Clinical Documentation Amish A Dangodara, MD, FACP Professor of Medicine Hospitalist Program
advertisement

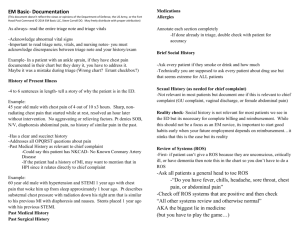
Clinical Documentation Amish A Dangodara, MD, FACP Professor of Medicine Hospitalist Program University of California, Irvine School of Medicine 07.11.14 Need 2 Volunteers: R1 & R3 Clinical Documentation • • • Chief Complaint HPI: 4+ elements of chief complaint Past Hx: 3/3 – PMHx • Medical, Surgical, Psych, OB, etc. • Allergies, Medications – FHx – SHx • • • • • ROS: 9+ systems Exam: 8+ systems or 2 detailed systems Data: 2+ elements Assessment: acute, active, unstable Plan Case Ms. Anne Gina Pektoras is a 56 year old Greek woman who presents with a chief complaint of abdominal pain and shows you the following list: • • • • • • • • • • High BP, 1985 High cholesterol, 1989 Diabetes, 1991 Pancreatitis, 1994 Gall bladder surgery, 1994 Liver failure & sepsis, 1994 Tracheostomy & G-tube, 1994, removed 1995 Blood clot in lung, 1994 Fluid in lung, 2005 Ovarian cancer, 2005, surgery 2006, chemotherapy 2005-2007 • • • • • • • • • Atenolol 100 mg at night Fosinopril 20 mg per day, twice a day Lasix 20 mg per day Glyburide 15 mg per day, 2 in morning, 1 at night Lipitor 40 mg at night Multivitamin 1 daily Calcium/Vitamin D twice a day Vicodin extra 1, 4-5 times a day Iron 325 mg 1 - 2 times a day Case The ED nurse hands you the following information: BP 98/56, P 112, RR 16, T 37.6, Wt 82 Kg Na 146, K 2.9, Cl 114, HCO3 32, BUN 26, Cr 1.4, glucose 54 WBC 6400, Hgb 14.8, Hct 46%, Platelet 273,000 Albumin 3.8, Alk Phos 68, TBil 1.2, AST 24, ALT 22 INR 0.98, PTT 32, CK 427, MB 6.3, MBI 1.5, troponin <0.03 Initial Differential Dx What is the most likely cause of abdominal pain? A) Cardiac B) Gastric/Liver/Pancreas C) Vascular D) Neurological E) Muscular F) Infectious G) Metabolic/Endocrine H) Intestinal I) Neoplastic J) Other Obtain and Review the H&P Exam Vitals: BP 98/56, P 112, RR 16, T 37.6, Wt 82 Kg HEENT: dry oral mucosa Abdomen: slightly distended, old midline scar from pelvic surgery, old scars from prior G-tube and colostomy that was reversed, tympanic to percussion, no HSM, no ascites or other stigmata of chronic liver disease, diffusely tender, but more in LLQ, no peritoneal signs, slightly hyperactive high pitched bowel sounds Pelvic: blind vaginal cuff without discharge or tenderness Rectal: normal tone, non-tender, no blood Extremities: tachycardic pulses, thready, poor skin turgor Rest of exam is normal Assessment What is the most likely cause of abdominal pain? A) Cardiac B) Gastric/Liver/Pancreas C) Vascular D) Neurological E) Muscular F) Infectious G) Metabolic/Endocrine H) Intestinal I) Neoplastic J) Other Plan What initial test(s) will you order? A) Additional cardiac enzymes B) AAS C) CT Abdomen/Pelvis D) Pancreatic enzymes E) Abdominal U/S F) Blood and urine cultures G) ABG H) CT Chest Angiography I) Other H&P HPI: This is a normally independent 56 year old woman who lives alone and presents with 7-9/10 severity, intermittent, achy, pressure-like, sometimes sharp, left-sided abdominal pain, lasting hours to days that began 2 months ago, initially with a frequency 1-2 times per week, and now progressing to nearly daily occurrence for the past week, associated with 1 week of constipation and nausea but without emesis or distention. The pain is exacerbated by eating solids more than liquids but unaffected by positional changes of the body and does not radiate anywhere, but is somewhat improved with eructation and flatus, as well as Vicodin which reduces severity to 3/10. She has reduced dietary intake for 2 days associated with dizziness and weakness, as well as clouded thinking and sweating. She denies alcohol use, hematemesis, BRBPR, or diarrhea. PMHx includes pancreatitis in 1994 and Ovarian cancer in 2005. What is Assessment now? What is the most likely cause of abdominal pain? A) Cardiac B) Gastric/Liver/Pancreas C) Vascular D) Neurological E) Muscular F) Infectious G) Metabolic/Endocrine H) Intestinal I) Neoplastic J) Other Evaluate H&P Summary: HPI HPI: 7 elements of the chief complaint • • • • • • • • • • Location Quality Chronology/Duration Severity/Intensity Associated Symptoms Aggravating or Alleviating factors Impact or intervention Symptoms associated with differential diagnoses for chief complaint, whether positive or negative (ROS pertinent to chief complaint) Important past history or prior work-up that relates to chief complaint Avoid PMHx in first sentence unless VERY pertinent Summary: Past History Past Medical History: • Explain all medications with associated Dx • Approximate onset and current status of problem • Describe specifics if known (complications, how Dx made) • Describe laterality (right shoulder pain, etc) or location (left arm DVT, etc) • Determine nature of allergic reaction, if known • Determine how medications are taken Family History: • Focus on genetically transmitted conditions, infectious exposures, cause of death Social History: • Focus on living situation, relationship, employment, independence, habits, environmental exposures Summary: ROS and Exam ROS: • List by system and label the system • Do not repeat or contradict what was in HPI (copy/paste or templated ROS that is not carefully edited) Exam: • List by system and label the system • Findings should reflect current exam (avoid copy/paste or templated exam that does not apply to patient) • Include pertinent negatives for what you were looking for as a result of presenting problem (rather than templated “standard” negative findings) • List only what you actually examined and only examine what was clinically indicated for patient’s current status (avoid copy/paste or unedited templates) Summary: Data Data: • List findings pertinent to indication for why test was ordered (avoid copy/pasting entire reports or impressions) • List “unexpected” findings only if they are clinically impactful • Trend results if trending reveals important nuance that may not be easily appreciated based on single value • Indicate if you personally interpreted the data or coordinated interpretation with another specialist Summary: Assessment Assessment: • Commit to a Dx or symptom followed by differential Dx, even if not certain (probable, possible, likely, or unlikely are ok) • Avoid a summary of findings without associated Dx • Avoid “rule out” terminology, “FEN,” or “prophylaxis”; indicate risk or Dx • Indicate ICD-10 components: • • • • • • • Dx or symptom followed by differential Dx and likelihood Type or Stage Acuity or severity Location and/or laterality Timing (present on admission, initial presentation, subsequent eval) Etiology (pathogen) Complication of Dx or associated co-morbidity Summary: Plan Plan: • • • • Each plan should have corresponding assessment(s) Provide brief rationale for plan Should logically follow from assessment Include preventive measures on initial plan Questions? Demographics Abdominal Pain: Quali ty Location Dura tion Severity Associated Sx Aggra vated by Reli eved by Impact 56 year old female Achy, pressure -like, sometimes sharp [no burning, no ÒacidityÓ] In the middle of abdomen, but off to the left usua lly Lasts hours to days, [happening for past 2 months, sometimes 1-2 times/wk, now almost every day for past week] 10/10 since last night, but usua lly 7/10, [comes and goes, sometimes no pain] Nausea for past 2 days, no vomiting, [no Òacidity,Óno hematemesis, no blood in stool, no fever or chill s, no diarrhea, no radiation to back, no diverticulosis, no EtOH; positive constipation x 1 week] Eating makes it worse than drinking since yesterday [unchanged by position] 1-2 Vicodin reduces pain to 3/10, [a li ttle better with burping o r flatus; unchanged by position] [I can no longer eat, sometimes feel dizzy, sweaty, cloudy thinking] HTN Dx 1985 [took meds today, home BP 130s/80s but rarely measure, Atenolol 100 mg qHS, Fosinopril 10 mg BID (20 mg/day), Lasix 20 mg/day for leg edema, no known Dx of CHF, no orthopnea] Hyperlipidemia Dx 1989 [Lipitor 40 mg QHS, no muscle aches, no h/o elevated LFTs from Lipitor, liver failure in 1994 was from sepsis] Diabetes II Dx 1991 [took meds today; Glyburide 10 mg (two 5 mg tabs) in AM and 5 mg in PM after meals; AM glucometer < 150, but rarely checks; dimi nished diet and positive hypoglycemic Sx (dizzy, sweaty, cloudy thinking) since yesterday; do not know HgbA1c Pancreatitis Dx 1994 [due to gallstones, had ERCP with sphincterotomy 1994 prior to cholecystectomy, no EtOH, led to DKA, no epigastric pain, no vomiting, no radiation of pain to back; positive nausea] Liver Failure Dx 1994 [due to sepsis, no EtOH, no hepatitis, no stigmata of chronic liver disease (ascites from ovarian cancer resolved after chemotherapy)] Sepsis Dx 1994 [due to cholecystitis, was in ICU Òfor long time,Óhad trach/PEG, subsequently removed, complicated by PE, pathogen not known] PE Dx 1994 [Complication of sepsis, treated with Coumadin Òfor long timeÓbut not more than 1 year, no SOB, no CP, not sure if IVC fil ter placed] Pulmonary edema Dx 2005 [drained fluid from right lung caused by cancer, resolved after chemotherapy, no known h/o CHF, no orthopnea; positive leg edema for years; no known Echo] Ovarian Cancer Dx 2005 [had chemotherapy (does not know drugs) from 20052007, s/p TAH/BSO/debulking with colostomy and takedown 2006 ROS: General HEENT Respiratory Cardiovascular GI GU Musculoskeletal Neurological Endocrine [No fever, chill s, weight change] [No vision, hearing change, no nasal congestion or sore throat; positive for dry mouth x 1 day] [No SOB, cough, sputum, orthopnea] [No CP, palpitations, DOE, no prior stress test, can usua lly clim b up 1 floor stairs] As per HPI Ğ see abdominal pain [No dysuria or polyuria, menopause at age 47] [No joint pain or swelli ng; chronic leg edema since 2005, better with Lasix] [No focal numbness, weakness, seizure, neuropathy] [No polydipsia, polyuria; positive hypoglycemix Sx for 1 day] FHx: Mother: DM, breast cancer, d. age 68 Father: CAD, d. MI age 49 Siblings: 2 have DM Children: 3, healthy SHx: Immi grated to US from Greece at age 17, married at age 19, divorced 1995, former art teacher, li ves alone in first floor apartment o n disabili ty, independent, still paints, daughter li ves nearby, never smoked, does not drink except special occasion, no illi cit drugs Allergies: ÒI think PCN when I was a youngÓ(reaction not known) Medications: Atenolol 100 mg qHS Fosinopril 20 mg/day [(total); 10 mg BID] Lasix 20 mg/day Glyburide 15 mg/day [(tot al) after meals; two 5 mg tabs in AM, one 5 mg tab in PM] Lipitor 40 mg qHS MVI 1 daily Ca/Vit D, 1 tab BID Vicodin ES, 4-5 times/day [uses 1-2 (10 mg) tabs q4-6h PRN] FeSO4 325 mg 1-2 times/d, [325 mg BID, sometimes skips one dose due to constipation]