Low Back Pain Elizabeth Chang, MD PGY-2
advertisement

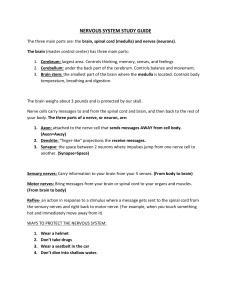
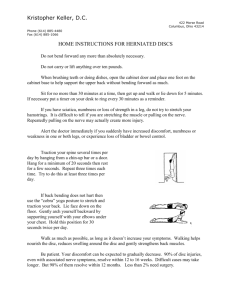
Low Back Pain Elizabeth Chang, MD PGY-2 46 yo male p/w LBP x 6 mo - Started 6 mo. ago while lifting boxes at his delivery job - Located middle of lower back, radiates to right buttock and right lateral aspect of right foot - Pain worsened with sneezing/coughing - Difficult to stand on tip toes - Absent right ankle jerk - Straight leg test, cannot elevate right leg above 35 degrees - No urinary/bowel incontinence, fevers, weight loss - Otherwise healthy “Fun” Facts • • • • • #2 reason patients show up in your office 84% of adults in US have LBP at some point Up to 85% no definitive cause found Costs the economy $100 BILLION per year Substantial impact on lifestyle and quality of life • <5% have serious systemic pathology Differential for LBP Red Flags • • • • • • • • • History of cancer Age > 50 Unexplained weight loss Symptoms of neurological compromise Pain lasting >3 mo. Nighttime pain Unresponsiveness to previous therapies History of AAA Risk factors for spinal infection (HIV, IVDA, etc) Radiological/Anatomic Spondylosis: arthritis of the spine – disc space narrowing, arthritic changes in joint facet Spondylolisthesis: anterior displacement of a vertebra on the one beneath it. Graded I – IV Sponylolysis: fracture in the pars interarticularis that protects the nerve Spinal stenosis: narrowing of the central spinal canal (bony enlargement or thickened ligamentum flavum). Shopping cart sign. Ankylosing Spondylitis • Chronic inflammatory disease of axial skeleton • Sacroiliac joint involvement, bamboo spine on imaging • Males, 20-30s, HLA-B27 • Dull vague stiffness, slowly progressive over years, worse at night, better with light activity • Elevated ESR, CRP • No cure, conservative management Physical Lumbar lordosis – inward curve Kyphosis – outward curve Scoliosis – sideways curve (always abnormal) Neurologic Radiculopathy – impairment of nerve root causing radiating pain, numbness/tingling, muscle weakness corresponding to specific nerve root. Most often herniated disc. Worsened with bending over. • Sciatica – set of symptoms, not a dx – compression/irritation of one of the 5 spinal roots – affects posterior/lateral aspect of leg to the foot/ankle Cauda Equina Syndrome • Saddle anesthesia • Recent onset bladder dysfunction • Severe or progressive neurologic deficit in lower extremity Surgery Classifications • Acute: <4 weeks – Excellent prognosis, 90% full recovery • Subacute: 4-12 weeks • Chronic: >12 weeks The Physical Exam 1 The Physical Exam 2 • Reflexes – Achilles tests S1 nerve root – Patellar tests L4 – Upgoing toes may indicate upper motor neuron instead • Straight Leg Test (for sciatic nerve irritation) – Pain below knee at <70 degrees worsened by ankle dorsiflexion suggests L5/S1 tension from disc herniation • Sitting Knee Extension Test – Should reproduce any findings from the SLT, helps clinician discover inconsistent findings Non-pharmacological treatments • Exercise/PT/OT – Proven modest benefits in subacute/chronic LBP – Yoga, pilates, tai chi • Spinal manipulation – Serious adverse effects rare (<1/1,000,000) • Acupuncture • Massage • TENS (transcutaneous electrical nerve stimulation) – large study showed no difference 1st Line Pharmacotherapy • NSAIDS – Ibuprofen 400-600 mg QID or Naproxen 220-550 mg BID or IM ketoralac 60 mg (ER) – Caution in elderly, nephrotoxic, GI • Acetaminophen as alternative – Max 4g/day – Hepatotoxicity risk Centrally-acting skeletal muscle relaxants • Limit use to 3 weeks • Anti-cholinergic side effects – Cyclobenzaprine – Methocarbamol – Carisoprodol • Baclofen • Benzos – less evidence supporting efficacy, high risk abuse Opioids • Norco, percocet, MS Contin • Tramadol – non-opioid that acts on opioid receptors • Sedation, confusion, nausea, constipation, respiratory depression in high doses • Misuse and abuse (30-45%) – scheduled rather than prn • Short-term only Anti-depressants & Anti-epileptics • Tricyclics (amitriptyline) – Drowsiness, dry mouth, dizziness • Radiculopathic pain – Gabapentin, pregabalin, topiramate Glucocorticoids • Limited data on efficacy and safety • Not recommended The End