Quality of Care and Patient Satisfaction Today Israel De Alba, MD MPH
advertisement

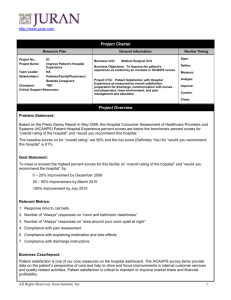
Quality of Care and Patient Satisfaction Today Israel De Alba, MD MPH Clinical Professor Hospitalist Program Content Quality of care today. Why? How? The patients’ perspective The doctors’ perspective Summary and conclusions Aims To provide an updated perspective on factors that impact quality of medical care and patient satisfaction in the era of health care reform. To review data on physician satisfaction CC: failure to thrive US health care system • 1 million physicians • 20 million health care workers • 5000 hospitals • 315 million patients The traditional model for practicing medicine in the United States has been obsolete for the past 40 years Ideal health care Real health care? Future of health care in the US? Current challenges needed change but… 1. Payment restructuring (ACA, from fee-for-service to restricted compensation based on outcomes) • Bundled payments for services • Payment for episode of care (specific condition for a specific period) • Physician Quality Reporting System and reimbursement based on metrics • Shared savings programs 2. Policy changes • ICD 10 the use of the International Classification of Diseases • Meaningful Use incentive program (MU2) for electronic health records (EHRs) • Accountability Act (HIPAA) • Physician Quality Reporting System (PQRS) (reporting on 138 outcome quality measures) Current challenges 3. Time for seeing patients • Finding time for patients despite escalating administrative noise 4. Rising cost to implement changes • Implementation of e-medical records and training of staff 5. Changing requirements for recertification 6. Oversight by multiple agencies: insurance companies, policy makers, government agencies, patients 7. Health information revolution 8. Emphasis on disease rather than on prevention Quality of care (Institute of Medicine) Safe Avoiding injuries to patients from the care that is supposed to help them. Effective Based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding underuse and overuse). Patient-centered Respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions. Timely Reducing waits and sometimes harmful delays for both those who receive and those who give care. Efficient Avoiding waste, in particular waste of equipment, supplies, ideas, and energy. Equitable Care that does not vary in quality because of personal characteristics, such as gender, ethnicity, geographic location, and socioeconomic status. How are we doing? Change over time Safety slight improvement 2011: National overall HAC rate: 142 per 1,000 hospital discharges. 2010: National overall HAC rate 145 per 1,000 hospital discharges Variation by state, race/ethnicity, SES *HAC: Hospital Acquired Conditions Timeliness • Time spent waiting in doctors’ offices, ED • Interval between identifying a need and receiving the service Outcomes in National Health Quality Report • ◆ Getting care for illness or injury as soon as wanted. • ◆ ED waiting times. • ◆ Timeliness of cardiac reperfusion for heart attack patients. Timeliness Patient centeredness Outcomes ◆ Patients who reported poor communication at the doctor’s office ◆ Adults who reported poor communication with nurses and doctors at the hospital. ◆ Provider-patient communication among adults receiving home health care. ◆ Provider’s involvement of the patient in making treatment decisions. Patient centeredness Patient centeredness HCAHPS: patient experience • Medicare & Medicaid Services (CMS) • 27-item survey instrument • First, national and standardized survey • Allow objective comparisons of hospitals • Public reporting creates new incentives for hospitals to improve quality of care • Reporting enhances accountability HCAHPS HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey is the first national, standardized, publicly reported survey of patients' perspectives of hospital care. Contains 18 core questions communication with nurses and doctors responsiveness of hospital staff the cleanliness and quietness of the hospital environment pain management communication about medicines discharge information overall rating of hospital would they recommend the hospital HCAHPS • 2% deduction if no reporting • HCAHPS is used in the calculation of the value-based incentive payment in the Hospital Value-Based Purchasing program • Random sample of adult inpatients between 48 hours and six weeks after discharge • Survey modes: mail, telephone, mail with telephone followup, or active interactive voice recognition (IVR) HCAHPS • English, Spanish, Chinese, Russian and Vietnamese versions HCAHPS UCIMC PatientsPerspective How patients define quality? What matters to patients? Funded: RWJ. N=1000, RDD during June 2014 PatientsPerspective What is quality? PatientsPerspective When choosing a physician? PatientsPerspective How do you rate quality of care? Funded: RWJ N = 1034 adults National, phone • N= 10,000 physicians • Telephone • Only physicians with >20 hours/week • Response rate: 52%, 40%, 67% Time with patient Freedom decisions High QoC to all Job Satisfied US 29% 55% 79% 84% Canada 7% 10% 46% 90% Norway 7% 12% 59% 90% • N= 7288 • American Medical Association Physician Masterfile and surveyed a probability-based sample of the general US population for comparison • Maslach Burnout Inventory Burnout and Satisfaction • 45.8% of physicians reported at least 1 symptom of burnout • Highest rates among physicians at the front line (family medicine, general internal medicine, and emergency medicine) • Compared with working US adults, physicians were more likely to: • Have symptoms of burnout • Be dissatisfied with work-life balance (40.2% vs 23.2%) (P < .001 for both) Burnout and Satisfaction • Highest level of education also related to burnout in multivariate analysis adjusted for age, sex, relationship status, and hours worked per week • Compared with high school graduates, MD or DO degree were at increased risk for burnout (odds ratio [OR], 1.36; P < .001) • Whereas individuals with a bachelor's degree (OR, 0.80; P = .048), master's degree (OR, 0.71;P = .01), or professional or doctoral degree other than an MD or DO degree (OR, 0.64; P = .04) were at lower risk for burnout. Across the world Burnout by specialty Good news Physician satisfaction/wellness missing form the quality of care picture Summary and Conclusions Quality medical care must be safe, effective, timely, efficient, equitable and patient centered The US healthcare system is undergoing needed major structural changes that deeply impact quality of care, patients perceptions and physician satisfaction Patient centeredness is a key component of quality of care Physician satisfaction/wellbeing should also be considered as a marker of quality of care