Spaceflight: Understanding the impact on vascular function
advertisement

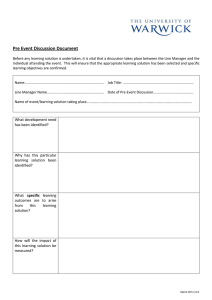
Spaceflight: Understanding the impact on vascular function Christian M. Westby, Ph.D. JSC Cardiovascular Laboratory University Space Research Association Houston, TX, United States Outline • Gender differences in venous function following 60-days headdown bedrest • Radiation induced CVD: should we be worried. Orthostatic Intolerance Orthostatic hypotension - the inability to maintain standing blood pressure. – Presyncope (lightheadedness, loss of peripheral vision) –Syncope This is a potential threat to both crew and vehicle. Postflight Orthostatic Hypotension The incidence and severity of postflight orthostatic hypotension has a complex, interrelated set of contributing factors, including: – – – – – – – Dehydration Direct Cardiac effects Changes in blood vessel responses Loss of neural control of blood pressure Duration of flight Individual preflight characteristics Gender Tilt tolerance after space flight Survival Analysis 1.0 Survival 0.8 0.6 0.4 Pre-flight Shuttle R+0 Long Duration R+0 0.2 0.0 0 2 4 6 Time(minutes) 8 10 Reduced Post-Flight Orthostatic Tolerance Flight Program Mercury-Atlas 9 (34 hrs of orbital flight) Gemini (3-14 day missions) Post-Flight Orthostatic Tolerance Moderate orthostatic hypotension Reduced orthostatic tolerance: ↑heart rate, pulse pressure, ↑venous pooling Orthostatic Challenge Tilt Table Hoffler GW, Johnson RL. Chapter 4: Apollo Flight Crew Cardiovascular Evaluations in Biomedical Results of Apollo, Johnston RS, Dietlein LF, and Berry CA, Eds. NASA SP-368, 1975. Tilt Table (70 upright tilt) Hoffler GW, Johnson RL. Chapter 4: Apollo Flight Crew Cardiovascular Evaluations in Biomedical Results of Apollo, Johnston RS, Dietlein LF, and Berry CA, Eds. NASA SP-368, 1975. Lower Body Negative Pressure and Static Stand Test Hoffler GW, Johnson RL. Chapter 4: Apollo Flight Crew Cardiovascular Evaluations in Biomedical Results of Apollo, Johnston RS, Dietlein LF, and Berry CA, Eds. NASA SP-368, 1975. (Symptoms persisted up to 50 hours after splashdown) Apollo (6-13 day missions) Reduced orthostatic tolerance: ↑heart rate, pulse pressure, stroke volume, body weight (Symptoms persisted for 7 to 19 hours after landing) Skylab (28, 59, and 84 day missions) EDOMP (4-14 day missions) Reduced orthostatic tolerance: ↑heart rate, pulse pressure, Lower Body Negative Pressure Johnson RL, Hoffler GW, Nicogossian AE, et al. Chapter 29: Lower Body Negative Pressure: Third Manned Skylab Mission in Biomedical Results from Skylab, Johnston RS and Dietlein LF eds., NASA SP-377, 1977. Monitoring during first stand after landing, Static stand test, Lower Body Negative Pressure Charles JB, Fritsch-Yelle JM, Whitson PA, et al. Chapter 1: Cardiovascular Deconditioning in Extended Duration Orbiter Medical Project: Final Report 1989-1995. Sawin SF, Taylor GR, Smith WL, eds. NASA SP-1999-534. (No detailed recovery time but stated as longer than Apollo) Reduced orthostatic tolerance: ↑heart rate, pulse pressure, (Symptoms persisted up to 2 days) References Volume Distribution in Humans • 70 % of blood volume is below heart • 19x more blood in capacitance vessels than resistance vessels • Up to 1 liter of blood resides in gut and legs • Without a gravitational field, blood redistributes, shifts head ward Loring B. Rowell, 1986 Example of cephalad fluid shift Pre-flight press briefing Day-2 in flight Gender Differences There is great individual variability in susceptibility to postflight orthostatic hypotension. The primary separating characteristic between presyncopal and nonpresyncopal astronauts is gender Orthostatic Tolerance Females ~20% ~80% Presyncopal Males ~20% ~80% Non-presyncopal Gender Differences in Venous Function Rat suspended hind limb model Zhang, LF. 1996 Arterial Remodeling Zhang LF et. al. J Gravit Physiol. 1996;3(2):5-8 Arterial Function Zhang LF et. al. J Gravit Physiol. 1996;3(2):5-8 Specific Aims To compare venous responses before and after bed rest: 1. between the hand and foot 2. between men and women Subject Characteristics Variable (pre bedrest) Male (n=16) Female (n=10) Age, yr 34 ± 2 37 ± 2 Body mass, kg 79.8 ± 2.4 61.3 ± 3.1* BMI, kg/m2 26.6 ± 0.5 23.8 ± 0.9* Systolic BP, mmHg 122 ± 2 104 ± 2* Diastolic BP, mmHg 80 ± 2 67 ± 2* 29.5 ± 1.9 24.7 ± 1.6 • VO2max, ml/kg/min Mean ± SEM; *p < 0.05 Ultrasound Images Venous Compliance (hand) 7.0 7.0 Pre Post 6.0 5.0 5.0 2 Area (mm ) 6.0 2 Area (mm ) Pre Post 4.0 3.0 4.0 3.0 2.0 2.0 1.0 1.0 Male Female 0.0 0.0 20 30 Pressure (mmHg) 40 20 30 Pressure (mmHg) 40 Venous Compliance (foot) 3.0 3.0 Pre Post Pre Post * 2.5 2.5 * 2.0 * 2 Area (mm ) 2 Area (mm ) 2.0 1.5 1.5 1.0 1.0 0.5 0.5 0.0 0.0 20 30 Pressure (mmHg) 40 20 30 Pressure (mmHg) 40 ACh Mediated Dilation 2 Change in area (mm ) 1.0 * Pre Post 1.0 0.8 0.8 0.6 0.6 0.4 0.4 0.2 0.2 0.0 0.0 -0.2 -0.2 Male Pre Post Female -0.4 -0.4 0.10 0.316 1.00 Acetylcholine (mmol) 3.16 0.10 0.316 1.00 Acetylcholine (mmol) 3.16 Venoconstriction 0.6 Male Female 0.5 2 Area (mm ) 0.4 0.3 0.2 0.1 0.0 Pre Post Phenylephrine Smooth Muscle Function 1.4 Male Female 1.2 Area (mm2) 1.0 0.8 0.6 0.4 0.2 0.0 Pre Post Nitorglycerine Nitric Oxide 5 5 Saline LNMMA 4 2 Area (mm ) 2 Area (mm ) 4 Saline LNMMA 3 2 1 3 2 1 0 0 Pre Post Acetylcholine Pre Post Acetylcholine Shear Stress Acetylcholine Bradykinin R L-NMMA - NOS L-ARGININE ENDOTHELIUM PGI L-citrulline Nitric Oxide Nitric Oxide Guanylate cyclase (inactive) Guanylate cyclase (active) cGMP SMOOTH MUSCLE Relaxation GTP 2 Prostaglandins 5 5 Saline PGI2 4 Area (mm2) Area (mm2) 4 Saline PGI2 3 2 1 3 2 1 0 0 Pre Post Prostaglandin Inhibition Pre Post Prostaglandin Inhibition Shear Stress Acetylcholine Bradykinin R L-NMMA - NOS EDHF L-ARGININE ENDOTHELIUM PGI L-citrulline Nitric Oxide Nitric Oxide Guanylate cyclase (inactive) Guanylate cyclase (active) cGMP SMOOTH MUSCLE Relaxation GTP 2 Conclusion • Males: – decrease venous compliance – Differences in vasodilator response • Females: – do not change venous compliance – EDHF or central reset Venous Compliance (foot) 3.0 3.0 Pre Post Pre Post * 2.5 2.5 * 2.0 * 2 Area (mm ) 2 Area (mm ) 2.0 1.5 1.5 1.0 1.0 0.5 0.5 0.0 0.0 20 30 Pressure (mmHg) 40 20 30 Pressure (mmHg) 40 Survival Analysis 100 Survival (%) 80 60 40 20 Male Female 0 0 3 6 9 Time (min) 12 15 Future Research Future Directions/Areas of Interest 1. Gender differences in orthostatic hypotension and venous tone regulation 2. Space-like radiation and CVD risk Space Exploration and CVD Risk • Astronauts outside the protection of the earth’s magnetic field will be continuously exposed to low levels of space radiation. – Increased risk for the development of certain diseases such as cancer • The same evidence used for cancer risk prediction suggests that exposure to low-dose radiation may also contribute to an increased risk for cardiovascular disease (CVD). The Vascular Endothelium Endothelial Cells Connective Tissue Smooth Muscle Cells Atherosclerosis Timeline Foam Cells Fatty Intermediate Streak Lesion Atheroma From First Decade Complicated Lesion/ Fibrous Rupture Plaque Endothelial Dysfunction From Third Decade From Fourth Decade Adapted from Pepine CJ. Am J Cardiol. 1998;82 suppl 10A Epidemiological Support • Patients who received radiotherapy as part of their treatment for a peptic ulcer – CVD-related mortality was ~24% higher compared to non-irradiated patients. Experimental Support Datta et al. demonstrated that in mice irradiated with 56Fe there was a significant increase in ROS and the pro-inflammatory cytokines IL-6 and TNF- , compared with gamma irradiation Experimental Support Factors associated with vascular dysfunction Luscher T F et al. Circulation 2000;102:2434-2440 Effects of Space-like Radiation on the Vessel Wall? Inflammation/Oxidation Cell Adhesion/Migration ↑ Cytokines • TNF-α, CRP ↑ Oxidative stress • oxLDL, superoxide monocyte adherence CAM expression chemotaxis Lumen Coagulation/Fibrinolysis fibrinogen factors VII, X PAI-1 Endothelial Vasoregulation Study 1 General Hypothesis Exposure to space-like radiation will impair endothelial vasodilator function and that this will be mediated by an increase in oxidative stress and associated with increased systemic inflammation. Study 1 Specific Aims 1. 2. 3. To determine if endothelial vasodilator function is decreased in rats exposed to low-fluence high energy particle radiation and whether the effects extend across different radiation ion types. To determine if the radiation-related decrease in endothelial vasodilator function is due to increased oxidative stress and if so, whether this is due to an increase in superoxide formation regulated at the level of NADPH oxidase. To determine if the radiation-related decrease in endothelial vasodilator function is associated with increased systemic inflammation. Study 1 Design Infusion Protocol Study 2 General Hypothesis Long-term exposure to fractionated low-dose space-like radiation in the presence of modeled microgravity will have a synergistic deleterious effect on endothelial vasodilator function. Endothelial Cell eNOS (uncoupled) NADPH oxidase O2- ONOO- COX eNOS Vasodilator prostanoids NO Vasoconstrictor prostanoids NADPH oxidase ONOOO2 O2- O2NO ONOOiNOS (uncoupled) Nucleus Vascular Smooth Muscle Cell NF-κB Study 2 Specific Aims • To determine if the vascular effects of long-term exposure to fractionated space-like radiation combined with modeled microgravity differ from the vascular effects following exposure to radiation or modeled microgravity alone. • To determine if the expression, release and availability of nitric oxide differs in animals exposed to radiation compared to modeled microgravity alone. • To identify differences in transcriptional control of nitric oxide dependent, atheroprotective pathways between groups. Study 2 Design SHAM Vascular function HLU 56Fe 1000 MeV/u Regulation and expression of nitric oxide 60 120 HLU + 56Fe 1000 MeV/u 240 Changes in NO-mediated pathways associated with vascular endothelial atheroprotective processes Contributions • Does exposure to space-like radiation (at low doses) contribute to an increase risk for CVD • Is the type of radiation important in explaining changes in vascular function and CVD risk? • What is the effect of exposure to microgravity combined with fractionated low-dose radiation Acknowledgments Steve Platts, Ph.D. Mike Stenger, Ph.D. Shang-Jin Shi, M.D. Ph.D. Stuart Lee Natalia Arzeno Susan Bourbonais Angie Brown Tim Cain Sondra Freeman-Perez David Martin Tim Matz Tiffany Phillips Chris Ribeiro Donna South Sydney Stein Michael Willig