Breast Imaging: What’s Important? Freddie J. Combs, MD
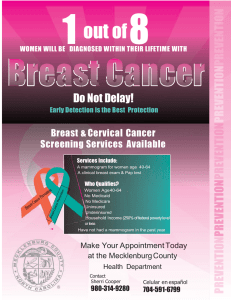
advertisement

Breast Imaging: What’s Important? Freddie J. Combs, MD The Great Mammography Debate The Great Mammography Debate • Breast imaging has long been a source of passionate debate and controversy within the medical community and society at large. The Great Mammography Debate • Breast imaging has long been a source of passionate debate and controversy within the medical community and society at large. • So why all the fuss…???? The Great Mammography Debate • Breast imaging has long been a source of passionate debate and controversy within the medical community and society at large. • So why all the fuss…???? “Because it’s out there, man…It’s out there.” Hot PINK Topic • Seems like you can’t go anywhere these days without seeing PINK. It’s in the News It’s in Hollywood It’s in Advertising It’s in Advertising REALLY!!! ??? Even Here….. Breast Cancer • Let’s start with some useful facts for providers and patients. Some Important Statistics Some Important Statistics • About 1 in 8 women (approx. 12%) and 1 in 1,000 men will develop invasive breast cancer in their lifetime Some Important Statistics • About 1 in 8 women (approx. 12%) and 1 in 1,000 men will develop invasive breast cancer in their lifetime • In 2013 an estimated 299,220 new cases of invasive and non-invasive (in situ) breast cancers were diagnosed in the U.S. Some Important Statistics • About 1 in 8 women (approx. 12%) and 1 in 1,000 men will develop invasive breast cancer in their lifetime • In 2013 an estimated 299,220 new cases of invasive and non-invasive (in situ) breast cancers were diagnosed in the U.S. • Approx. 39,620 women died of Breast cancer in 2013 (2nd only to lung cancer) Rose Bowl holds 93,000 Angel Stadium Holds 45,000 But Wait, There’s More…. • 2nd most common cancer in U.S. women (behind skin cancer) But Wait, There’s More…. • 2nd most common cancer in U.S. women (behind skin cancer) • 30% of all cancers diagnosed in women But Wait, There’s More…. • 2nd most common cancer in U.S. women (behind skin cancer) • 30% of all cancers diagnosed in women • 3,000,000 U.S. breast cancer survivors But Wait, There’s More…. • 2nd most common cancer in U.S. women (behind skin cancer) • 30% of all cancers diagnosed in women • 3,000,000 U.S. breast cancer survivors • 15% diagnosed have a family history. Risk doubles with history in a 1st degree relative But Wait, There’s More…. • 2nd most common cancer in U.S. women (behind skin cancer) • 30% of all cancers diagnosed in women • 3,000,000 U.S. breast cancer survivors • 15% diagnosed have a family history. Risk doubles with history in a 1st degree relative • 85% have no family history. Most breast cancers are not genetically linked Ok, so…you got any Good News? Ok, so…you got any Good News? • Since widespread screening for breast cancer began in the 1990’s there has been a decline in mortality Ok, so…you got any Good News? • Since widespread screening for breast cancer began in the 1990’s there has been a decline in mortality • CDC data from 2001-2010 shows breast cancer mortality rate decreased by 2% per year Ok, so…you got any Good News? • Since widespread screening for breast cancer began in the 1990’s there has been a decline in mortality • CDC data from 2001-2010 shows breast cancer mortality rate decreased by 2% per year • Factors include early detection with improved screening, advances in treatment and increased awareness Mortality Rate 1992-2010 Mortality Rate 1992-2010 Dude…What about Genes?? Dude, what about genes? Dude, what about genes? Dude, what about genes? • 5-10% of breast cancers are linked to specific gene mutations. BRCA1 & 2 most common Dude, what about genes? • 5-10% of breast cancers are linked to specific gene mutations. BRCA1 & 2 most common • BRCA1 carries a 50-80% and BRCA2 a 40-70% risk of developing breast cancer by age 70 Dude, what about genes? • 5-10% of breast cancers are linked to specific gene mutations. BRCA1 & 2 most common • BRCA1 carries a 50-80% and BRCA2 a 40-70% risk of developing breast cancer by age 70 • Cancers in women with gene mutations tend to occur early (before age 50) and may be aggressive HBOC Gene Testing: Who Qualifies • The Patient History: HBOC Gene Testing: Who Qualifies • The Patient History: • Breast cancer at age 50 or younger or ovarian cancer at any age HBOC Gene Testing: Who Qualifies • The Patient History: • Breast cancer at age 50 or younger or ovarian cancer at any age • Male with breast cancer at any age HBOC Gene Testing: Who Qualifies • The Patient History: • Breast cancer at age 50 or younger or ovarian cancer at any age • Male with breast cancer at any age • Ashkenazi Jewish descent and a personal or family history of breast, ovarian or pancreatic cancer (HBOC cancers) (HBOC cancers are Breast, Ovarian and Pancreatic) HBOC Gene Testing: Who Qualifies • The Family History: HBOC Gene Testing: Who Qualifies • The Family History: • 2 breast cancers in the same family member or on the same side of the family HBOC Gene Testing: Who Qualifies • The Family History: • 2 breast cancers in the same family member or on the same side of the family • Family member diagnosed with triple negative breast cancer at any age (ER/PR/Her2Nu all negative) HBOC Gene Testing: Who Qualifies • The Family History: • 2 breast cancers in the same family member or on the same side of the family • Family member diagnosed with triple negative breast cancer at any age (ER/PR/Her2Nu all negative) • Pancreatic cancer and an HBOC-associated cancer in the same person or on same side of the family HBOC Gene Testing: Who Qualifies • The Family History: • 2 breast cancers in the same family member or on the same side of the family • Family member diagnosed with triple negative breast cancer at any age (ER/PR/Her2Nu all negative) • Pancreatic cancer and an HBOC-associated cancer in the same person or on same side of the family • 3 or more breast cancers on the same side of the family HBOC Gene Testing: Who Qualifies • The Family History: • 2 breast cancers in the same family member or on the same side of the family • Family member diagnosed with triple negative breast cancer at any age (ER/PR/Her2Nu all negative) • Pancreatic cancer and an HBOC-associated cancer in the same person or on same side of the family • 3 or more breast cancers on the same side of the family • Known BRCA1 or BRCA2 mutation in the family Affordable Care Act considers gene testing as a preventive measure Aside from Gene Testing, Who’s else is High Risk? • Several models exist for calculating risk. Models may include Lifetime Risk (LTR), Tenyear risk, probability of a BRCA mutation • Tyrer-Cuzick (IBIS), Gail, Claus, BRCAPRO, BOADICEA are the most used models and offer downloadable online versions • IBIS shown to be most consistently accurate model. We use this at PBCC on all patients IBIS examples A more useful IBIS example (IBIS= International Breast Cancer Intervention Study) Enough with the stats, let’s get to the practice related stuff…. Enough with the stats, let’s get to the practice related stuff…. The Basic Questions: Enough with the stats, let’s get to the practice related stuff…. The Basic Questions: • WHO should we evaluate? Enough with the stats, let’s get to the practice related stuff…. The Basic Questions: • WHO should we evaluate? • WHEN should we evaluate them? Enough with the stats, let’s get to the practice related stuff…. The Basic Questions: • WHO should we evaluate? • WHEN should we evaluate them? • HOW should we do it? Enough with the stats, let’s get to the practice related stuff…. The Basic Questions: • WHO should we evaluate? • WHEN should we evaluate them? • HOW should we do it? Answer: It depends on who you ask………. Enough with the stats, let’s get to the practice related stuff…. The Basic Questions: • WHO should we evaluate? • WHEN should we evaluate them? • HOW should we do it? Answer: It depends on who you ask………. So, let’s ask the experts! The USPSTF Says: The USPSTF Says: • Routine screening mammogram every 2 years for women ages 50-74 with consideration for starting earlier biennial screening based on patient’s beliefs regarding benefits and harms. The USPSTF Says: • Routine screening mammogram every 2 years for women ages 50-74 with consideration for starting earlier biennial screening based on patient’s beliefs regarding benefits and harms. • Recommends against teaching SBE (Self-breast Examination). The USPSTF Says: • Routine screening mammogram every 2 years for women ages 50-74 with consideration for starting earlier biennial screening based on patient’s beliefs regarding benefits and harms. • Recommends against teaching SBE (Self-breast Examination). • Insufficient evidence to recommend for or against CBE (Clinical Breast Exam), digital mammography and MRI. The ACR Says (a lot): The ACR Says (a lot): • Yearly mammograms starting at 40 for women at average risk. The ACR Says (a lot): • • Yearly mammograms starting at 40 for women at average risk. Screen women < 40 at increased risk for breast cancer as follows: The ACR Says (a lot): • • Yearly mammograms starting at 40 for women at average risk. Screen women < 40 at increased risk for breast cancer as follows: a. Woman with known mutation or genetic syndrome with increased breast cancer risk: yearly starting by age 30, but not before age 25. The ACR Says (a lot): • • Yearly mammograms starting at 40 for women at average risk. Screen women < 40 at increased risk for breast cancer as follows: a. Woman with known mutation or genetic syndrome with increased breast cancer risk: yearly starting by age 30, but not before age 25. b. Untested women with a first-degree relative with known BRCA mutation: yearly starting by age 30, but not before age 25. The ACR Says (a lot): • • Yearly mammograms starting at 40 for women at average risk. Screen women < 40 at increased risk for breast cancer as follows: a. Woman with known mutation or genetic syndrome with increased breast cancer risk: yearly starting by age 30, but not before age 25. b. Untested women with a first-degree relative with known BRCA mutation: yearly starting by age 30, but not before age 25. c. Woman with a 20% or greater lifetime risk based on breast cancer risk models: yearly starting by age 30, but not before age 25, or 10 years earlier than the age at which the youngest first-degree relative was diagnosed, whichever is later. The ACR Says (a lot): • • Yearly mammograms starting at 40 for women at average risk. Screen women < 40 at increased risk for breast cancer as follows: a. Woman with known mutation or genetic syndrome with increased breast cancer risk: yearly starting by age 30, but not before age 25. b. Untested women with a first-degree relative with known BRCA mutation: yearly starting by age 30, but not before age 25. c. Woman with a 20% or greater lifetime risk based on breast cancer risk models: yearly starting by age 30, but not before age 25, or 10 years earlier than the age at which the youngest first-degree relative was diagnosed, whichever is later. d. Woman with a history of chest (mantle) radiation between the ages of 10 and 30: yearly starting 8 years after the radiation therapy, but not before age 25. The ACR Says (a lot): • • Yearly mammograms starting at 40 for women at average risk. Screen women < 40 at increased risk for breast cancer as follows: a. Woman with known mutation or genetic syndrome with increased breast cancer risk: yearly starting by age 30, but not before age 25. b. Untested women with a first-degree relative with known BRCA mutation: yearly starting by age 30, but not before age 25. c. Woman with a 20% or greater lifetime risk based on breast cancer risk models: yearly starting by age 30, but not before age 25, or 10 years earlier than the age at which the youngest first-degree relative was diagnosed, whichever is later. d. Woman with a history of chest (mantle) radiation between the ages of 10 and 30: yearly starting 8 years after the radiation therapy, but not before age 25. e. Woman with biopsy-proven lobular neoplasia, atypical ductal hyperplasia (ADH), ductal carcinoma in-situ (DCIS), invasive breast cancer, or ovarian cancer: yearly from time of diagnosis, regardless of age. Screening for Breast Cancer • Regardless of which set of recommendations you follow, it all starts with our old friend…. Screening for Breast Cancer • Regardless of which set of recommendations you follow, it all starts with our old friend…. The Mammogram Sensitivity and Specificity for Screening SCREENING TEST(S) SENSITIVITY % SPECIFICITY % Mammogram 71-83 91-93 MRI 75-97 91-96 Mammogram/US 76 84 Mammogram/MRI 84-94 86-95 •Sensitivity of mammography varies depending upon density and Radiologist •Addition of ultrasound and MRI to mammography detects more cancers but leads to an increase in recall rates and procedures (false positives) Ichikawa LE , Barlow WE , Anderson ML , et al .Time trends in radiologists’ interpretive performance at screening mammography fromthe communitybased Breast Cancer Surveillance Consortium, 1996-2004 . Radiology 2010 ; 256 ( 1 ): 74 – 82 Berg WA, Zhang Z, Lehrer D, et al. Detection of Breast Cancer With Addition of Annual Screening Ultrasound or a Single Screening MRI to Mammography in Women With Elevated Breast Cancer Risk. JAMA. 2012;307(13):1394-1404. Kuhl CK, Schrading S, Leutner CC, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol. 23(33):8469-76, 2005. Mammography: Mammography: • Governed by the FDA via the Mammography Quality Standards Act of 1992 (MQSA) • MQSA requires all facilities and technologists that perform mammograms and interpreting physicians to maintain certification (via the ACR) to ensure consistency. • Make sure your patients are going to an accredited facility! Mammography: • May be performed using screen-film or digital technique. Sensitivity is equivalent but digital performs better in dense tissue and allows use of CAD (Computer-Aided Diagnosis) software. Mammography: • May be performed using screen-film or digital technique. Sensitivity is equivalent but digital performs better in dense tissue and allows use of CAD (Computer-Aided Diagnosis) software. Old school- Workin’ Hard Mammography: • May be performed using screen-film or digital technique. Sensitivity is equivalent but digital performs better in dense tissue and allows use of CAD (Computer-Aided Diagnosis) software. Old school- Workin’ Hard VS. New school-Hardly Workin’ Mammography: • There are two categories of Mammogram Mammography: • There are two categories of Mammogram • SCREENING: routine, preventive exam in asymptomatic women. 4 standard views (bilateral CC and MLO) Mammography: • There are two categories of Mammogram • SCREENING: routine, preventive exam in asymptomatic women. 4 standard views (bilateral CC and MLO) • DIAGNOSTIC: evaluation of a specific symptom, clinical finding or to follow-up an abnormal finding on screening or known disease process. May include additional views and/or other modalities Mammography: • There are two categories of Mammogram • SCREENING: routine, preventive exam in asymptomatic women. 4 standard views (bilateral CC and MLO) • DIAGNOSTIC: evaluation of a specific symptom, clinical finding or to follow-up an abnormal finding on screening or known disease process. May include additional views and/or other modalities • IMPORTANT DISTINCTION WHEN ORDERING Screening Mammogram • Two Standard Views: CC and MLO Diagnostic Mammogram Magnification views Other Modalities: Ultrasound Other Modalities: Ultrasound • Most effective as a diagnostic tool Other Modalities: Ultrasound • Most effective as a diagnostic tool • Preferred modality in pregnant or lactating women and women under 30 Other Modalities: Ultrasound • Most effective as a diagnostic tool • Preferred modality in pregnant or lactating women and women under 30 • May be useful as an adjunct to mammogram screening in women with dense breasts and increased lifetime risk that are not able to have MRI, but no current specific screening recommendations Other Modalities: Ultrasound • Most effective as a diagnostic tool • Preferred modality in pregnant or lactating women and women under 30 • May be useful as an adjunct to mammogram screening in women with dense breasts and increased lifetime risk that are not able to have MRI, but no current specific screening recommendations • Best modality for biopsy Other Modalities: Ultrasound • Most effective as a diagnostic tool • Preferred modality in pregnant or lactating women and women under 30 • May be useful as an adjunct to mammogram screening in women with dense breasts and increased lifetime risk that are not able to have MRI, but no current specific screening recommendations • Best modality for biopsy • Operator dependent. Use dedicated breast facility with experienced techs and Radiologist Ultrasound (Fibroadenoma) CCancer on Ultrasound Cyst on US Other Modalities: Breast MRI • High sensitivity and specificity Other Modalities: Breast MRI • High sensitivity and specificity • Does not replace mammography Other Modalities: Breast MRI • High sensitivity and specificity • Does not replace mammography • Recommended as screening tool with mammogram in high risk women (LTR >20%) Other Modalities: Breast MRI • High sensitivity and specificity • Does not replace mammography • Recommended as screening tool with mammogram in high risk women (LTR >20%) • Requires IV Contrast (gadolinium) to evaluate for cancer (Don’t order a non-contrast breast MRI) Other Modalities: Breast MRI • High sensitivity and specificity • Does not replace mammography • Recommended as screening tool with mammogram in high risk women (LTR >20%) • Requires IV Contrast (gadolinium) to evaluate for cancer (Don’t order a non-contrast breast MRI) • No Radiation Other Modalities: Breast MRI • High sensitivity and specificity • Does not replace mammography • Recommended as screening tool with mammogram in high risk women (LTR >20%) • Requires IV Contrast (gadolinium) to evaluate for cancer (Don’t order a non-contrast breast MRI) • No Radiation • Avoid in pregnancy (Gad. is Category C) Other Modalities: Breast MRI • High sensitivity and specificity • Does not replace mammography • Recommended as screening tool with mammogram in high risk women (LTR >20%) • Requires IV Contrast (gadolinium) to evaluate for cancer (Don’t order a non-contrast breast MRI) • No Radiation • Avoid in pregnancy (Gad. is Category C) • Limit in lactation. Avoid nursing for 24 hrs after MRI (pumpand-dump) Breast MRI Indications MRI Cancer with Mets to Axilla 3-D Mammography (Tomosynthesis) 3-D Mammography (Tomosynthesis) • Combines multiple mammo images to reduce tissue overlap (like CT) 3-D Mammography (Tomosynthesis) • Combines multiple mammo images to reduce tissue overlap (like CT) • Does not replace conventional mammogram 3-D Mammography (Tomosynthesis) • Combines multiple mammo images to reduce tissue overlap (like CT) • Does not replace conventional mammogram • Benefit: Improves call back rate and detection 3-D Mammography (Tomosynthesis) • Combines multiple mammo images to reduce tissue overlap (like CT) • Does not replace conventional mammogram • Benefit: Improves call back rate and detection • Requires more radiation 3-D Mammography (Tomosynthesis) • Combines multiple mammo images to reduce tissue overlap (like CT) • Does not replace conventional mammogram • Benefit: Improves call back rate and detection • Requires more radiation • More expensive 3-D Mammography (Tomosynthesis) • Combines multiple mammo images to reduce tissue overlap (like CT) • Does not replace conventional mammogram • Benefit: Improves call back rate and detection • Requires more radiation • More expensive • Trendy but not currently a standard recommendation…Time will tell where it fits in 3-D Mammography (Tomosynthesis) Quick Facts: Implants Quick Facts: Implants • Screening rec’s are the same for women with implants Quick Facts: Implants • Screening rec’s are the same for women with implants • Reduces sensitivity of mammogram (blind spots) but overall cancer outcomes unchanged Quick Facts: Implants • Screening rec’s are the same for women with implants • Reduces sensitivity of mammogram (blind spots) but overall cancer outcomes unchanged • Requires additional views and more radiation Quick Facts: Implants • Screening rec’s are the same for women with implants • Reduces sensitivity of mammogram (blind spots) but overall cancer outcomes unchanged • Requires additional views and more radiation • Risk of rupture caused by a mammogram is very low (but not zero). Experienced facility is key Quick Facts: Implants • Screening rec’s are the same for women with implants • Reduces sensitivity of mammogram (blind spots) but overall cancer outcomes unchanged • Requires additional views and more radiation • Risk of rupture caused by a mammogram is very low (but not zero). Experienced facility is key • MRI is preferred method to eval. implants. FDA rec’s MRI 3 yr. after placed then q2 yrs. (Silicone) Quick Facts: Implants • Screening rec’s are the same for women with implants • Reduces sensitivity of mammogram (blind spots) but overall cancer outcomes unchanged • Requires additional views and more radiation • Risk of rupture caused by a mammogram is very low (but not zero). Experienced facility is key • MRI is preferred method to eval. implants. FDA rec’s MRI 3 yr. after placed then q2 yrs. (Silicone) • Overall rupture rate unknown but studies suggest at least 15% between years 3-10 after placed Implant Rupture (Linguine Sign) Implant Rupture (Key Hole Sign and Free Silicone) Radiation facts for worried patients: Radiation facts for worried patients: • Mammogram should not be routinely performed in women under age 30 or in pregnant women Radiation facts for worried patients: • Mammogram should not be routinely performed in women under age 30 or in pregnant women • Rad exposure is very low: 0.4 mSv (0.1 mSv per view) Radiation facts for worried patients: • Mammogram should not be routinely performed in women under age 30 or in pregnant women • Rad exposure is very low: 0.4 mSv (0.1 mSv per view) • CXR 0.1 mSv for single view Radiation facts for worried patients: • Mammogram should not be routinely performed in women under age 30 or in pregnant women • Rad exposure is very low: 0.4 mSv (0.1 mSv per view) • CXR 0.1 mSv for single view • CT Scan avg. 10 mSv Radiation facts for worried patients: • Mammogram should not be routinely performed in women under age 30 or in pregnant women • Rad exposure is very low: 0.4 mSv (0.1 mSv per view) • CXR 0.1 mSv for single view • CT Scan avg. 10 mSv • Roundtrip plane flight LA to NY is approx. 0.1 mSv Radiation facts for worried patients: • Mammogram should not be routinely performed in women under age 30 or in pregnant women • Rad exposure is very low: 0.4 mSv (0.1 mSv per view) • CXR 0.1 mSv for single view • CT Scan avg. 10 mSv • Roundtrip plane flight LA to NY is approx. 0.1 mSv • Natural background radiation is around 3 mSv/yr. Higher in Colorado (pun intended) Radiation facts for worried patients: • Mammogram should not be routinely performed in women under age 30 or in pregnant women • Rad exposure is very low: 0.4 mSv (0.1 mSv per view) • CXR 0.1 mSv for single view • CT Scan avg. 10 mSv • Roundtrip plane flight LA to NY is approx. 0.1 mSv • Natural background radiation is around 3 mSv/yr. Higher in Colorado (pun intended) • Thyroid exposure is minimal and indirect (similar to 30 min. of natural background radiation) What is the official mascot of the Radiologist? THE HEDGE But not for Breast Imaging…. Here’s Why…. Reporting: The No Hedging Zone • BI-RADS: Reporting: The No Hedging Zone • BI-RADS: BREAST IMAGING-REPORTING AND DATA SYSTEM Reporting: The No Hedging Zone • BI-RADS: BREAST IMAGING-REPORTING AND DATA SYSTEM • System which includes a standardized format and lexicon designed to guide patient care and improve physician communication. Reporting: The No Hedging Zone • BI-RADS: BREAST IMAGING-REPORTING AND DATA SYSTEM • System which includes a standardized format and lexicon designed to guide patient care and improve physician communication. • BI-RADS includes specifics for mammography, ultrasound and MRI reporting. Reporting: The No Hedging Zone • BI-RADS: BREAST IMAGING-REPORTING AND DATA SYSTEM • System which includes a standardized format and lexicon designed to guide patient care and improve physician communication. • BI-RADS includes specifics for mammography, ultrasound and MRI reporting. • ALL breast imaging should be performed according to BI-RADS guidelines BI-RADS reporting must include: BI-RADS reporting must include: • Patient name and identifier BI-RADS reporting must include: • Patient name and identifier • Date of exam BI-RADS reporting must include: • Patient name and identifier • Date of exam • Name of interpreting physician BI-RADS reporting must include: • • • • Patient name and identifier Date of exam Name of interpreting physician Overall final assessment with BI-RADS# (0-6) BI-RADS reporting must include: • • • • • Patient name and identifier Date of exam Name of interpreting physician Overall final assessment with BI-RADS# (0-6) A written report must be sent to the ordering provider and a report in lay terms sent to the patient within 30 days BI-RADS reporting must include: • • • • • Patient name and identifier Date of exam Name of interpreting physician Overall final assessment with BI-RADS# (0-6) A written report must be sent to the ordering provider and a report in lay terms sent to the patient within 30 days • Suspicious findings should be communicated to the ordering physician within 3 business days and to the patient within 5 days Report format • Date, clinical history and indication for study (At PBCC we also include the patient’s estimated risk: IBIS) • Comparison studies • Technique used • Description of breast density in BI-RADS terms • Imaging findings using BI-RADS lexicon • Final assessment with BI-RADS number and recommendations for follow-up BI-RADS CATEGORIES: 1-6 • • • • BI-RADS: 0. FURTHER EVALUATION OR PRIORS NEEDED BI-RADS: 1. NEGATIVE BI-RADS: 2. BENIGN FINDINGS BI-RADS: 3. PROBABLY BENIGN (implies <2% chance of malignancy) • BI-RADS: 4. SUSPICIOUS OF MALIGNANCY (requires biopsy. May be subdivided as A,B,C: low, intermediate, moderate) • BI-RADS: 5. HIGHLY SUSPICIOUS (requires biopsy. Implies 95% likelihood of malignancy) • BI-RADS: 6. KNOWN MALIGNANCY (prior to treatment) BI-RADS CATEGORIES: 1-6 • • • • BI-RADS: 0. FURTHER EVALUATION OR PRIORS NEEDED BI-RADS: 1. NEGATIVE BI-RADS: 2. BENIGN FINDINGS BI-RADS: 3. PROBABLY BENIGN (implies <2% chance of malignancy) • BI-RADS: 4. SUSPICIOUS OF MALIGNANCY (requires biopsy. May be subdivided as A,B,C: low, intermediate, moderate) • BI-RADS: 5. HIGHLY SUSPICIOUS (requires biopsy. Implies 95% likelihood of malignancy) • BI-RADS: 6. KNOWN MALIGNANCY (prior to treatment) BI-RADS CATEGORIES: 1-6 • • • • BI-RADS: 0. FURTHER EVALUATION OR PRIORS NEEDED BI-RADS: 1. NEGATIVE BI-RADS: 2. BENIGN FINDINGS BI-RADS: 3. PROBABLY BENIGN (implies <2% chance of malignancy) • BI-RADS: 4. SUSPICIOUS OF MALIGNANCY (requires biopsy. May be subdivided as A,B,C: low, intermediate, moderate) • BI-RADS: 5. HIGHLY SUSPICIOUS (requires biopsy. Implies 95% likelihood of malignancy) • BI-RADS: 6. KNOWN MALIGNANCY (prior to treatment) BI-RADS CATEGORIES: 1-6 • • • • BI-RADS: 0. FURTHER EVALUATION OR PRIORS NEEDED BI-RADS: 1. NEGATIVE BI-RADS: 2. BENIGN FINDINGS BI-RADS: 3. PROBABLY BENIGN (implies <2% chance of malignancy) • BI-RADS: 4. SUSPICIOUS OF MALIGNANCY (requires biopsy. May be subdivided as A,B,C: low, intermediate, moderate) • BI-RADS: 5. HIGHLY SUSPICIOUS (requires biopsy. Implies 95% likelihood of malignancy) • BI-RADS: 6. KNOWN MALIGNANCY (prior to treatment) BI-RADS CATEGORIES: 1-6 • • • • BI-RADS: 0. FURTHER EVALUATION OR PRIORS NEEDED BI-RADS: 1. NEGATIVE BI-RADS: 2. BENIGN FINDINGS BI-RADS: 3. PROBABLY BENIGN (implies <2% chance of malignancy) • BI-RADS: 4. SUSPICIOUS OF MALIGNANCY (requires biopsy. May be subdivided as A,B,C: low, intermediate, moderate) • BI-RADS: 5. HIGHLY SUSPICIOUS (requires biopsy. Implies 95% likelihood of malignancy) • BI-RADS: 6. KNOWN MALIGNANCY (prior to treatment) BI-RADS CATEGORIES: 1-6 • • • • BI-RADS: 0. FURTHER EVALUATION OR PRIORS NEEDED BI-RADS: 1. NEGATIVE BI-RADS: 2. BENIGN FINDINGS BI-RADS: 3. PROBABLY BENIGN (implies <2% chance of malignancy) • BI-RADS: 4. SUSPICIOUS OF MALIGNANCY (requires biopsy. May be subdivided as A,B,C: low, intermediate, moderate) • BI-RADS: 5. HIGHLY SUSPICIOUS (requires biopsy. Implies 95% likelihood of malignancy) • BI-RADS: 6. KNOWN MALIGNANCY (prior to treatment) BI-RADS CATEGORIES: 1-6 • • • • BI-RADS: 0. FURTHER EVALUATION OR PRIORS NEEDED BI-RADS: 1. NEGATIVE BI-RADS: 2. BENIGN FINDINGS BI-RADS: 3. PROBABLY BENIGN (implies <2% chance of malignancy) • BI-RADS: 4. SUSPICIOUS OF MALIGNANCY (requires biopsy. May be subdivided as A,B,C: low, intermediate, moderate) • BI-RADS: 5. HIGHLY SUSPICIOUS (requires biopsy. Implies 95% likelihood of malignancy) • BI-RADS: 6. KNOWN MALIGNANCY (prior to treatment) BI-RADS CATEGORIES: 1-6 • • • • BI-RADS: 0. FURTHER EVALUATION OR PRIORS NEEDED BI-RADS: 1. NEGATIVE BI-RADS: 2. BENIGN FINDINGS BI-RADS: 3. PROBABLY BENIGN (implies <2% chance of malignancy) • BI-RADS: 4. SUSPICIOUS OF MALIGNANCY (requires biopsy. May be subdivided as A,B,C: low, intermediate, moderate) • BI-RADS: 5. HIGHLY SUSPICIOUS (requires biopsy. Implies 95% likelihood of malignancy) • BI-RADS: 6. KNOWN MALIGNANCY (prior to treatment) BI-RADS Bottom Line BI-RADS Bottom Line • BI-RADS: 1 and 2. No action needed BI-RADS Bottom Line • BI-RADS: 1 and 2. No action needed • BI-RADS: 3. Short term follow-up, usually in 6 months or consider biopsy (decision may be based on patient’s preference) BI-RADS Bottom Line • BI-RADS: 1 and 2. No action needed • BI-RADS: 3. Short term follow-up, usually in 6 months or consider biopsy (decision may be based on patient’s preference) • BIRADS: 4 and 5. Take action. Needs biopsy Sample Report RIGHT BREAST DIGITAL DIAGNOSTIC MAMMOGRAM CLINICAL HISTORY: Asymptomatic 41 year old female seen for diagnostic evaluation of a spiculated mass in the right breast 3:00 location noted on today's baseline screening mammography. She has a history of bilateral breast augmentation mammoplasty in March, 2006. The patient has the following family history of breast cancer: great aunt, Maternal. IBIS estimated lifetime risk 15% TECHNIQUE: Digital mammographic images were obtained using a Selenia mammographic system. Standard and/or additional views were obtained as deemed necessary. MAMMOGRAM FINDINGS: Magnification views of the right breast demonstrate a spiculated mass 2 cm from the nipple at the 3:00 position, middle depth with 2 associated punctate calcifications at the anterior inferior margin. The mass measures approximately 15 x 15 x 20 mm. There is associated architectural distortion. No additional mass, calcification or architectural distortion is seen to suggest malignancy. IMPRESSION: BI-RADS 5. Highly suspicious. Same day ultrasound is pending and if visualized, ultrasound core biopsy will be performed. lf not visualized on ultrasound, stereotactic core biopsy is recommended. ACR BI-RADS Category 5 - Highly Suggestìve of Malignancy. Electronically signed by Freddie Combs. M.D. on 03127/2014 Breast Density, what’s up with that? Breast Density, what’s up with that? • California SB-1538 (2012) requires a written report notifying patients of their breast density. Many states have similar laws • Dense breast tissue decreases mammographic sensitivity and may be an independent risk factor for breast cancer • Currently no formal recommendation for additional testing in dense breasts. Should be individual decision made with their health care provider BI-RADS Breast Density Types • Type 1: “Almost Entirely Fat” or “Mostly Fatty Replaced” (0-25%) BI-RADS Breast Density Types • Type 1: “Almost Entirely Fat” or “Mostly Fatty Replaced” (0-25%) • Type 2: “Scattered Fibroglandular” (25-50%) BI-RADS Breast Density Types • Type 1: “Almost Entirely Fat” or “Mostly Fatty Replaced” (0-25%) • Type 2: “Scattered Fibroglandular” (25-50%) • Type 3: “Heterogeneously Dense”. (50-75%) BI-RADS Breast Density Types • Type 1: “Almost Entirely Fat” or “Mostly Fatty Replaced” (0-25%) • Type 2: “Scattered Fibroglandular” (25-50%) • Type 3: “Heterogeneously Dense”. (50-75%) • Type 4: “Extremely Dense” (>75%) Breast Density Images Our Approach at PBCC to Screening • Patient History • Risk Assessment (IBIS)-Lifetime Risk (LTR) Low Risk: 0-11% Intermediate Risk: 12-19% High Risk: 20%+ • Assess Breast density on screening mammogram PBCC Screening Protocol Low Risk Intermediate Risk High Risk (0-11%) (12-19%) (20%+) • Mammogram • Mammogram • Screening US if Dense Breasts • Mammogram • Screening MRI • Screening US if can’t have MRI Summary Summary • Breast Cancer is a common but mostly treatable disease Summary • Breast Cancer is a common but mostly treatable disease • Screening is the key to early diagnosis but only works if patients trust that it is safe and effective (and it is!) Summary • Breast Cancer is a common but mostly treatable disease • Screening is the key to early diagnosis but only works if patients trust that it is safe and effective (and it is!) • It is our job to: Educate patients, order appropriate imaging, provide consistent follow-up and communicate. Summary • Breast Cancer is a common but mostly treatable disease • Screening is the key to early diagnosis but only works if patients trust that it is safe and effective (and it is!) • It is our job to: Educate patients, order appropriate imaging, provide consistent follow-up and communicate. • This is a team effort! What’s best for your patients? • MQSA/ACR certified breast center What’s best for your patients? • MQSA/ACR certified breast center • Digital imaging preferred What’s best for your patients? • MQSA/ACR certified breast center • Digital imaging preferred • Experienced Radiologists and Techs What’s best for your patients? • • • • MQSA/ACR certified breast center Digital imaging preferred Experienced Radiologists and Techs Evidence based imaging protocols What’s best for your patients? • • • • • MQSA/ACR certified breast center Digital imaging preferred Experienced Radiologists and Techs Evidence based imaging protocols Timely reporting to physicians using BI-RADS format and easy to understand patient information Get to know your Breast Imagers Get to know your Breast Imagers • Breast cancer is a complex disease on many levels with many gray areas in screening and diagnosis. We owe it to our patients to work together to provide consistent information Get to know your Breast Imagers • Breast cancer is a complex disease on many levels with many gray areas in screening and diagnosis. We owe it to our patients to work together to provide consistent information • Even basic screening can be terrifying to patients. Sometimes the most important service we provide is REASSURANCE THANK YOU! Mammography: • Swedish Two-County Trial, a landmark study started in 1977 demonstrated a 31% reduction in mortality and 25% reduction in Stage II or later cancers. (1977-84) Tabár L, Vitak B, Chen TH, et al.. Swedish two-county trial: impact of mammography screening on breast cancer mortality during 3 decades. Radiology 2011;260(3):658–663.