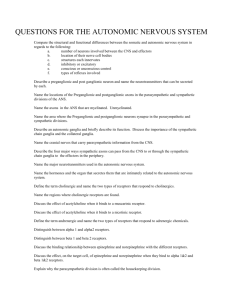
Autonomic Nervous System (Chapter 9) Autonomic Nervous System (ANS) – general properties
advertisement

Subdivisions of Nervous System Autonomic Nervous System (Chapter 9) Central nervous system • Autonomic Nervous System (ANS) – general properties – anatomy • Autonomic Effects on Target Organs Brain Spinal cord Visceral sensory division • Who Controls Autonomic Function • Somatic Nervous System Peripheral nervous system Sensory division Somatic sensory division Motor division Visceral motor division Somatic motor division Skin, bones, Muscles, Joints, Senses Sympathetic division 15-1 12-2 Parasympathetic division Role of the Autonomic Division in General Properties of ANS Homeostasis • autonomic nervous system (ANS) – a motor nervous system that controls glands, cardiac muscle, and smooth muscle • Maintains homeostasis • Primary effectors of the ANS • viscera of thoracic and abdominal cavities – cutaneous blood vessels – some exocrine glands – piloerector muscles – eyes – some endocrine glands • carries out actions involuntarily – no intent/awareness • visceral effectors do not depend on the ANS to function 15-3 Figure 11-1 Divisions of ANS • Divisions of ANS • 2 Divisions dualing innervate most organs – – sympathetic division (Fight or Flight) prepares body for physical activity: exercise, trauma, arousal, competition, anger, or fear • increases heart rate, BP, airflow • reduces blood flow to skin and digestive tract • increases blood to skeletal muscle • Glycogen to glucose (blood glucose) • Fat breakdown • Pupil dilation • Salivation increased 2 Divisions dualing innervate most organs – parasympathetic division (Rest and digest) calms many body functions reducing energy expenditure and assists in bodily maintenance – Constricts pupils and bronchioles – Slows heart – Stimulates • Digestion • Insulin release • Urination parasympathetic division (Rest and digest) calms many body functions reducing energy expenditure and assists in bodily maintenance • digestion and waste elimination 15-5 15-6 1 Autonomic tone • Neural Pathways autonomic tone - represents the balance of the two systems according to the body’s changing needs • – parasympathetic tone • maintains smooth muscle tone in intestines • holds resting heart rate down to about 70 – 80 beats per minute – sympathetic tone • keeps most blood vessels partially constricted and maintains blood pressure ANS has components in both the central and peripheral nervous systems – nuclei in the hypothalamus and other brainstem regions – motor neurons in the spinal cord and peripheral ganglia – nerve fibers that travel through the cranial and spinal nerves 15-7 15-8 Somatic versus Autonomic Pathways Autonomic Control Centers in the Brain (the 2 major pathways of motor neurons) • Hypothalamus – Water balance, temperature, and hunger Temperature control Water balance • Medulla oblongata – – – – Respiration Cardiac Vomiting Swallowing ACh Hypothalamus Eating behavior • Pons – Respiration Somatic efferent innervation Pons Urinary bladder control Secondary respiratory center Blood pressure control Respiratory center Myelinated fiber Somatic effectors (skeletal muscles) Autonomic efferent innervation Medulla ACh Myelinated preganglionic fiber ACh or NE Unmyelinated postganglionic fiber Visceral effectors (cardiac muscle, smooth muscle, glands) Autonomic ganglion Preganglionic cell bodies in grey matter 15-10 Figure 11-3 Sympathetic Nervous System • Aka thoracolumbar division (T1 – L2) • relatively short preganglionic and long postganglionic fibers • Sympathetic Nervous System – each paravertebral ganglion is connected to a spinal nerve by two branches – communicating rami (rami communicants) – preganglionic fibers are small myelinated fibers that travel from spinal nerve to the ganglion via white communicating ramus (myelinated) – postganglionic fibers leave the ganglion via gray communicating ramus (unmyelinated) • forms a bridge back to the spinal nerve – postganglionic fibers extend to the target organ preganglionic cell bodies in lateral horns & gray matter of spinal cord – lead to 1. 2. sympathetic chain of ganglia (paravertebral ganglia) collateral (prevertebral) ganglia 15-11 15-12 2 Other ganglia of Sympathetic Nervous System Sympathetic Chain Ganglia • • collateral ganglia (prevertebral ganglia) Some preganglionic fibers pass thru sympathetic chain - splancic nerves - synapse in collateral (prevertebral ganglia) contribute to network called the abdominal aortic plexus – 3 major collateral ganglia in this plexus • • – celiac, superior mesenteric, and inferior mesenteric postganglionic fibers accompany these arteries and their branches to their target organs solar plexus – collective name for the celiac and superior mesenteric ganglia • nerves radiate from ganglia like rays of the sun 15-14 Preganglionic Pathways Efferent Pathways of sympathetic division 3 pathways of preganglionic neurons entering sympathetic chain Soma of preganglionic neuron Salivary glands To iris, salivary glands, lungs, heart, thoracic blood vessels, esophagus Preganglionic neurons Postganglionic neurons Cervical Spinal nerve Somatic motor fiber Thoracic Preganglionic sympathetic fiber Lumbar Sacral Postganglionic sympathetic fiber To somatic effector (skeletal muscle) 1 White ramus Gray ramus Preganglionic neuron 3 pathways of leaving sympathetic chain Liver and gallbladder Stomach Superior mesenteric ganglion Spleen Pancreas 3 Splanchnic nerve Somatic neuron Lung Celiac ganglion To sweat glands, piloerector muscles, and blood vessels of skin and skeletal muscles Soma of somatic motor neuron Heart Cardiac and pulmonary plexuses Regions of spinal cord Sympathetic nerve 2 Postganglionic neuron Eye Pons Communicating rami Collateral ganglion Soma of postganglionic neuron Postganglionic sympathetic fibers Sympathetic trunk Postganglionic fibers to skin, blood vessels, adipose tissue Inferior mesenteric ganglion Small intestine Large intestine Rectum Sympathetic chain ganglia Adrenal medulla Kidney To liver, spleen, adrenal glands, stomach, intestines, kidneys, urinary bladder, reproductive organs Sympathetic ganglion 2 15-15 Ovary Penis Scrotum Uterus Bladder Adrenal Glands Summary of Sympathetic Innervation • essentially a sympathetic ganglion secretes catecholamines: - 85% epinephrine (adrenaline) - 15% norepinephrine (noradrenaline) • effectors in body wall are innervated by sympathetic fibers in spinal nerves • effectors in head and thoracic cavity are innervated by fibers in sympathetic nerves • sympathoadrenal system is adrenal medulla and sympathetic nervous system • effectors in abdominal cavity are innervated by sympathetic fibers in splanchnic nerves 15-17 15-18 3 The Adrenal Medulla Parasympathetic Division Adrenal cortex: endocrine gland (steroid hormones) • parasympathetic division (aka craniosacral division) Adrenal medulla: modified sympathetic ganglion. • origin preganglionic neurons – midbrain, pons, and medulla (III, VII, IX, X) – sacral spinal cord segments S2-S4 Adrenal gland Kidney (b) (a) ACh Preganglionic sympathetic neuron Chromaffin Cell: modified postganglionic sympathetic neuron. (c) Adrenal medulla • terminal ganglia in or near target organs – long preganglionic, short postganglionic fibers Blood vessel Epinephrine is a neurohormone that enters the blood. To target tissues 15-20 Parasympathetic Sacral Nerves Parasympathetic Cranial Nerves • Facial n. (CN VII) Postganglionic neurons Ciliary ganglion Submandibular ganglion Submandibular salivary gland Thoracic Lumbar Sacral Facial nerve (VII) – tear, nasal and salivary glands • Heart Pulmonary plexus Esophageal plexus Liver and gallbladder Spleen Pancreas Pelvic splanchnic nerves Kidney and ureter Transverse colon Descending colon Inferior hypogastric plexus Small intestine Rectum Pelvic nerves Penis Uterus • Postganglionic neurons Ciliary ganglion Lacrimal gland Eye Submandibular ganglion Submandibular salivary gland Otic ganglion Parotid salivary gland Glossopharyngeal n. (CN IX) form pelvic splanchnic nerves that lead to the inferior hypogastric plexus Vagus n. (CN X) Heart Cardiac plexus Regions of spinal cord Cervical Pulmonary plexus Esophageal plexus Lung Thoracic • Stomach Abdominal aortic plexus Ovary • Glossopharyngeal nerve (IX) – parotid salivary gland Lung Celiac ganglion Facial n. (CN VII) Arise from levels S2 to S4 of the spinal cord Parotid salivary gland Glossopharynge al n. (CN IX) Cardiac plexus Regions of spinal cord Cervical • Lacrimal gland Eye Otic ganglion Vagus n. (CN X) Oculomotor n. (CN III) Preganglionic neurons Pterygopalatine ganglion Oculomotor n. (CN III) Preganglionic neurons Pterygopalatine ganglion Oculomotor nerve (III) – pupil constriction/lens focus Vagus nerve (X) – viscera as far as proximal half of colon – cardiac, pulmonary, and esophageal plexus – 75% of all Parasympathetic fibers most form pelvic nerves to their terminal ganglion on the target organs Lumbar Sacral Celiac ganglion Stomach Liver and gallbladder Abdominal aortic plexus Spleen Pancreas – distal half of colon, rectum, urinary bladder, and reproductive organs Kidney and ureter Transverse colon Descending colon Small intestine Rectum Pelvic nerves Bladder Scrotum Penis Ovary 15-21 Uterus Neurotransmitters and Receptors Enteric Nervous System • What determines if an autonomic neuron is excitatory or inhibitory • enteric nervous system – nervous system in wall of digestive tract – does not arise from the brainstem or spinal cord – innervates smooth muscle and glands • Effects determined by 1. type of neurotransmitter released 2. type of receptors found on target cells • semiautonomous • 2 things to remember: • has its own reflex arcs – sympathetic (NE) and parasympathetic fibers (Ach) secrete different neurotransmitters • regulates motility of esophagus, stomach, and intestines and secretion of digestive enzymes and acid • normal digestive function also requires regulation by sympathetic and parasympathetic systems Bladder Scrotum – target cells respond to the same neurotransmitter differently depending upon the type of receptor they have for it 15-23 • all autonomic fibers secrete either Ach or NE • there are 2 classes of receptors for each of these neurotransmitters 15-24 4 ANS Neurotransmitters Neurotransmitters and Receptors • Both Symp and Parasymp preganglionics release ACh • Parasymp postganglionics also release ACh – Called cholinergic synapses • Most Sympathetic postganglionics release Norepinephrine – Called adrenergic synapses – A small number release ACh (a) Parasympathetic fiber Nicotinic receptor ACh Target cell ACh Preganglionic neuron Postganglionic neuron Muscarinic receptor (b) Sympathetic adrenergic fiber Nicotinic receptor ACh Target cell Preganglionic neuron Postganglionic neuron NE MOST Adrenergic receptor (c) Sympathetic cholinergic fiber Nicotinic receptor ACh Target cell Preganglionic neuron Postganglionic neuron ACh Muscarinic receptor 15-26 9-23 Comparison of nicotinic and muscarinic ACh receptors Acetylcholine (ACh) • ACh is secreted by all preganglionic neurons in both divisions and the postganglionic parasympathetic neurons – called cholinergic fibers – any receptor that binds it is called cholinergic receptor • 2 types of cholinergic receptors – muscarinic receptors • all cardiac muscle, smooth muscle, and gland cells have muscarinic receptors • excitatory or inhibitory due to subclasses of muscarinic receptors – nicotinic receptors • on all ANS postganglionic neurons, adrenal medulla, and neuromuscular junctions of skeletal muscle • excitatory when ACh binding occurs 5 types of muscarinic receptors!! 15-27 9-28 Monoamine NTs (Catecholamines) Norepinephrine (NE) • • NE is secreted by nearly all sympathetic postganglionic neurons – called adrenergic fibers – receptors for it called adrenergic receptors Use G-proteins and Second Messengers • alpha-adrenergic receptors – usually excitatory – 2 subclasses use different second messengers (α1 & α2) • beta-adrenergic receptors – usually inhibitory – 2 subclasses with different effects, but both act through cAMP as a second messenger (β1 & β2) 15-29 7-65 5 ANS • Many drugs have been developed to affect ANS receptors – Drugs that promote actions of a NT are agonists – Drugs that inhibit actions of a NT are antagonists • Postganglionics have unusual synapses called varicosities – release NTs along a length of axon – Target cell doesn’t have clusters of receptors at specific sites – Neuroatransmitters diffuses to receptors 9-26 Dual Innervation Dual Innervation • dual innervation - most viscera receive fibers from both parasympathetic and sympathetic divisions • antagonistic effects - oppose each other cooperative effects – two divisions act on different effectors to produce a unified overall effect – parasympathetics increase salivary serous cell secretion – sympathetics increase salivary mucous cell secretion – exerted through dual innervation of same effector cells • heart rate decreases (parasympathetic) • heart rate increases (sympathetic) – exerted because each division innervates different cells 15-33 Dual Innervation of the Iris 15-34 Sympathetic and Vasomotor Tone Brain Parasympathetic fibers of oculomotor nerve (III) Superior cervical ganglion sympathetic division prioritizes blood vessels to skeletal muscles and heart in times of emergency Sympathetic fibers Ciliary ganglion blood vessels to skin vasoconstrict to minimize bleeding if injury occurs during stress or exercise Cholinergic stimulation of pupillary constrictor Iris Pupil Sympathetic (adrenergic) effect Sympathetic nerve fiber 1 Strong sympathetic tone 2 2 Smooth muscle contraction 3 Vasomotor tone Spinal cord Adrenergic stimulation of pupillary dilator Artery 1 Parasympathetic (cholinergic) effect 3 Vasoconstriction (a) Vasoconstriction 1 1 Weaker sympathetic tone 2 3 2 Smooth muscle relaxation 3 Vasodilation Figure 15.9 (b) Vasodilation Pupil dilated Pupil constricted 15-35 Figure 15.10 15-36 6 Somatic Motor Division Somatic Motor Division • Single neuron – CNS origin – Myelinated • Terminus – Branches – Neuromuscular junction Figure 11-11 (1 of 5) Anatomy of the Neuromuscular Junction Anatomy of the Neuromuscular Junction Schwann cell sheath Somatic motor neuron The neuromuscular junction Axon terminal Mitochondria Muscle fiber Terminal bouton Motor end plate Figure 11-12 (1 of 3) Anatomy of the Neuromuscular Junction Synaptic vesicle (ACh) Figure 11-12 (2 of 3) Events at the Neuromuscular Junction Somatic motor neuron Axon terminal Presynaptic membrane Ca2+ Synaptic cleft Nicotinic ACh receptors Postsynaptic membrane ACh Voltage-gated Ca2+ channel Skeletal muscle fiber (a) Figure 11-12 (3 of 3) Ca2+ Action potential Acetyl + choline AChE Nicotinic receptor Motor end plate Figure 11-13a 7 Events at the Neuromuscular Junction Open channel Closed channel ACh K+ Na+ K+ Na+ (b) Figure 11-13b 8