Antibiotics: Selected Topics Steven Park, MD/PhD Director, Antimicrobial Stewardship Program
advertisement

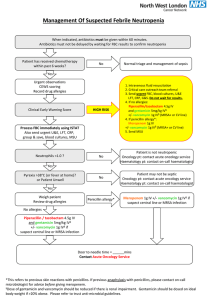
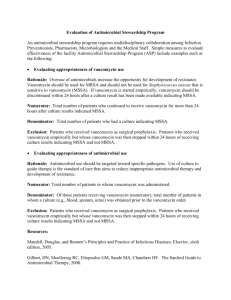
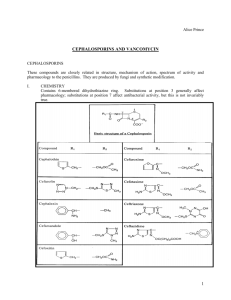
Antibiotics: Selected Topics Steven Park, MD/PhD Director, Antimicrobial Stewardship Program Division of Infectious Diseases UCI Medical Center Case 1 60 yo male admitted for fevers and dysuria. Underwent TURP one week ago for BPH History of previous pyelonephritis secondary to BPH On admission, temperature 102. BP stable. Pulse 105 but after a liter of fluid comes down to 84 WBC 20 with left shift; creatinine 1.0; UA with 140 wbc. Urine sent for culture. Blood cultures drawn. Patient started on ceftriaxone. Patient does not look ill. Complaining of dysuria. Case 1 continued Laboratory calls you the next day and tells you both urine and blood are growing gram negative rods Still febrile CBC 28 Blood pressure and pulse ok Next step? a. b. c. d. e. Continue ceftriaxone Start Zosyn Start cefepime Start ciprofloxacin Start meropenem Next step? a. b. c. d. e. Continue ceftriaxone Start Zosyn Start cefepime Start ciprofloxacin Start meropenem UCI Antibiogram 2014 Case 2 60 yo male transferred from SNF for fever Has been on TPN and has PICC line Febrile with leukocytosis Patient looks ill Chest xray clear. UA negative You suspect PICC line infection. Patient placed on vancomycin and Zosyn Creatinine 2.8. Previous 1.0. Case 2 continued Next day patient’s blood pressure drops and patient intubated Levophed and ADH required to maintain BP Nurse about to start phenylephrine You remove the PICC line Lab calls and states that blood is growing gram negative rods which appear lactose negative You stop vancomycin Next step? a. b. c. d. e. Continue Zosyn Stop Zosyn and start meropenem Stop Zosyn and start cefepime Stop Zosyn and start cefepime and amikacin Stop zosyn and start cefepime and ciprofloxacin Next step? a. b. c. d. e. Continue Zosyn Stop Zosyn and start meropenem Stop Zosyn and start cefepime Stop Zosyn and start cefepime and amikacin Stop zosyn and start cefepime and ciprofloxacin Lactose fermenters Characteristic of gram negative organisms Ability of organism to use lactose as food source Fermenters: E. coli, Enterobacter, Klebsiella Non-fermenters: Pseudomonas, Acinetobacter, Stenotrophomonas UCI Antibiogram 2014 Case 2 continued Patient improves on cefepime and amikacin. Next day only on Levophed Cultures come back Pseudomonas sensitive to cefepime, meropenem, ciprofloxacin, amikacin, resistant to Zosyn Creatinine 3.2 Next step? a. b. c. d. Continue cefepime and amikacin Change to cefepime and ciprofloxacin Continue cefepime only Change to meropenem Next step? a. b. c. d. Continue cefepime and amikacin Change to cefepime and ciprofloxacin Continue cefepime only Change to meropenem Empiric treatment of gram negative bacteremia Really depends on how sick the patient is and how much you need to be right initially After sensitivities back, can narrow down antibiotics No need to routinely double cover Pseudomonas Rely on your local antibiogram Case 1 Patient stable Nosocomial pathogen possible Evidence that patient was failing ceftriaxone Willing to take 50% chance of missing ESBL Case 2 Patient in septic shock Your empiric therapy has to cover the pathogen even at the expense of kidneys We knew that ESBL or CRE was not a factor because of lactose negative GNR If it was, would have used meropenem instead of cefepime Gram negative agents Penicillins Cephalosporins Carbapenems Fluoroquinolones Aminoglycosides Polymixins Aztreonam New agents Penicillins Penicillin, oxacillin, nafcillin, dicloxacillin really no gram negative coverage Amoxicillin/clavulanate (Augmentin) and ampicillin/sulbactam (Unasyn) has some gram negative coverage including anaerobes (not reliable for E. coli so do not use for abdominal infections). Can use for aspiration pneumonia Piperacillin/tazobactam (Zosyn) broadest coverage including pseudomonas and anaerobes Zosyn sometimes active against ESBL and can use in the urine Cephalosporins Gram negative coverage increases as you go from 1st to 3rd generation and gram positive coverage decreases Only ceftazidime and cefepime will cover pseudomonas Ceftazidime has no gram positive coverage Limited anaerobic coverage except cefoxitin and cefotetan Cefepime sometimes active against ESBL and can use in the urine No enterococcal coverage Carbapenems Ertapenem, imipenem, and meropenem Most reliable agents against ESBL Meropenem and imipenem will cover pseudomonas Ertapenem will not cover pseudomonas and enterococcus and penicillin resistant S. pneumoniae Meropenem considered better than imipenem for gram negatives Imipenem considered better than meropenem for gram positives Some concern with imipenem and seizure threshold Fluoroquinolones Levofloxacin, ciprofloxacin, moxifloxacin Broad gram negative coverage including pseudomonas (not moxifloxacin) Pretty good gram positive coverage (levofloxacin, moxifloxacin better than ciprofloxacin) Moxifloxacin has better anaerobic coverage and can use for abdominal infection Need to add Flagyl to levofloxacin and ciprofloxacin for abdominal infections Watch out for QT prolongation and tendinitis and tendon rupture Aminoglycosides Amikacin, gentamicin, tobramycin Excellent gram negative coverage including pseudomonas No gram positive coverage Very little tissue penetration Good for bacteremia, endovascular infections, and urine infections Nephrotoxic and ototoxic Need to measure levels Polymixins Polymixin E (Colistin), polymixin B Stopped using decades ago. Started using again 10 years ago due to MDR gram negative infections Excellent gram negative coverage including pseudomonas, acinetobacter, ESBL, CRE No gram positive coverage Limited tissue penetration Good for bacteremia, endovascular infections Doesn’t concentrate in urine like aminoglycosides but still nephrotoxic Aztreonam Purely gram negative agent including coverage for pseudomonas Not active against ESBL or CRE Can use in penicillin allergic patients Can not use it for patients allergic to ceftazidime New gram negative agents Ceftolozane/Tazobactam (ZERBAXA) • Recently FDA approved • Has in vitro activity against gram negative pathogens including Pseudomonas and most ESBL enterobacteriaceae • Limited activity against gram positive pathogens • Equally effective as Levaquin for complicated urinary tract infections • Equally effective as Meropenem for complicated intra-abdominal infections (included ESBL) when combined with Flagyl • Limited activity against Acinetobacter Ceftazidime/Avibactam (AVYCAZ) • Recently FDA approved • Has in vitro activity against gram negative pathogens including Pseudomonas and most ESBL enterobacteriaceae and some CRE • Limited activity against gram positive pathogens • Equally effective as Imipenem for complicated urinary tract infections • Equally effective as Meropenem for complicated intra-abdominal infections when combined with Flaygl • Limited activity against Acinetobacter Case 3 70 yo male with Parkinson’s disease admitted for frequent falls Fell today and hit head. CT with small subdural hematoma and patient admitted Denies fevers, chills, sob, cough, dysuria. Complaining of fatigue more than usual. He thinks he needs his Parkinson medications adjusted On admission, afebrile, blood pressure stable. Looks tired but not ill WBC 14 with 85% neutrophils but no left shift UA negative Blood cultures drawn Case 3 continued Next day lab informs you that ¼ blood culture bottles with Staphylococcus aureus, sensitivities pending Patient doing well. Wants to go home. Afebrile. WBC 15. Next step? a. b. c. d. e. Start vancomycin Start daptomycin Start linezolid Start Bactrim No antibiotics since it is probably contaminant given only ¼ bottles and patient with no signs of infection Next step? a. b. c. d. e. Start vancomycin Start daptomycin Start linezolid Start Bactrim No antibiotics since it is probably contaminant given only ¼ bottles and patient with no signs of infection Case 3 continued Next day the other 3 bottles are positive and organism identified as MRSA with vancomycin MIC<0.5; sensitive to daptomycin, linezolid, synercid, gentamicin, rifampin, Bactrim TTE shows 0.5 cm vegetation of native mitral valve Vancomycin continued with good trough levels 5 days later, patient doing well but blood still growing MRSA. Vancomycin MIC still <0.5 Next step? In addition to looking for another source of infection: a. Keep vancomycin b. Start daptomycin c. Add gentamicin to vancomycin d. Add rifampin to vancomycin e. Start linezolid Next step? In addition to looking for another source of infection: a. Keep vancomycin b. Start daptomycin c. Add gentamicin to vancomycin d. Add rifampin to vancomycin e. Start linezolid Staphylococcus aureus Staphylococcus aureus should not be treated as a contaminant Vancomycin is still the mainstay of therapy Combination therapy only for prosthetic valve endocarditis (gentamicin, rifampin) and hardware associated osteomyelitis with retention of hardware (rifampin) Think about failure after 7 days of persistent cultures IDSA guidelines high dose daptomycin with another agent recommended if true failure (B-III) Antimicrobial failure is rare Usually due to lack of source control Abscess Natural course of disease rather than antimicrobial failure Aspiration pneumonia Endovascular infections Other staphylococcus aureus infections Vancomycin Still the mainstay therapy Indicated for all infections Be careful with acute kidney injury Some concern over efficacy recently but this is debatable (MIC creep) Only 14 cases of vancomycin resistant staphylococcus aureus in US total Daptomycin FDA approved for right sided endocarditis and skin/soft tissue infection Can’t use for pneumonia Can increase CPK Can become resistant during treatment Reports of eosinophilic pneumonia Clindamycin FDA approved for serious S. aureus (not MRSA) infections Used in children with MRSA infections causing septic arthritis, osteomyelitis, pneumonia, and lymphadenitis Excellent tissue penetration except brain Inducible resistance can be present so lab needs to D zone test Used mainly for skin/soft tissue infections in adults But based on pediatric data, probably can use in pneumonia, osteomyelitis, septic arthritis Excellent bioavailability Linezolid FDA approved for skin/soft tissue infection and pneumonia Can cause serotonin syndrome in patients taking SSRI’s Myelosuppression (reversible), neuropathy side effects (not reversible) Less resistance reported than daptomycin No clear evidence that linezolid better than vancomycin for nosocomial pneumonia Not recommended for bacteremia (bacteriostatic) and failures reported Tetracyclines Doxycycline FDA approved for skin/soft tissue infection due to S. aureus Data lacking for more invasive infections Minocycline may still work if resistant to doxycycline Tygacil also improved for intra-abdominal infections. Don’t use for bacteremia. Bactrim Not FDA approved for any S. aureus infection Still used quite a bit for skin/soft tissue infection Data lacking for invasive infections Recent open label randomized trial failed to show non-inferiority of Bactrim versus vancomycin (OR 1.4) Synercid FDA approved for skin/soft tissue infections Rarely used these days Usually now for VRE resistant to daptomycin and linezolid High incidence of arthralgias Ceftaroline 5th generation cephalosporin FDA approved for community acquired pneumonia and skin/soft tissue infection Has gram negative coverage in addition to MRSA coverage $400 per day MRSA: Treatment of serious infections For endocarditis, bacteremia, pneumonia, osteomyelitis, necrotizing fasciitis, vancomycin is still first line Daptomycin for bacteremia, endocarditis, osteomyelitis, necrotizing fasciitis Linezolid for pneumonia Clindamycin for pneumonia (based on data on pediatrics) and skin/soft tissue infections, osteomyelitis, septic arthritis Bactrim and doxycycline for skin/soft tissue infections Case 4 45 yo female is admitted with C. difficile colitis C. difficile PCR positive with NAP1 strain Multiple episodes of diarrhea per day Patient febrile with WBC 22K Creatinine 1.8 (previously normal) Tachycardic which responds to 1 liter NS Abdomen mildly distended and tender CT scan with colitis in descending colon but no ileus Next step? a. b. c. d. Start po Flagyl Start po vancomycin Start fidaxomicin Start po vancomycin and IV Flagyl Next step? a. b. c. d. Start po Flagyl Start po vancomycin Start fidaxomicin Start po vancomycin and IV Flagyl Case 4 continued Patient starts to get hypotensive requiring levophed 10 mcg Transferred to unit WBC increases to 38K Still having profuse diarrhea No ileus on imaging Next step? a. b. c. d. Add po Flagyl Add IV Flagyl Add fidaxomicin Add IV Flagyl and rectal vancomycin Next step? a. b. c. d. Add po Flagyl Add IV Flagyl Add fidaxomicin Add IV Flagyl and rectal vancomycin Treatment of C. difficile colitis Mild (leukocytosis<15K; creatinine<1.5 times baseline): use po Flagyl Severe (leukocytosis>15; creatinine>1.5 times baseline): use po vancomycin Severe, complicated (hypotension, megacolon, ileus): use po vancomycin, IV Flagyl, rectal vancomycin (only with ileus) Do not add IV Flagyl unless it is severe and complicated No evidence that increased doses of vancomycin better but most physicians would do it Can get high serum levels of po vancomycin with prolonged therapy in patients with renal failure New guidelines coming soon Case 5 83 yo female is admitted for prosthetic left hip infection Had arthroplasty 2 years ago. 2 weeks ago started to have pain. 4 days ago started to drain pus. Admitted to Fountain Valley and vancomycin started and transferred to UCI. Imaging with 5 cm abscess tracking to hardware Afebrile. Left hip with wound and drainage and some surrounding erythema WBC 8.7 Patient in no acute distress with stable vital signs Case 5 continued Assessment and Plan: 83 year old female with PMHx atrial fibrillation (on eliquis), HTN, HL, DM, prior hip replacement presents for left hip abscess. # left hip abscess: concern for infected hardware vs osteo. Patient not septic at this time - ortho consulted - random vancomycin prior to starting vanc - vancomycin, cefepime - wound culture - blood culture - esr, crp - CT hip - XR hip - norco prn - q2d esr/crp - discuss with patient/family in AM if they want to pursue surgery Case 5 continued HOD3: ID consulted Orthopedic service recommends surgery but patient refuses Patient understands that antibiotics alone will not eradicate infection and suppressive therapy likely ID recommends stop antibiotics and get IR drainage HOD4: IR guided drainage HOD6: Discharged on vancomycin and ceftriaxone pending cultures Cultures negative 2 weeks later seen in ID clinic: creatinine 1.6 (baseline 0.8) with supra-therapeutic vancomycin levels Admitted to Fountain Valley for acute kidney injury likely due to vancomycin toxicity When do you have to start antibiotics right away? And when should you wait until you can get proper cultures? Make every attempt to get cultures if you know that treatment will be prolonged Hardware associated osteomyelitis Diabetic foot infections Endovascular infections Decision to start antibiotics right away depends on the infection and how the sick the patient is Septic shock: Start right away Meningitis: Start right away Bad pneumonia: Start right away Endocarditis: Depends If symptoms have been going on for a while, safe to wait If unsure, call ID fellow or Antimicrobial Stewardship Program attending (me) Case 5: In retrospect Antibiotics should never have gotten started on this patient Patient should have gotten drainage before broad spectrum antibiotics started Possible that vancomycin was not necessary Antibiotics can do harm sometimes Who is hurt by unnecessary antibiotics? Most: Patient Some: Society in general Least: Prescribing physician The easy thing to do is prescribe antibiotics but it may not be the right thing to do. It takes a little bit of courage to not prescribe antibiotics.