INITIAL MANAGEMENT OF SUSPECTED BACTERIAL MENINGITIS Stephanie Singson PGY2
advertisement
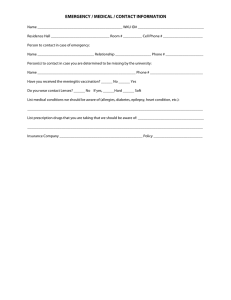
INITIAL MANAGEMENT OF SUSPECTED BACTERIAL MENINGITIS Stephanie Singson PGY2 Case Mr. B is a 70 year old M evaluated in the ED for a 1-day history of fever and altered mental status. PMH is notable for CAD and HTN on HCTZ, ASA, Lisinopril, and Atenolol. On physical exam, T 38.3C (101F), BP 96/52, HR 101/min, RR 20/min. Patient is confused and oriented only to person. Neurologic exam is nonfocal. Objectives Identify patient Initial presentation Signs of meningeal irritation Diagnostics Role of CT LP: CSF Analysis Microbiology review Treatment Antibiotic regimen Role of steroids Initial Presentation Triad of fever, nuchal rigidity, change in mental status. In a 2004 review of >600 cases, only 44% had the clinical triad. 99% had at least one classic feature. Other common complaints include headache, nausea, vomiting and photophobia. Physical Exam: Signs of Meningeal Irritation Brudzinski sign: Involuntary flexion of the hips with neck flexion. Kernig sign: Resistance with knee extension. Patient is supine, with hip and knee flexed to about 90 degrees. Studies report a wide range of sensitivities for both tests (5-39%) although specificity is high >95%. To CT or Not to CT? Based on IDSA guidelines for 2004, a CT scan of the head before LP should be done in patients who have one or more risk factors: Immunocompromised state History of CNS disease New onset seizure Papilledema Abnormal level of consciousness Focal neurological deficit LP: CSF Analysis Opening pressure: 200-500 mm H2O WBC count: 1000-5000/microL with a percentage of neutrophils >80% Protein: 100-500mg/dL Glucose: <40mg/dL Gram stain and culture The Usual Suspects Major causes of community acquired bacterial meningitis in developed countries: Streptococcus pneumoniae Neisseria meningitidis Listeria monocytogenes in patients >50 years old or who have deficiencies in cell-mediated immunity The Usual Suspects cont. Major causes of healthcare-associated bacterial meningitis: Staphylococci Aerobic gram-negative bacilla (Pseudomonas, Klebsiella) Initial Treatment: Community Acquired • Vancomycin 15-20mg/kg IV q8-12h • • PLUS Third generation Cephalosporin (Ceftriaxone 2g IV q12h or Cefotaxime 2g IV q4-6h ) • • Adjust to achieve trough of 15-20mcg/mL Note: Increased dose of Cephalosporin compared to standard antibiotic dose ADD Ampicillin 2g IV q4h to cover Listeria Initial Treatment: Healthcare-associated • Vancomycin 15-20mg/kg IV q8-12h • • • Adjust to achieve trough of 15-20mcg/mL PLUS Cefepime 2g IV q8h OR Meropenem 2g IV q8h to cover Pseudomonas aeruginosa and Klebsiella pneumoniae Think recent neurosurgery, complicated head trauma Role of Steroids Adjunct Dexamethasone 0.15mg/kg IV q6h to prevent neurologic complications given before or at the same time as the first dose of antibiotics (Grade 1B). Suspected bacterial meningitis Fever, nuchal rigidity, AMS Obtain blood cultures, head CT (if indicated), lumbar puncture Community acquired Recent neurosurgery Complicated head trauma Dexamethasone 0.15mg/kg IV q6h Vancomycin + Ceftriaxone or Cefotaxime +/Ampicillin Vancomycin + Cefepime or Meropenem (For Pseudomonas and Klebsiella coverage) (Age >50 or immunocomrpomised ) Await culture results for targeted therapy Back to the Case: Mr. B is a 70 year old M evaluated in the ED for a 1-day history of fever and altered mental status. PMH is notable for CAD and HTN on HCTZ, ASA, Lisinopril, and Atenolol. On physical exam, T 38.3C (101F), BP 96/52, HR 101/min, RR 20/min. Patient is confused and oriented only to person. Neurologic exam is nonfocal. How would you manage Mr. B? Non-contrast head CT Indication: Abnormal level of consciousness Result: Negative for bleed or acute abnormality Draw blood cultures. Perform LP. Result: Opening pressure 300 mmH2O Leukocyte count 1200/uL 60% neutrophils, 40% lymphocytes Glucose level 30mg/dL Protein level 350mg/dL Gram stain negative Administer: Dexamethasone, Vancomycin, Ceftriaxone, and Ampicillin (Age> 50) Await culture results to titrate antibiotic regimen and determine duration of treatment Summary Consider bacterial meningitis in a patient with fever and AMS, with or without signs of meningeal irritation. Consider head CT before LP based on IDSA recommendations. Perform blood cultures and LP prior to administering IV antibiotics. Administer Dexamethasone with first dose or prior to IV antibiotics. Mortality rate of untreated disease approaches 100%. References LeBlond RF, Brown DD, Suneja M, Szot JF. The Nervous System. In: LeBlond RF, Brown DD, Suneja M, Szot JF. eds. DeGowin’s Diagnostic Examination, 10e. New York, NY: McGraw-Hill; 2014. http://accessmedicine.mhmedical.com. Accessed February 22, 2015. Roos KL, Tyler KL. Chapter 381. Meningitis, Encephalitis, Brain Abscess, and Empyema. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson J, Loscalzo J. eds. Harrison's Principles of Internal Medicine, 18e. New York, NY: McGraw-Hill; 2012. http://accessmedicine.mhmedical.com. Accessed February 20, 2015. Thomas KE, Hasbun R, Jekel J, Quagliarello VJ. The diagnostic accuracy of Kernig's sign, Brudzinski's sign, and nuchal rigidity in adults with suspected meningitis. Clin Infect Dis 2002; 35:46. Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 2004; 39:1267. www.uptodate.com