Syncope UCI Internal Medicine Core – Mini Lecture Curriculum
advertisement

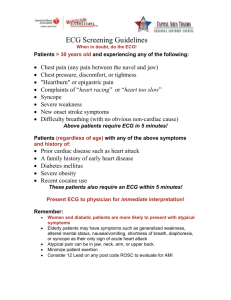
Syncope UCI Internal Medicine Core Curriculum – Mini Lecture Asad Qasim – PGY3 Learning Objectives • Understand the Definition of Syncope • Know the Basic Etiologies of Syncope • Know how to Work-up High vs Low Risk Syncope What is Syncope? • Syncope is the abrupt and transient loss of consciousness associated with absence of postural tone, followed by complete and usually rapid spontaneous recovery. The underlying mechanism is global hypoperfusion of both the cerebral cortices or focal hypoperfusion of the reticular activating system. What is Syncope? • It is important to distinguish Syncope from other causes of T-LOC (Transient Loss of Consciousness) • • • • • • • • Pre-Syncope: lightheadedness without LOC Drop Attack: loss of posture without LOC Coma: LOC without spontaneous recovery Seizure: Tonic-Clonic Movements that start WITH LOC (vs hypoxic myoclonus which can occur with syncope), postictal recovery period Hypoglycemia Hypoxia TIA Cardiac Arrest Etiologies of Syncope • • Neurocardiogenic / Vasovagal Most Common Cardiovascular Most Dangerous • • • Pain/Noxious Stimuli Situational (micturation, cough, defecation) Carotid Sinus Hypersensitivity (CSH) Fear Prolonged standing / heat exposure • • • Arrhythmia – Tachy or Brady Valve Stenosis (outflow obstruction) HOCM (outflow obstruction) • • • • Drugs: BP meds, Diuretics, TCAs Autonomic Insufficiency (Parkinsons, Shy-Dragger, DM, Adrenal Insufficiency) Alcohol Dehydration • • Psuedosyncope TIA or Vertibro-basilar Insufficiency Orthostatic Hypotension “DAAD“ Neuro / Functional / Psychiatric - <5% Work-up and Risk Stratification •The syncope work-up should determine who is at HIGH RISK for a dangerous short-term cardiac event. •All patient should get basic Work-up Including •History/Physical including Orthostatics •Medication Review •ECG. •If age >40, consider Carotid Sinus Massage to assess for Carotid Sinus Hypersensitivity • CONTRAINDICATED if carotid bruit present or recent TIA/Stroke • + Test = bradycardia, hypotension, transient pause/asystole, or prodrome symptoms • All patients should then be Risk Stratified • Adapted from AHA/ACCF Scientific Statement on the Evaluation of Syncope. (Circulation.2006;113:316-327) Work-up and Risk Stratification • Risk Stratification • High Risk: These patients are at high risk for short term cardiac mortality and need appropriate cardiac work-up as an INPATIENT • Evidence of significant heart disease (such as heart failure, low left ventricular ejection fraction, structural abnormality, or previous myocardial infarction). • Clinical (eg palpitations) or ECG features suggesting arrhythmia • Comorbidities such as severe anemia or electrolyte disturbance. • High Risk Work-Up • Echo, Stress test, and/or Ischemic Evaluation • Check for recent Echo and/or TMST before ordering a new one! Consider Posterior Circulation imaging of the brain if suspect Neurological “syncope” • • Carotid Ultrasound has POOR utility in the workup of Syncope and should not be ordered routinely. Work-up and Risk Stratification • Low Risk: Patient’s with no High risk characteristics and/or with highly suspected Vasovagal or Neurocardiogenic Etiology • Single Episode: No further workup indicated • Multiple Episodes: Can workup as outpatient • Patient having FREQUENT Episodes: Holter Monitor or Event Monitor • Patient having INFREQUENT Episodes: Implantable Loop Recorder • These patients DO NOT need “ACS Rule Out” or Imaging (including Head CT or Carotid Ultrasound) Imaging in the Workup of Syncope • So When do I get Brain Imaging? • Neurological Causes of true Syncope are RARE • Bilateral Carotid or Basilar Artery Disease • Non-convulsive Seizure • Head CT is indicated ONLY if the patient has or experienced focal neurological deficits or they experienced head trauma from the event. • Carotid Ultrasound has LOW utility and should NOT be ordered routinely. • Posterior Circulation evaluation with CTA/MRA or Ultrasound is useful only if Vertibro-basilar insufficiency is suspected • Typically present with Dizziness, gait instability, blurry vision, nystagmus, or frank Coma. “Hey its Triage, have this syncope admit” • 71y/o M presents after he passed out while walking up the stairs. He felt slightly lightheaded just prior to the event. Wife saw him fall but was able to quickly arouse him. He had no incontinence or tongue biting. Similar event occurred 2 weeks prior while he was doing yard-work for which he did not seek medical care. He has a long history of DM, and hypertension for which he takes Glipizide, Amlodipine, Lisinopril, and HCTZ. He does not drink. Vitals, orthostatics, and blood sugar are unremarkable. ECG shows left axis deviation and LVH. Exam shows 1+ bilateral edema and 4/6 ejection murmur radiating to the carotids. • What risk category is this patient and how would you proceed with workup? “Hey its Triage, have this syncope admit” • H/P, Orthostatics, ECG, Meds • ECG shows evidence of structural heart disease and exam shows murmur. No orthostasis or suspicious history of vasovagal syncope. Patient has had multiple episodes. • Based on initial workup, patient is High Risk o Needs Admission and Cardiac Work-up including Echocardiogram and Stress Test Dx: Aortic Stenosis “Last admit of the day!” 35y/o healthy M presents with an episode of syncope while standing. He did not experience any prodrome symptoms. This has never happened before. He has no medical history and uses no medications, drugs, or EtoH. Physical exam and ECG are normal. No orthostasis. Carotid massage is negative. Routine labs are unremarkable. • What risk category is this patient and how would you proceed with workup? Last admit of the day! • • • H/P, Orthostatics, ECG, Meds - normal with no obvious cause of syncope Patient is Low Risk and has had only a Single Episode of syncope No Further Work-up Indicated What if the same patient presented with syncope while working out at the gym and physical exam showed a grade III systolic murmur that increased with Valsalva? o Patient is now High Risk given possible structural heart disease and exertional syncope Admit to telemetry for cardiac work-up including Echocardiogram to evaluate for Hypertrophic Cardiomyopathy. Key Points • Key Differential Dx o o o o • Vasovagal/Neurocardiogenic - most common Cardiac – HIGH RISK PATIENTS, most dangerous Orthostatic – “D A A D” Other - Neurologic, Functional, Psych Work-up and Risk Stratification o o H/P, Orthostatics, Meds, ECG, +/- Carotid Massage Risk Stratify • High Risk - Admit w/ cardiac work-up Low Risk - Outpatient workup based on frequency of episodes Brain Imaging ONLY if focal Neuro Deficits or Head trauma References • • • AHA/ACCF Scientific Statement on the Evaluation of Syncope. (Circulation.2006;113:316-327) ESC Guidlines for the Diagnosis and Management of Syncope. (European Heart Journal. 2009. 30;2631-2671) UptoDate Management of Syncope in the Emergency Department Etiology and Pathogenesis of Syncope Diagnosis and Management of Syncope in Adults Cases Adapted from NMS Medicine Casebook. Tilak Shah 2009 o o o •