syndrome (MIM 229120); PallisterKillian syndrome (MIM 601803); Simpson-Golabi-Behmel syndrome (MIM 312870); congenital hypothyroidism. Sialic acid storage disease, a lysosomal transport defect (Chap. 20) should also be considered in the differential diagnosis 19.7 Summary Oligosaccharidoses are inherited diseases showing relevant clinical overlap with other related lysosomal disorders. Analysis of undegraded and accumulated metabolites is used as a screening test only, for oligosaccharidoses as well as for mucopolysaccharidoses. A profound deficiency of a specific enzyme has to be demonstrated for a biochemically defined diagnosis of these diseases. Progresses in molecular genetics have already modified the approach to prenatal, postnatal and heterozygote diagnosis. In the next future they are expected to lead to new forms of treatment, including gene therapy. References 1. Scriver C.R., Beaudet A., Valle D., Sly W.S. (eds.), The metabolic and molecular bases of inherited disease. McGraw-Hill, New York, U.S.A., 2001, 8th edition. Chap. 138, 139, 140, 141, 144, 145, 146, 147, 149, 151, 152, 153 2. Durand P., O’Brien J.S., Genetic errors of glycoprotein metabolism. Edi-Ermes, Milan, Italy, 1982. 3. Warner T.G., O’Brien J.S., Genetic defects in glycoprotein metabolism. Ann. Rev. Genet., 17: 395–441, 1983