Maternal Depression Associated with Less Healthy Dietary Behaviors in Young Children
advertisement

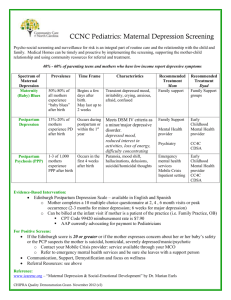
INCOME AND BENEFITS POLICY CENTER BRIEF Maternal Depression Associated with Less Healthy Dietary Behaviors in Young Children Tracy C. Vericker February 2015 Maternal depression threatens the well-being of millions of children in the United States: one out of five women with at least one child suffered from depression in 2002 (NRC and IOM 2009). Maternal depression can interfere with positive parenting practices, many of which may have lasting developmental consequences for children. Maternal depression or depressive symptoms are associated with such negative parenting behaviors as shortened duration of breastfeeding, fewer well-child visits, neglect, psychological aggression, and physical assault. 1 Maternal depression’s effects on parenting can have long-reaching harmful effects on children and 2 may damage their cognitive, social, and emotional development. Mothers’ depressive symptoms and depression have also been linked to children’s internalizing and externalizing behavior problems throughout childhood and adolescence, and they may jeopardize a child’s own mental health in 3 adulthood. Maternal depression may also affect children’s physical health, particularly their risk of childhood 4 obesity. Many obese children become obese adults and are burdened by adverse health conditions, 5 including type II diabetes, hypertension, and certain forms of cancer. The medical costs associated with adult obesity may be as high as $209.7 billion a year (in 2005 dollars)—20.6 percent of total US health care expenditures (Cawley and Meyerhoefer 2012). While private payers bear most of the burden of obesity costs, the taxpayer burden is nontrivial: if adult obesity were eliminated, spending on Medicare and Medicaid could be 8.5 percent and 11.8 percent lower, respectively (Finkelstein et al. 2009). The link between maternal depression or depressive symptoms and childhood obesity may be a result of poor eating habits, though evidence is scant. Duarte and colleagues (2012) find that severe maternal depression symptoms at different points during childhood are associated with high body mass index (BMI) z-scores for children in fifth grade; among boys, fewer healthy eating practices may mediate the relationship between maternal depressive symptoms in kindergarten and BMI in fifth grade. This research builds on the work of Duarte and colleagues by investigating the relationship between maternal depression and eating habits earlier in childhood, when food preferences are developing. Specifically, this research asks if maternal depression is associated with poor dietary behaviors in young children. Data, Measures, and Analyses The data for this study come from the Early Childhood Longitudinal Survey–Birth Cohort (ECLS-B), a nationally representative survey of 14,000 infants born in 2001, administered by the Department of 6 Education. This study uses data from the fourth round of the survey in 2006, when focal children were approximately 5 years old, yielding a sample of 5,100. The ECLS-B is a complex survey design, sampling children from both primary and secondary sampling units. To account for this complexity, all analyses include sampling weights to account for clustering, and the Survey procedures in SAS 9.2 are used to adjust standard errors. Sample sizes are rounded to the nearest 50, per disclosure requirements of the National Center for Education Statistics. The presence of maternal depressive symptoms is measured using data from the 2006 parent interview and is based on mothers’ responses to a modified version of the Center for Epidemiologic Studies Depression Scale, or CES-D (Radloff 1977). The CES-D is a commonly used scale that measures the frequency of depressive symptoms during the prior week. It is not equivalent to a clinical diagnosis of depression. The cut points used to identify the presence and severity of depressive symptoms (mild, moderate, and severe) are provided in the CES-D user’s manual (Nord et al. 2004). Measures of children’s dietary behaviors are also drawn from the 2006 parent interview. Parents are asked how often their children consumed fruits, vegetables, milk, sweet snacks, salty snacks, fast food, and sweetened beverages (e.g., sports drinks, fruit drinks, soda) over the past seven days. Responses to these questions are used to develop seven continuous outcome measures of the number of times a child consumed these foods and beverages over seven days. Responses are also recoded to examine whether children consume these foods and beverages every day. Bivariate analyses are used to examine differences in characteristics of children, mothers, and households between children whose mothers report depressive symptoms and children whose mothers do not. Chi-square tests are used to measure statistically significant differences in dichotomous variables, and t-tests are used to measure differences in continuous measures. The associations between the presence of maternal depressive symptoms and children’s dietary behaviors are assessed using ordinary least squares models with rich covariates; logistic regression is used to estimate models with dichotomous outcome measures. All models account for the following characteristics: child’s gender; mother’s race/ethnicity; presence of two biological parents in the household; number of children under age 18 in the household; mother’s age at first birth; mother’s fulltime employment status; if household income is below 185 percent of the poverty level; level of mother’s social support; if child has had a well-child visit since the last interview; if child spends time in a 2 MATERNAL DEPRESSION AND DIET QUALITY child care arrangement each week; if child attends kindergarten; and if child participated in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) up to his or her fifth birthday. Prevalence and Severity of Maternal Depression More than one-third (38 percent) of kindergarten-age children in the sample have a mother who has recently experienced depressive symptoms; the prevalence of maternal depressive symptoms is significantly higher in low-income households—those with incomes less than 185 percent of the poverty level—than in higher-income households (46 percent versus 32 percent; see figure 1). Among mothers with depressive symptoms, many (38 percent) experience moderate to severe symptoms, though most (62 percent) experience mild depressive symptoms. The presence of moderate to severe maternal depressive symptoms is also more common in low-income households than in higher-income households: 46 percent versus 30 percent. FIGURE 1 Prevalence of Depressive Symptoms among Mothers of Kindergarten-Age Children by Income, 2006 (%) Mild symptoms Moderate to severe symptoms 45.9 38.2 21.0 32.3 14.5 9.6 23.7 24.9 22.7 All children < 185% of poverty level ≥ 185% of poverty level Source: Tabulations derived from the fourth round of the 2001 Early Childhood Longitudinal Study–Birth Cohort (ECLS-B). Notes: Tabulations are weighted to be nationally representative of children born in 2001. The sample is 5,100 kindergarten-age children in 2006. Per National Center for Education Statistics guidelines, unweighted samples have been rounded to the nearest 50. Maternal depression is measured using mothers’ responses to a modified version of the Center for Epidemiologic Studies Depression Scale. The cut points used to identify symptom severity are from the user’s manual for the ECLS-B (Nord et al. 2004). MATERNAL DEPRESSION AND DIET QUALITY 3 Thirty-eight percent of kindergarten-age children have a mother who has recently experienced depressive symptoms; such symptoms are significantly more prevalent in lowincome households than in higher-income households (42 percent versus 32 percent). Characteristics of Mothers, Households, and Kindergarten-Age Children Mothers of kindergarten-age children who experience depressive symptoms are more likely to have characteristics associated with disadvantage than their peers without depressive symptoms (table 1). Compared with mothers who do not exhibit depressive symptoms, mothers who exhibit depressive symptoms are more likely to have had children before age 18, live without their child’s biological father, not complete high school, and live in a low-income household. Mothers with depressive symptoms also report worse health outcomes than their peers who do not report depressive symptoms. Mothers with depressive symptoms are more likely to report fair to poor health, experience household food insecurity, and binge drinking. Social isolation is also associated with depressive symptoms. These mothers have fewer resources available when they need help with such activities as getting their children to the doctor or accessing cash for an emergency. Mothers with depressive symptoms use more negative discipline with their children. More than half (52 percent) report spanking their children, compared with 41 percent of mothers without depressive symptoms. More than one-third (34 percent) of mothers with depressive symptoms report hitting, making fun of, or yelling or threatening their children, compared with 27 percent of mothers without depressive symptoms. Despite these challenges, mothers with depressive symptoms interact with several service systems. One in three of these mothers lives in a household receiving Supplemental Nutrition Assistance Program (SNAP) assistance, and nearly one in five (18 percent) reports that her child received benefits from WIC up to age 5. Nearly all mothers report that their children are insured (95 percent), many by Medicaid (38 percent). Most (93 percent) report that their kindergarten-age child has had a well-child check-up since their last interview. The majority of their children (72 percent) attend kindergarten, and many (52 percent) spend some time in a child care arrangement in a typical week. Yet, few mothers reporting depressive symptoms receive help for their depression. Roughly onefifth (22 percent) of mothers reporting depressive symptoms have spoken with a professional about psychological health problems in the past 12 months, and fewer (13 percent) have taken medication for these problems. 4 MATERNAL DEPRESSION AND DIET QUALITY TABLE 1 Characteristics of Mothers, Households, and Kindergarten-Age Children by Presence of Maternal Depressive Symptoms Characteristic Depressive symptoms reported (n = 2,050) No depressive symptoms reported (n = 3,050) Maternal/household characteristics Mother's race/ethnicity (%) White, non-Hispanic Black, non-Hispanic Hispanic Other Two biological parents in the household (%) Number of children under age 18 in the household Mother's age at first birth (%) < 18 18–24 25 or older Mother employed full-time (%) Highest level of education of parents in the household (%) Less than high school High school Some college or technical training Bachelor's degree or higher Household lives below 185% of the poverty level (%) Someone in household received SNAP benefits last year (%) Discipline methods (%) Spank Hit back, make fun of, or yell or threaten child 57.0 17.1 20.1 5.8 61.9 2.6 60.5* 11.7** 22.6 5.2 76.8** 2.5 15.4 50.0 34.6 41.9 10.4** 43.0** 46.6** 43.4 11.9 26.2 32.9 29.0 52.4 33.1 7.7** 23.4 30.1 38.8** 38.2** 16.9** 51.7 34.2 41.4** 27.0** 14.6 18.5 5.2** 4.2** 21.7 6.4** 12.5 12.9 15.3 4.1** 8.8** 15.9** 94.5 37.7 93.2 51.5 72.1 18.2 96.5** 26.5** 95.9** 52.8** 71.4 14.3** Maternal health (%) Mother in fair or poor health Household is food insecure Mother spoke to a professional about emotional or psychological problems in the last 12 months Mother takes medication daily for anxiety, depression, or other emotional problems Mother had four or more drinks in one sitting in past month a Social support scale (0–18, 0 = no support; mean) Child characteristics Covered by health insurance Covered by Medicaid Had well-child visit since last interview Spends time each week in a child care arrangement Attended kindergarten in 2006 Received WIC benefits up to age 5 Source: Tabulations derived from the fourth round of the 2001 Early Childhood Longitudinal Study-Birth Cohort (ECLS-B). Notes: Tabulations are weighted to be nationally representative of children born in 2001. Per National Center for Education Statistics guidelines, unweighted samples have been rounded to the nearest 50. Maternal depression is measured using mothers’ responses to a modified version of the Center for Epidemiologic Studies Depression Scale. The cut point used to identify presence of depressive symptoms is provided by the user’s manual for the ECLS-B (Nord et al. 2004). a. Respondents were asked to rate their social support systems on a three-point scale (never true, sometimes true, and always true) for six items. Ratings were converted into an 18-point scale, with 0 meaning no support and 18 meaning full support. *p < 0.01., **p < 0.05. MATERNAL DEPRESSION AND DIET QUALITY 5 Associations between Mothers’ Depressive Symptoms and Their Kindergarten-Age Children’s Eating Practices Reported maternal depressive symptoms are associated with poor eating habits, based on bivariate comparisons of the consumption patterns of kindergarten-age children (table 2). Over seven days, children whose mothers report depressive symptoms consume vegetables less often (64 percent every day) than children of mothers reporting no depressive symptoms (67 percent every day); milk less often (14.3 times a week; 81 percent every day) than children of mothers reporting no depressive symptoms (15.0 times a week; 85 percent every day); sweetened beverages more often (5.1 times a week; 33 percent every day) than children of mothers reporting no depressive symptoms (4.1 times a week; 26 percent every day); and sweet snacks more often (6.6 times a week; 49 percent every day) than children of mothers reporting no depressive symptoms (6.0 times a week; 44 percent every day). Though children of mothers with depressive symptoms eat fruit the same number of times each week as children of mothers with no depressive symptoms, children whose mothers report moderate to severe depressive symptoms consume fruit less often than children whose mothers do not report depressive symptoms (9.2 versus 10.1 times a week; data not shown). Consumption of salty snacks and fast food does not differ between children whose mothers report depressive symptoms and those whose mothers do not. Reported maternal depressive symptoms are associated with a number of adverse conditions, particularly low-income status, as shown in table 1. Models controlling for these adverse conditions as well as other possible confounders better assess the relationship between maternal depression and children’s consumption patterns (middle column of table 2). Even after holding these factors constant, all statistically significant bivariate findings remain. Discussion Maternal depression affects the social, emotional, and physical health of many children. This study examines the potential association between maternal depressive symptoms and consumption of healthy and unhealthy foods by kindergarten-age children. Results suggest that many children live with mothers who report depressive symptoms and few of their mothers receive treatment for their symptoms. Mothers with reported depressive symptoms are faced with numerous challenges, including having low income, food insecurity, and weak social support networks. Young children with mothers reporting depressive symptoms consume more unhealthy foods and beverages and fewer healthy foods 6 MATERNAL DEPRESSION AND DIET QUALITY and beverages than children with mothers who do not report depressive symptoms, even after accounting for numerous confounding challenges such as low-income status. Parents play an important role in establishing healthy eating habits for their children early in life (Sealy and Farmer 2011; Ventura and Birch 2008). A mother’s depression, or the challenges that coexist with depression, may interfere with her ability to provide healthy food and beverages for her children and to model healthy eating behaviors, possibly leading to unhealthy eating habits that continue later in her children’s lives. TABLE 2 Consumption Patterns of Kindergarten-Age Children by Presence of Maternal Depressive Symptoms Depressive symptoms reported (n = 2,050) Number of times consumed in previous seven days Fruits Vegetables Mean 9.8 8.9 Milk Sweet snacks Salty snacks Fast food Sweetened beverages 14.3** 6.6** 4.8 2.2 5.1** Consumed every day in the previous seven days Fruits Vegetables Milk Sweet snacks Salty snacks Fast food Sweetened beverages Mean 68.6 63.5* 81.0** 48.9* 33.5 7.2 33.1** a a b OLS estimate (SE) -0.33 (0.275) -0.28 (0.265) -0.76** (0.343) 0.56* (0.308) 0.12 (0.232) 0.07 (0.113) 0.62** (0.239) b Odds ratio (SE) 0.93 (0.337) 0.85* (0.087) 0.77** (0.116) 1.22** (0.097) 1.07 (0.112) 1.03 (0.029) 1.22** (0.201) No depressive symptoms reported (n = 3,050) Mean 10.1 8.9 15.0 6.0 4.5 2.0 4.1 Mean 70.7 67.1 85.4 44.4 30.1 6.9 25.8 Source: Tabulations derived from the fourth round of the 2001 Early Childhood Longitudinal Study-Birth Cohort. Notes: Tabulations are weighted to be nationally representative of children born in 2001. Per National Center for Education Statistics guidelines, unweighted samples have been rounded to the nearest 50. Maternal depression is measured using mothers’ responses to a modified version of the Center for Epidemiologic Studies Depression Scale. The cut points used to identify the presence and severity of depressive symptoms are from the user’s manual for the ECLS-B (Nord et al. 2004). SE = standard error. a. The reference group is no depressive symptoms. b. The model is estimated with the following controls: child’s gender; mother’s race/ethnicity; presence of two biological parents in the household; number of children under age 18 living in the household; mother’s age at first birth; mother’s full-time employment status; if household income is below 185 percent of the poverty level; level of mother’s social support; if child had well-child visit since last interview; if child spends time in a child care arrangement each week; if child attends kindergarten; and if child participated in WIC up to his or her fifth birthday. * p < 0.1; **p < 0.05. MATERNAL DEPRESSION AND DIET QUALITY 7 The link between maternal depression and unhealthy dietary patterns among children may shed important light on the childhood obesity epidemic, a condition that partly stems from diets high in fats and sugars and low in fresh fruits and vegetables and whole grains (Bradlee et al. 2010; Kröller and Warschburger 2009). A mother suffering from a lack of energy, fatigue, or other depression symptoms may feed her children more convenient, but often unhealthy, foods and beverages. Sweetened beverage consumption may be particularly problematic, as some studies have shown a positive association between consumption of sugar-sweetened beverages and child obesity (Grimes et al. 2013; Ludwig, Peterson, and Gortmaker 2001). These unhealthy eating habits are an additional lens to examine the harmful two-generational impact of maternal depression and to provide further motivation to better link depressed mothers to effective treatment. Two limitations of this research are noteworthy. First, this study uses cross-sectional data. While every attempt has been made to control for potential confounding variables in the multivariate analysis, omitted variables may explain the relationship between maternal depression and children’s food and beverage consumption; therefore, results from this research should be cautiously interpreted as associations and not causal effects. Second, because the measure of maternal depression is selfreported symptoms, not a clinical diagnosis of depression, this study likely overstates the number of mothers who are clinically depressed. Conclusions This study provides further evidence that maternal depression may have a damaging effect on the health of children. With so many mothers reporting depressive symptoms and so few receiving treatment, the room for improvement is considerable. In particular, there are opportunities to better serve low-income depressed mothers. Many of these mothers are newly eligible to receive Medicaid coverage under the Patient Protection and Affordable Care Act, opening up the possibility of increasing depression screenings and treatment. Acknowledgments The research upon which this brief is based was funded by the Doris Duke Charitable Foundation. The author is grateful to Olivia Golden and Marla McDaniel for their thoughtful comments and review and to Christopher Lowenstein for his research assistance. 8 MATERNAL DEPRESSION AND DIET QUALITY Notes 1. For breastfeeding, see Dennis and McQueen (2009) and Henderson et al. (2003); for well-child visits, see Minkovitz et al. (2005). For neglect, see Lovejoy et al. (2000) and Turney (2010); for psychological aggression, see Feng et al. (2007); and for physical assault, see Berger (2005) and Silverstein et al. (2009). 2. See, for example, Center on the Developing Child at Harvard University (2009), NRC and IOM (2009), and Kiernan and Huerta (2008). 3. See Turney (2011) and Weissman et al. (2006). 4. See, for example, Wang et al. (2013), Milgrom et al. (2011), and Topham et al. (2010). 5. “Basics about Childhood Obesity,” Centers for Disease Control and Prevention, accessed November 24, 2014, http://www.cdc.gov/obesity/childhood/basics.html. 6. The ECLS-B provides detailed information about the early life experiences of these focal children, following them from birth through kindergarten. Information was collected from parents, child care providers, and teachers as well as from direct assessments of children and home observations conducted by interviewers when the focal children were 9 months, 24 months, 4 years, and 5 years old. Data collection for 5-year-olds occurred in 2006, and a subset of data were collected in 2007 to capture early school experiences of children who did not attend kindergarten in 2006. For more information on the ECLS-B, see Snow et al. (2009). References Berger, L. M. 2005. “Income, Family Characteristics, and Physical Violence toward Children.” Child Abuse and Neglect 29 (2): 107–33. Bradlee, M. L., M. R. Singer, M. M. Qureshi, and L. L. Moore. 2010. “Food Group Intake and Central Obesity among Children and Adolescents in the Third National Health and Nutrition Examination Survey (NHANES III).” Public Health Nutrition 13 (6): 797–805. Cawley, J., and C. Meyerhoefer. 2012. “The Medical Care Costs of Obesity: An Instrumental Variables Approach.” Journal of Health Economics 31 (1): 219–30. Center on the Developing Child at Harvard University. 2009. Maternal Depression Can Undermine the Development of Young Children. Cambridge, MA: Center on the Developing Child at Harvard University. Dennis, C. L., and K. McQueen. 2009. “The Relationship between Infant-Feeding Outcomes and Postpartum Depression: A Qualitative Systematic Review.” Pediatrics 123 (4): 736–51. Duarte, C. S., S. Shen, P. Wu, and A. Must. 2012. “Maternal Depression and Child BMI: Longitudinal Findings from a U.S. Sample.” Pediatric Obesity 7 (2): 124–33. Feng, X., D. S. Shaw, E. M. Skuban, and T. Lane. 2007. “Emotional Exchange in Mother-Child Dyads: Stability, Mutual Influence, and Associations with Maternal Depression and Child Problem Behavior.” Journal of Family Psychology 21 (4): 714–25. Finkelstein, E. A., J. G. Trogdon, J. W. Cohen, and W. Dietz. 2009. “Annual Medical Spending Attributable to Obesity: Payer- and Service-Specific Estimates.” Health Affairs 28 (5): w822–31. Grimes, C. A., L. J. Riddell, K. J. Campbell, and C. A. Nowsonm. 2013. “Dietary Salt Intake, Sugar-Sweetened Beverage Consumption, and Obesity Risk.” Pediatrics 131 (1): 14–21. Henderson J.J., S.F. Evans, J. A. Straton, S. R. Priest, and R. Hagan. 2003. “Impact of Postnatal Depression on Breastfeeding Duration.” Birth 30 (3):175–80. Kiernan, K. E., and M. C. Huerta. 2008. “Economic Deprivation, Maternal Depression, Parenting and Children’s Cognitive and Emotional Development in Early Childhood.” British Journal of Sociology 59 (4): 783–806. MATERNAL DEPRESSION AND DIET QUALITY 9 Kröller, K., and P. Warschburger. 2009. “Maternal Feeding Strategies and Child’s Food Intake: Considering Weight and Demographic Influences Using Structural Equation Modeling.” International Journal of Behavioral Nutrition and Physical Activity 6 (78). Lovejoy, C. M., P. A. Graczyk, E. O’Hare, and G. Neuman. 2000. “Maternal Depression and Parenting Behavior: A Meta-Analytic Review.” Clinical Psychology Review 20 (5): 561–92. Ludwig, D. S., K. E. Peterson, and S. L. Gortmaker. 2001. “Relation between Consumption of Sugar-Sweetened Drinks and Childhood Obesity: A Prospective, Observational Analysis.” Lancet 357: 505–08. Milgrom, J., H. Skouteris, T. Worotniuk, A. Henwood, and L. Bruce. 2011. “The Association Between Ante- and Postnatal Depressive Symptoms and Obesity in Both Mother and Child: A Systematic Review of the Literature.” Women’s Health Issues 22 (3): 319–28. Minkovitz, C. S., D. Strobino, D. Scharfstein, W. Hou, T. Miller, K. B. Mistry, and K. Swartz. 2005. “Maternal Depressive Symptoms and Children’s Receipt of Health Care in the First 3 Years of Life.” Pediatrics 115 (5): 306–14. NRC and IOM (National Research Council and Institute of Medicine), Committee on Depression, Parenting Practices, and the Healthy Development of Children. 2009. Depression in Parents Parenting, and Children: Opportunities to Improve Identification, Treatment and Prevention. Washington, DC: National Academies Press. Nord, C., et al. 2004. Early Childhood Longitudinal Study, Birth Cohort (ECLS-B): User’s Manual for the ECLS-B 9Month Restricted-Use Data File and Electronic Code Book. Washington, DC: Institute of Education Sciences, US Department of Education. Radloff, L. S. 1977. “The CES-D Scale: A Self-Report Depression Scale for Research in the General Population.” Applied Psychological Measurement 1: 385–401. Sealy, Y. M., and L. Farmer. 2011. “Parents’ State of Change for Diet and Physical Activity: Influence on Childhood Obesity.” Social Work in Health Care 50: 274–91. Silverstein, M., M. Augustyn, R. Young, and B. Zuckerman. 2009. “The Relationship between Maternal Depression, In-Home Violence and the Use of Physical Punishment: What Is the Role of Child Behaviour?” Archives of Disease in Childhood 94 (2): 138–43. Snow, K., et al. 2009. Early Childhood Longitudinal Study, Birth Cohort (ECLS-B): Kindergarten 2006 and 2007 Data File User’s Manual. Washington, DC: Institute of Education Sciences, US Department of Education. Topham, G. L., M. C. Page, L. Hubbs-Tait, J. M. Rutledge, T. S. Kennedy, L. Shriver, and A. W. Harrist. 2010. “Maternal Depression and Socio-Economic Status Moderate the Parenting Style/Child Obesity Association.” Public Health Nutrition 13 (8): 1237–44. Turney, K. 2010. “Labored Love: Examining the Link between Maternal Depression and Parenting Behaviors.” Social Science Research 40 (1): 399–415. ———. 2011. “Chronic and Proximate Depression among Mothers: Implications for Child Well-Being.” Journal of Marriage and the Family 73 (1): 149–63. Ventura, A. K., and L. L. Birch. 2008. “Does Parenting Affect Children’s Eating and Weight Status?” International Journal of Behavioral Nutrition and Physical Activity 5: 15. Wang, L., et al. 2013. “Maternal Depressive Symptoms and the Risk of Overweight in Their Children.” Maternal and Child Health Journal 17: 940–48. Weissman, M. M., P. Wickramaratne, Y. Nomura, V. Warner, D. Pilowsky, and H. Verdeli. 2006. “Offspring of Depressed Parents: 20 Years Later.” American Journal of Psychiatry 163 (6): 1001–08. 10 MATERNAL DEPRESSION AND DIET QUALITY About the Author Tracy C. Vericker is a senior research associate at the Urban Institute with over a decade of experience in policy research and evaluation. Focusing on policies and service systems to support vulnerable children and families, she specializes in survey and administrative data management and has led several projects involving complex quantitative analyses. Vericker has substantive expertise in food and nutrition policy and programs. Her work falls into two broad categories: research to support positive health outcomes and research to support improvement of administrative procedures to reduce inefficiencies and encourage participation in the federal food and nutrition programs. Before joining the Urban Institute, Vericker was a Presidential Management Fellow at the Food and Nutrition Service and the Economic Research Service at the USDA. She received her PhD in public policy and administration from The George Washington University in 2011. ABOUT THE URBAN INSTITUTE 2100 M Street NW Washington, DC 20037 www.urban.org The nonprofit Urban Institute is dedicated to elevating the debate on social and economic policy. For nearly five decades, Urban scholars have conducted research and offered evidence-based solutions that improve lives and strengthen communities across a rapidly urbanizing world. Their objective research helps expand opportunities for all, reduce hardship among the most vulnerable, and strengthen the effectiveness of the public sector. Funders do not determine research findings or influence scholars’ conclusions. Urban scholars and experts are independent and empowered to share their evidence-based views and recommendations shaped by research. Copyright © December 2014. Urban Institute. Permission is granted for reproduction of this file, with attribution to the Urban Institute. MATERNAL DEPRESSION AND DIET QUALITY 11