C S L LINICAL
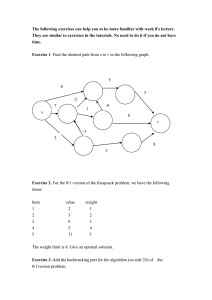
advertisement

Journal of C LINICAL S PEECH AND L ANGUAGE S TUDIES Official Journal of the Irish Association of Speech and Language Therapists Volume 21 2014 ISSN 0791-5985 J&R Press Ltd JOURNAL OF CLINICAL SPEECH AND LANGUAGE STUDIES Editor’s Notes A peer-reviewed periodical published by the Irish Association of Speech and Language Therapists (IASLT). The purpose of the Journal is to encourage and showcase the growing research environment in Ireland and to provide a forum for the exchange of information and discussion of both clinical and theoretical issues regarding communication science and disorders in children and adults, swallowing and its disorders, as well as speech and language therapy. The 2014 issue of the Journal of Clinical Speech and Language Studies presents three research papers and one book review. The three research papers were based on undergraduate research projects conducted by speech and language therapy students in Ireland. The paper by Armstrong, O’Malley, Collins and Carroll is a qualitative study that explores the parents’ opinions regarding the impact of stuttering on the lives of their school-aged children. The paper by Lee and Moore reports the usage of non-speech oral motor exercises by clinicians in Ireland for treating speech sound disorders in children; and the paper by Bessell and Mulhall studies the perceived location, occupation and socio-economic class of three accents from County Cork and reported the phonetic characteristics of these accents. Editor Alice Lee, University College Cork, Ireland Advisory Editorial Board Rozanne Barrow, Beaumont Hospital, Dublin, Ireland Clare Carroll, National University of Ireland, Galway, Ireland Fiona Gibbon, University College Cork, Ireland Margaret Leahy, Trinity College Dublin, Ireland Arlene McCurtin, University of Limerick, Ireland Carol-Anne Murphy, University of Limerick, Ireland Clothra Ní Cholmáin, Trinity College Dublin, Ireland Ciara O’Toole, University College Cork, Ireland Irene Walsh, Trinity College Dublin, Ireland Margaret Walshe, Trinity College Dublin, Ireland For permission to reprint or copy journal content for any other purpose, request should be sent to the IASLT: Irish Association of Speech and Language Therapists Block 4, Harcourt Centre, Harcourt Road, Dublin 2, Ireland Tel/Fax: +353 (0)85 7068707 Email: info@iaslt.ie Website: http://www.iaslt.ie For queries about the Journal and manuscript submission, contact the Editor: Dr Alice Lee Department of Speech and Hearing Sciences, University College Cork, Brookfield Health Sciences Complex, College Road, Cork Ireland Tel: +353 (0)21 4901540; Fax: +353 (0)21 4901542 Email: a.lee@ucc.ie For subscription matters, contact the Publisher: J&R Press Tel: +44 (0)1483 894256 Website: http://www.jr-press.co.uk/ I would like to thank Dr Nicola Bessell in the Department of Speech and Hearing Sciences at University College Cork for reviewing a recently-published title, Methods in Teaching Clinical Linguistics and Phonetics (edited by Dr Nicole Whitworth and Dr Rachael-Anne Knight). Finally, I would like to take the opportunity to encourage members of the IASLT to submit to the Journal, to share the findings of your research projects! Alice Lee University College Cork December 2014 Reviewers The Journal of Clinical Speech and Language Studies would like to thank the following colleagues who served as manuscript reviewers between October 2013 and December 2014: Aidan Doyle, University College Cork, Ireland Arlene McCurtin, University of Limerick, Ireland Carol-Anne Murphy, University of Limerick, Ireland Ciara O’Toole, University College Cork, Ireland Elspeth McCartney, University of Strathclyde, UK Helen Kelly, University College Cork, Ireland Jill Hoover, University of Massachusetts Amherst, USA Joanne Cleland, University of Strathclyde, UK Margaret Leahy, Trinity College Dublin, Ireland Rachel Leonard, HSE (Health Service Executive), Ireland Raymond Hickey, University of Duisburg-Essen, Germany Susanne Cook, University College London, UK Tessa Bent, Indiana University, USA Contents A Survey of the Usage of Nonspeech Oral Motor Exercises by Speech and Language Therapists in the Republic of Ireland 1 Alice Lee and Niamh Moore University College Cork, Ireland A Qualitative Exploration of Maternal Perspectives on the Impact of Stuttering on the lives of 6–10-year-old children 41 Elizabeth Armstrong1, Mary-Pat O’Malley Keighran1, Patricia Collins2 and Clare Carroll1 1National University of Ireland, Galway, Ireland 2Health Service Executive, Shantella, Galway, Ireland What’s in an Accent? Perceptions of Young Adult Listeners in Cork and Kilkenny 63 Nicola Bessell and Eimear Mulhall University College Cork, Ireland Book Review Methods in Teaching Clinical Linguistics and Phonetics 87 A Survey of the Usage of Nonspeech Oral Motor Exercises by Speech and Language Therapists in the Republic of Ireland Alice Lee and Niamh Moore University College Cork, Ireland Correspondence to: Alice Lee, Department of Speech and Hearing Sciences, School of Clinical Therapies, College of Medicine and Health, University College Cork, Brookfield Health Sciences Complex, College Road, Cork, Republic of Ireland Email: a.lee@ucc.ie Abstract Objective: To collect information on the usage of nonspeech oral motor exercises (NSOMEs) by speech and language therapists (SLTs) for treating speech sound disorders (SSDs) in children in the Republic of Ireland. Method: SLTs who had worked with children with SSDs were invited to complete an online questionnaire adapted from a previous survey conducted in the US by Lof and Watson (2008). Main results: 22/39 (56%) of the respondents reported using NSOMEs. Information from a colleague about the usefulness of NSOMEs, continuing education, and literature influenced the respondents the most to use NSOMEs. Most respondents used NSOMEs as a “warm up”, mainly with children with childhood apraxia of speech, dysarthria, and Down Syndrome. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 2 Use of Nonspeech Oral Motor Exercises Conclusion: NSOMEs are used by over half of the respondents despite the lack of evidence that supports this treatment approach. Continuous effort to encourage the application of evidence-based practice in clinics is warranted. Key words: Nonspeech oral motor exercises, speech sound disorders, speech and language therapists, Ireland Introduction Children with speech sound disorders (SSDs) “can have any combination of difficulties with perception, articulation/motor production, and/or phonological representation of speech segments (consonants and vowels), phonotactics (syllable and word shapes) and prosody (lexical and grammatical tones, rhythm, stress and intonation) that may impact speech intelligibility and acceptability” (International Expert Panel on Multilingual Children’s Speech [IEPMCS], 2012, p. 1). The speech difficulties can be due to structural, sensory, and neuromuscular deficits (e.g., cleft palate, hearing impairment, etc.) but, more often, their cause is unknown. Different approaches for treating SSDs in children have been developed (phonetic, phonemic, and hybrid phoneticphonemic treatments; Ruscello, 2008) and the clinical decision on which approach to use for a particular child is based mainly on the cause of the speech problems. One alternative approach for treating SSDs is nonspeech oral motor exercises (NSOMEs). NSOMEs have been defined as “non-speech activities that involve sensory stimulation to or actions of the lips, jaw, tongue, soft palate, larynx, and respiratory muscles that are intended to influence the physiological underpinnings of the oropharyngeal mechanism to improve its function. They may include activities described as active muscle exercise, muscle stretching, passive exercise, or sensory stimulation” (McCauley, 2009, p. 344). For example, nonspeech activities such as smiling, pursing, blowing into horns, and lip massage are used to target lip mobility for the production of speech sounds that involves the lips – /p/, /b/, and /m/ (Marshalla, 2000; Rosenfeld-Johnson, 2001). A few previous systematic reviews (Lass & Pannbacker, 2008; McCauley et al., 2009; Ruscello, 2008) and a recently published Cochrane Systematic Review (Lee & Gibbon, 2015) have shown that there is no strong evidence JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 3 to support the efficacy of NSOMEs for treating SSDs in children. Moreover, a number of articles have discussed the theoretical grounds of why NSOMEs would not be effective; for example: the clinical forum on NSOMEs published in 2008 in the journal Language, Speech, and Hearing Services in Schools; the special issue on the controversies of NSOMEs published also in 2008 in the journal Seminars in Speech and Language; and other articles and conference papers (e.g., Bowen, 2005; Lof, 2003, 2006, 2007, 2009a, 2009b; Lof & Watson, 2010). Lof and Watson (2010) summarized the arguments about why the effect of NSOMEs do not generalize to speech production. First, the neural organization is task-specific rather than structure-specific. Hence, although the same oral structures are involved in speech production and nonspeech tasks, the neural representations of the two activities are different. Second, many NSOMEs involve isolated training of individual speech movements; however, practising fragmented gestures does not enhance the acquisition of highly-integrated tasks such as speech production. Finally, as speech production does not involve high muscular strength, there is no need to use any activities, such as NSOMEs, to improve the muscle strength or warm up the muscles of articulators. Despite the lack of evidence that support the use of NSOMEs for treating SSDs and the long-standing debate regarding the efficacy of this treatment approach, previous surveys have shown that NSOMEs are used by many clinicians. Three surveys published between 2005 and 2008 showed that 71.5% of the respondents (speech and language therapists or SLTs) in the UK (Joffe & Pring, 2008) and 85% of the respondents (speech-language pathologists or SLPs) in the US (Lof & Watson, 2008) and in Alberta, Canada (Hodge, Salonka, & Kollias, 2005), reported using NSOMTs in their clinical practice. Two very recent surveys reported that 67% of the respondents in the US (Brumbaugh & Smit, 2013) and 37.6% of the respondents in Australia (McLeod & Baker, 2014) indicated using NSOMEs. As stated by Lof and Watson (2008), the information on how clinicians are using NSOMEs in their clinical practice is useful when planning future research on testing the efficacy of NSOMEs. In addition, the findings would have important implications for SLT education and continuous professional education, particularly in the area of evidencebased practice, in Ireland. However, currently there are no statistics regarding the use of NSOMEs by clinicians working in Ireland; therefore, the present study was conducted to answer this question. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 4 Use of Nonspeech Oral Motor Exercises Use of Nonspeech Oral Motor Exercises Method Ethics approval for conducting this study was obtained from the Clinical Research Ethics Committee of the Cork Teaching Hospital in January 2014. Participants SLTs who had worked or were working with children with SSDs in the Republic of Ireland were recruited to participate in this study through two means available to the investigators. The first was the Irish Association of Speech and Language Therapists (IASLT), who informed their members of this study via their website and social media pages (Facebook and Twitter) in February 2014. Members who were willing to take part in the survey were directed to the IASLT website where they had to login as a member to access the questionnaire. In addition, a convenience sample of 18 SLT managers of SLT services in south HSE (Health Service Executive)1, who were on the mailing list of the Department of Speech and Hearing Sciences at University College Cork, were contacted by email and asked to forward the information about this study and the link for the questionnaire to the SLTs working in their service. Development of the questionnaire The questionnaire used in this study was developed by following most of the items in that by Lof and Watson (2008) for investigating the use of NSOMEs by SLPs in the US, as this would allow comparison of results between the two studies. Adaptions were made to ensure the clarity and brevity of the questionnaire. Terminologies and phrases that are relevant to the Irish context were used; for example, “county” instead of “state”; “tick” instead of “check”; “community care” instead of “early intervention (birth to 1 SLT managers working in the following areas were contacted: community care in Cork (Cork North, Cork South Lee, West Cork), Kerry, South Tipperary, Waterford, Wexford; hospitals in Cork; and voluntary agencies in Cork, Kerry, Waterford, Wexford, and Kilkenny. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 5 3)” and “preschool”. For questions that asked about the frequency of usage, four options – “usually, often, sometimes, never” were used instead of three options – “usually, sometimes, never”. The 5-point ordinal scale was spelled out in the current questionnaire (e.g., “strongly agree, agree, neutral, disagree, strongly disagree”). The present questionnaire consisted of four parts (see Appendix). Part A contained six questions which enquired about the respondents’ demographic information, such as education, location of work, and caseload information. Part B was to be completed by respondents who used NSOMEs in their clinical practice. This part consisted of 12 questions which collected information on the factors that influenced the respondents’ use of NSOMEs, their opinions towards NSOMEs, the types of NSOME tasks/materials used and how frequently they were used, and the client groups they treated using NSOMEs. Those who did not use NSOMEs in their clinical practice completed Part C which contained six questions that asked for their opinions regarding this intervention approach and the factors that influenced their opinions. Finally, all respondents completed Part D which enquired the familiarity and use of 14 other speech therapy techniques (e.g., distinctive feature approach) for treating SSDs in children. The questionnaire was piloted on three SLTs-in-training, who were asked to comment on whether the questionnaire was comprehensive and easy to complete; whether the questions were objective enough; and the time taken to complete the questionnaire. The SLTs-in-training commented that the questions were objective enough and they gave suggestions regarding the wording of some questions and other minor issues, such as font size and style. On average, it took each person 10 to 15 minutes to complete the questionnaire. In addition, the authors of the Lof and Watson (2008) paper were consulted and their suggestions were employed for improving the questionnaire. Procedure The potential participants were notified of the present study by an electronic information sheet which detailed the aims and rationale of the study and included a link to access the electronic questionnaire. The questionnaire was presented using a free online survey tool (http://esurv.org/). The first page of the questionnaire was a consent page, where it stated that clicking the “Next” JCSLS Vol. 21 2014 © IASLT/TCD/UCC 6 Use of Nonspeech Oral Motor Exercises Use of Nonspeech Oral Motor Exercises button at the bottom of this page constituted as willingness to participate in the survey (see Appendix). The participants were given four weeks to complete the questionnaire. Two weeks into the survey, a reminder message was sent to participants via the IASLT and the SLT managers to encourage participation in the survey. All responses were stored in a password-protected account of the second author on the free online survey tool. Frequency count and percentage were used to summarize the results for each question in the questionnaire. The responses in the account of the free online survey tool were deleted once the data was analyzed. Chi-square test were used to examine whether (1) the use of NSOMEs was related to the number of years of clinical experience; (2) whether the level of agreement or disagreement with the assumptions of NSOMEs was related to whether the respondent was a user or non-user of NSOMEs; and (3) whether the level of familiarity with research and theory of NSOMEs was related to whether the respondent was a user or non-user of NSOMEs, if at least 80% of the cells had expected frequencies of 5 or more (Pallant, 2005). Language Therapy and 28% had a Master’s degree as their highest level of education (see Table 1 for details). Thirty-three respondents supplied the year of award of their Bachelor’s degree; the majority (24/33 or 73%) were awarded in or after 2000 and others were awarded in the period of 1970 to 1999 (see Table 1). For the Master’s degree, most of the respondents received their degree in or after 2000. Table 1 Summary of respondents’ demographic information on education and work location. Demographic Highest level of education (n = 39) Bachelor’s degree in Speech and Language Therapy Master’s degree Forty-six questionnaires were returned; however, for seven of them, only Part A on demographic information was completed. As no information regarding the use of NSOMES could be extracted from these seven questionnaires, they were excluded from data analysis. Of the remaining 39 questionnaires, nine were completed in their entirety; that is, all required questions were answered and the answers were filled out correctly. For the other 30 questionnaires, occasional errors in filling out the questionnaire were found. These errors were, namely, incorrect responses (e.g., entered country name instead of county name for the question on location of work); did not answer a question; and provided two answers where only one was required. Responses with errors were not included in the data analysis. Demographic information of all respondents (Part A) All 39 respondents responded to Question 1 on academic qualifications – two-thirds of the respondents received a Bachelor’s degree in Speech and Number (and percent) of respondents 26 (66%) 11 (28%) Licentiate of the College of Speech Therapists 1 (3%) Postgraduate higher diploma 1 (3%) Year of award of Bachelor’s degree (n = 33) 1970–79 Results 7 1 (3%) 1980-89 3 (9%) 1990-99 5 (15%) 2000-09 19 (58%) 2010-13 5 (15%) Year of award of Bachelor’s degree (n = 10) 1980-89 1 (10%) 1990-99 1 (10%) 2000-09 6 (60%) 2010-13 2 (20%) Work location (n = 35) Cork 17 (49%) Dublin 5 (14%) Kerry 4 (11%) Wexford Kilkenny, Limerick, Wicklow, Galway, Longford, Galway/Mayo, and Longford/Roscommon* 2 (6%) 7 (20%) *These seven locations were each listed once. JCSLS Vol. 21 2014 © IASLT/TCD/UCC JCSLS Vol. 21 2014 © IASLT/TCD/UCC 8 Use of Nonspeech Oral Motor Exercises Use of Nonspeech Oral Motor Exercises Thirty-five respondents indicated where they were working (Question 2) at the time of data collection. Almost half of them were working in Cork, followed by Dublin, Kerry, and Wexford (see Table 1). There was one respondent from each of these areas: Kilkenny, Limerick, Wicklow, Galway, Longford, Galway/Mayo, and Longford/Roscommon. With regards to the work settings (Question 3), most of the respondents worked in a single setting only (27/39 or 69%), with more than half of them working in disability services (14/27 or 52%), followed by community care (10/27 or 37%), private practice (2/27 or 7%), and hospital (1/27 or 4%). Twelve of the 39 respondents reported working in more than one setting and the details are summarized in Table 2. Table 2 Work settings of 12 of the respondents who reported working in more than one setting. Combination of work settings Number of respondents Community care and hospital 3 Disability services and private practice 2 Community care and disability services 1 Community care and a language class 1 Private practice and hospital 1 Hospital and on an early intervention team 1 Private practice and a non-specified “other” setting 1 Community care, hospital, and language class 1 Disability services, hospital, and community care 1 Number of respondents (percentage) Number of respondents who used NSOMEs Number of respondents who did not use NSOMEs 1 to 5 years 20 (51%) 11 9 6 to 10 years 6 (15.5%) 4 2 11 to 15 years 5 (13%) 2 3 2 (5%) 2 0 6 (15.5%) 3 3 15 to 20 years More than 20 years JCSLS Vol. 21 2014 © IASLT/TCD/UCC Table 4 Size of caseload. Demographic Number (and percent) of respondents Number of children on caseload (n = 39) 1–20 6 (16%) 21–40 4 (10%) 41–60 2 (5%) More than 60 27 (69%) Number of children with speech sound disorders on caseload (n = 39) 1–20 18 (46%) 21–40 9 (23%) 41–60 More than 60 3 (8%) 9 (23%) For the number of years of experience working with children with speech sound disorders (Question 4), about two-thirds of the respondents (26/39 or 66.5%) were in their first decade of working with this clinical group, whereas the others had worked with this group for more than 10 years (see Table 3 for details). Most of the respondents (69%) had more than 60 children on their current caseload (Question 5; see Table 4 for details). Finally, regarding the number of children with SSDs on the current caseload (Question 6), almost half of the respondents (46%) had a size of 1–20 children (see Table 4). Table 3 Number of years of experience working with children with speech sound disorders of the 39 respondents and the number of respondents in each category who used and did not use nonspeech oral motor exercises (NSOMEs). Number of years 9 The use of NSOMEs by SLTs (Part B) Twenty-two of the 39 respondents (56%) completed Part B of the questionnaire, indicating that they used NSOMEs in their clinical practice. Table 3 shows the number of users (and non-users) broken down by their number of years of clinical experience. Chi-square analysis was not conducted as there were 80% of cells that had expected count less than 5. As stated in the Method section, SLTs who did not use NSOMEs were instructed to leave Part B blank and to proceed to Part C. However, six of the 22 respondents who completed Part B also completed Part C. It is evident from the answers in Part B that these six respondents did use NSOMEs, and therefore their answers for Part B were JCSLS Vol. 21 2014 © IASLT/TCD/UCC 10 Use of Nonspeech Oral Motor Exercises analyzed whereas their answers for Part C were discarded. The results of this part of the questionnaire are summarized in the following six sub-sections. With whom NSOMEs were used The respondents were asked how frequently they used NSOMEs with eight different client groups (Question 4a to 4h); 19 to 22 respondents gave their answers. None of the respondents indicated usually using NSOMEs with any of the client groups (see Figure 1). NSOMEs were used often or sometimes with children with childhood apraxia of speech (13/21 or 62%), dysarthria (12/20 or 60%), and Down Syndrome (12/22 or 54%). Most respondents never used NSOMEs with children with phonological disorders (14/22 or 64%), function articulation disorders (13/21 or 62%), SSD due to structural anomalies (12/22 or 55%), SSD due to hearing impairment (15/19 or 79%), Figure 1 The number (indicated in the columns) and percentage of respondents who “never”, “sometimes”, “often”, or “usually” used NSOMEs with children with speech sound disorders of different origins. JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 11 and children who are regarded as “late talkers” (15/21 or 71%). The opinion about whether NSOMEs can favour children of any age (Question 12) was divided – 45% (9/20) of the respondents agreed with this statement whereas the others disagreed. Which NSOME materials and tasks were used The questionnaire listed nine NSOME materials (Questions 5a to 5i) and 13 tasks of NSOMEs (Questions 6a to 6m), where the respondents were asked to indicate how frequently they used them with their clients (see Figures 2 and 3). The results showed that, regarding materials, more than half of the respondents used tongue depressors (13/22 or 59%), straws (16/22 or 73%), and whistles (12/22 or 55%). For NSOMEs, more than half of the respondents used the following tasks – pucker-smile alternations (11/21 or 52%), tongue Figure 2 The number (indicated in the columns) and percentage of respondents who “never”, “sometimes”, “often”, or “usually” used nine different NSOMEs materials in their clinical practice JCSLS Vol. 21 2014 © IASLT/TCD/UCC 12 Use of Nonspeech Oral Motor Exercises Use of Nonspeech Oral Motor Exercises 13 professionals (e.g., teachers, occupational therapists) to use this treatment approach (Question 11). From where the respondents learnt about NSOMEs More than half of the respondents indicated that they had observed improved nonspeech oral motor skills as a results of using NSOMEs (18/21 or 86%), and read literature, such as journal articles and book chapters (19/22 or 86%), or internet sources such as websites and blogs (14/22 or 64%) that encourage the use of NSOMEs (Questions 1a to 1g). In addition, 50% of the respondents (11/22) had attended continuing education offerings, workshops, Table 5 Sources of information from where the 22 respondents who reported using nonspeech oral motor exercises (NSOMEs) learnt about this treatment approach and the information sources that influenced their practice the most. Sources of information Figure 3 The number (indicated in the columns) and percentage of respondents who “never”, “sometimes”, “often”, or “usually” used 13 different NSOMEs in their clinical practice. “push-ups” (11/21 or 52%), and blowing (e.g., cotton balls) (14/19 or 74%); and half of the respondents (10/20) used “big smile” exercises. The rest of the materials and tasks were never used by over 50% of the respondents. How NSOMEs were used Seventeen of the 22 respondents answered Question 7. Thirteen (76%) of them used these exercises as a “warm up” with the client; two (12%) used them until the client met a set criterion; one (6%) divided therapy time equally between NSOMEs and speech intervention, and one (6%) reported that the therapy sessions were almost restricted to NSOMEs. In terms of training others to use NSOMEs, most respondents (13/19 or 68%) trained the caregivers of children with SSDs to use NSOMEs as part of a home programme (Question 10), whereas only 10% (2/21) of the respondents trained other a. Taught to use NSOMEs during SLT training (lectures/tutorials) b. Taught to use NSOMEs during SLT training (clinical placement) c. Observed improved speech production after NSOMEs d. Observed improved nonspeech oral motor skills after NSOMEs e. Other speech elicitation exercises did not work for some clients f. Informed by a colleague that NSOMEs are useful g. Attended continuing education on NSOMEs h. Read literature that encourages NSOMEs i Read internet sources that encourages NSOMEs Number of respondents who learned about NSOMEs from this sourcea Number of respondents who found this source influenced their use of NSOMEs the mostb 10 (45%) 2 9 (41%) 1 10 (45%) 3 18 (86%) 1 8 (36%) 1 9 (43%) 7 11 (50%) 7 19 (86%) 6 14 (64%) 1 a22 users of NSOMEs responded to all nine statements, except statements d and f where there was one missing data each. bFourteen of the 22 respondents identified two information sources while one respondent indicated one only, resulting in 29 responses. JCSLS Vol. 21 2014 © IASLT/TCD/UCC JCSLS Vol. 21 2014 © IASLT/TCD/UCC 14 Use of Nonspeech Oral Motor Exercises and/or in-services on the use of NSOMEs (see Table 5). Regarding the two most important sources of information that influenced the respondents’ use of NSOMEs (Question 2), 15 of the 22 respondents gave their answers; one respondent identified one information source only, yielding 29 responses. The results were that information from a colleague about the usefulness of NSOMEs (7/29 or 24%), continuing education offerings or workshops on NSOMEs (7/29 or 24%), and literature (6/29 or 21%) had influenced the respondents the most on their use of NSOMEs. Opinions regarding some assumptions of NSOMEs The majority of the respondents disagreed or strongly disagreed with five of the seven statements surrounding some assumptions of NSOMEs and treatment of SSDs (Questions 3a to 3g): (1) the development of intelligible speech requires the use of separate oral motor tasks (13/20 or 65%); (2) children with SSDs frequently lack the strength needed to produce intelligible speech (12/19 or 63%); (3) the use of NSOMEs for treating SSDs is supported by research literature (15/21 or 71%); (4) dividing complex behaviours of speech into component oral motor movements is an efficient method to treat SSDs (13/21 or 62%); and (5) muscle movements for nonspeech oral tasks will carry over to muscle movements for speech sound productions (14/20 or 70%; see Table 6). Nearly half of the respondents (10/21 or 47%) agreed or strongly agreed that speech develops from early oral behaviours such as sucking or chewing. Finally, there were about the same number of respondents who (strongly-) agreed (9/21 or 43%), or (strongly-) disagreed (8/21 or 38%) that NSOMEs serve as groundwork for the development of more sophisticated motor movements needed for speech production. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 15 Use of Nonspeech Oral Motor Exercises Opinions regarding the benefits of NSOMEs Most of the respondents usually, often, or sometimes used NSOMEs to achieve the following five claimed benefits of the treatment: (1) clients’ awareness of the articulators (16/19 or 84%), followed by (2) drooling control (15/19 or 79%), (3) tongue elevation (13/19 or 68%), (4) feeding (14/21 or 67%), and (5) jaw stabilization (12/19 or 63%). See Table 7 for details of the results. Table 6 The number and percentage (in brackets) of respondents who reported using nonspeech oral motor exercises (NSOMEs) in clinical practice and their opinions towards seven statements on some assumptions of this treatment for speech sound disorders (SSDs). The number of respondents who answered the question was included at the end of each item. Assumptions of NSOMEs and Strongly treatment for SSDs agree a. Development of intelligible speech requires the use of separate oral 2 (10%) motor tasks (n = 20) b. Children with SSDs frequently lack the strength necessary to produce 1 (5%) intelligible speech (n = 19) c. Speech develops from early oral behaviours (e.g., sucking or 3 (14%) chewing) (n = 21) d. NSOMEs serve as groundwork for the development of more sophisticated motor movements 1 (5%) necessary for speech production (n = 21) e. The use of NSOMEs for treating SSDs is supported by research 0 literature (n = 21) f. Dividing complex behaviours of speech into component oral motor 0 movements is an efficient method to treat SSDs (n = 21) g. Muscle movements for NSOMEs will carry over to muscle 0 movements for speech sound productions (n = 20) Agree Neutral Disagree Strongly disagree 1 (5%) 4 (20%) 7 (35%) 6 (30%) 3 (16%) 3 (16%) 9 (47%) 3 (16%) 7 (33%) 5 (24%) 6 (29%) 0 8 (38%) 4 (19%) 7 (33%) 1 (5%) 0 6 (29%) 7 (33%) 8 (38%) 3 (14%) 5 (24%) 8 (38%) 5 (24%) 1 (5%) 5 (25%) 7 (35%) 7 (35%) JCSLS Vol. 21 2014 © IASLT/TCD/UCC 16 Table 7 The number and percentage (in brackets) of respondents who used nonspeech oral motor exercises to achieve 15 claimed benefits of this treatment approach. The number of respondents who answered the question is included at the end of each item. a. Lateral tongue movements (n = 21) b. Tongue protrusion (n = 20) c. Tongue strength (n = 21) d. Lip protrusion (n = 21) e. Lip strength (n = 21) f. Tongue elevation (n = 19) g. Jaw stabilization (n = 19) h. Sucking ability (n = 20) i. Drooling control (n = 19) j. Movement of the frenulum (n = 20) k. Biting (n = 21) l. Velopharyngeal competence (n = 19) m. Clients’ awareness of the articulators (n = 19) n. Swallowing (n = 21) o. Feeding (n = 21) Usually 0 0 1 (5%) 0 1 (5%) 1 (5%) 0 2 (10%) 1 (5%) 1 (5%) 2 (10%) 0 Often 5 (24%) 2 (10%) 3 (14%) 2 (10%) 1 (5%) 3 (16%) 6 (31.5%) 2 (10%) 7 (37%) 2 (10%) 1 (5%) 1 (5%) Sometimes 5 (24%) 6 (30%) 4 (19%) 8 (38%) 6 (28%) 9 (47%) 6 (31.5%) 6 (30%) 7 (37%) 3 (15%) 6 (28%) 8 (42%) Never 11 (52%) 12 (60%) 13 (62%) 11 (52%) 13 (62%) 6 (32%) 7 (37%) 10 (50%) 4 (21%) 14 (70%) 12 (57&) 10 (53%) 1 (5%) 3 (16%) 12 (63%) 3 (16%) 1 (5%) 2 (10%) 4 (19%) 3 (14%) 6 (28%) 9 (43%) 10 (48%) 7 (33%) Familiarity with research and theory related to NSOMEs Most of the respondents reported that they were very familiar or familiar with the research that investigated the effectiveness of NSOMEs (15/21 or 71%), the relationship between NSOMEs and the development of speech (13/20 or 65%), and the theory related to NSOMEs and the relationship to speech (14/21 or 67%) (Questions 8a to 8c; see Table 8 for details of results). Opinions of SLTs who do not use NSOMEs (Part C) How NSOMEs were used Seventeen of the 39 respondents (44%) did not use NSOMEs in their clinical practice. However, two of the 17 respondents (12%) indicated that they JCSLS Vol. 21 2014 © IASLT/TCD/UCC 17 Use of Nonspeech Oral Motor Exercises Use of Nonspeech Oral Motor Exercises Table 8 Familiarity with research and theory related to nonspeech oral motor exercises (NSOMEs) by respondents who used this treatment and those who did not. The number of respondents who answered the question was included at the end of each item. Familiarity with… Respondents who used NSOMEs a. Research that examined NSOMEs effectiveness (n = 21) b. Relationship between NSOMEs and speech development (n = 20) c. Nonspeech oral motor skills theory and its relationship to speech (n = 21) Respondents who did not use NSOMEs a. Research that examined NSOMEs effectiveness (n = 17) b. Relationship between NSOMEs and speech development (n = 17) c. Nonspeech oral motor skills theory and its relationship to speech (n = 17) Very Very Familiar Neutral Unfamiliar familiar unfamiliar 3 (14%) 12 (57%) 5 (24%) 1 (5%) 0 2 (10%) 11 (55%) 4 (20%) 3 (15%) 0 2 (9%) 12 (57%) 6 (29%) 1 (5%) 0 0 11 (65%) 3 (18%) 1 (5%) 2 (12%) 0 10 (59%) 4 (23%) 0 3 (18%) 0 9 (52%) 3 (18%) 2 (12%) 3 (18%) trained the caregivers of children with SSDs to use NSOMEs as part of a home programme (Question 5) and one (1/17 or 6%) trained other professionals to use this treatment approach (Question 6). From where the respondents learned about NSOMEs Almost all respondents indicated that they had not observed improved speech production skills after NSOMEs (16/17 or 94%), although many of them (11/16 or 65%) had observed improved nonspeech oral motor skills after the treatment (Questions 1a to 1g). Most of the respondents reported that they were not taught to use NSOMEs during their professional training (13/17 or 76%) and that they had not read literature that encourages the use of NSOMEs (13/16 or 81%). In addition, more than half of the respondents JCSLS Vol. 21 2014 © IASLT/TCD/UCC 18 Use of Nonspeech Oral Motor Exercises had not heard of the usefulness of NSOMEs from a colleague (10/17 or 59%) and they had not attended any continuing education on the use of NSOMEs (10/17 or 59%). Finally, half of the respondents (8/16 or 50%) had not read internet sources that encourage the use of NSOMEs. Sixteen respondents answered Question 2 regarding the two information sources (as listed in Questions 1a to 1g) that had influenced their opinion on NSOMEs the most. One respondent gave one answer only and four respondents gave their own answers but two of the responses could not be classified; hence, 29 responses were analyzed. The results showed that the respondents did not use NSOMEs mainly because they had not read literature that encourages the use of NSOMEs (7/31 or 23%), had not observed improved speech production skills after NSOMEs (4/31 or 13%), and were not taught to use NSOMEs during their professional training (4/31 or 13%). Opinions regarding some assumptions of NSOMEs All 17 respondents either disagreed or strongly disagreed that muscle movements for nonspeech oral tasks will carry over to muscle movements for speech sound productions (Questions 3a to 3g; see Table 9). Moreover, most of the respondents disagreed or strongly disagreed with another five statements: (1) the development of intelligible speech requires the use of separate oral motor tasks (15/17 or 88%); (2) children with SSDs frequently lack the strength needed to produce intelligible speech (11/16 or 69%); (3) NSOMEs serve as groundwork for the development of more sophisticated motor movements needed for speech production (13/17 or 76%); Use of Nonspeech Oral Motor Exercises 19 Table 9 The number and percentage (in brackets) of respondents who did not use nonspeech oral motor exercises (NSOMEs) in clinical practice and their opinions towards seven statements on some assumptions of this treatment for speech sound disorders (SSDs). The number of respondents who answered the question was included at the end of each item. Assumptions of NSOMEs and Strongly treatment for SSDs agree a. Development of intelligible 0 speech requires the use of separate oral motor tasks (n = 17) b. Children with SSDs frequently lack the strength necessary to 0 produce intelligible speech (n = 16) c. Speech develops from early oral behaviours (e.g., sucking or 0 chewing) (n = 16) d. NSOMEs serve as groundwork for the development of more sophisticated motor movements 0 necessary for speech production (n = 17) e. The use of NSOMEs for treating SSDs is supported by research 0 literature (n = 17) f. Dividing complex behaviours of speech into component oral 0 motor movements is an efficient method to treat SSDs (n = 17) g. Muscle movements for NSOMEs will carry over to muscle 0 movements for speech sound productions (n = 17) Agree Neutral Disagree Strongly disagree 2 (12%) 0 7 (41%) 8 (47%) 2 (12%) 3 (19%) 6 (38%) 5 (31%) 5 (31%) 4 (25%) 5 (31%) 2 (13%) 1 (6%) 3 (18%) 8 (47%) 5 (29%) 0 1 (6%) 3 (18%) 13 (76%) 0 1 (6%) 6 (35%) 10 (59%) 0 0 7 (41%) 10 (59%) (4) the use of NSOMEs for treating SSDs is supported by the research literature (16/17 or 94%); and (5) dividing complex behaviours of speech into component oral motor movements is an efficient method to treat SSDs (16/17 or 94%). Nearly half of the respondents (7/16 or 44%) disagreed or strongly disagreed JCSLS Vol. 21 2014 © IASLT/TCD/UCC that speech develops from early oral behaviours. The chi-square test was not conducted to compare the NSOMEs users and non-users regarding their opinions on the assumptions of NSOMEs, as the assumption of using this test was violated. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 20 Use of Nonspeech Oral Motor Exercises Familiarity with research and theory related to NSOMEs More than half of the respondents reported they were familiar with the research that investigated the effectiveness of NSOMEs (11/17 or 64%), the relationship between NSOMEs and the development of speech (10/17 or 59%), and the theory related to NSOMEs and the relationship to speech (9/17 or 53%) (Questions 4a to 4c; see Table 8 for details of results). The chi-square test was not conducted to examine whether the level of familiarity with research and theory of NSOMEs was related to whether the respondent was a user or non-user of NSOMEs, as the assumption of using this test was violated. SLTs’ use of speech therapy techniques for SSDs (Part D) Thirty-six out of 39 respondents completed the final section of the questionnaires which enquired whether they were familiar with 14 speech therapy techniques and, if they were familiar with them, how frequently they used them in clinical practice. All 36 respondents indicated that they were familiar with minimal pairs, maximal pairs, and the phonemic awareness approach. There were three therapy techniques which were less familiar among the respondents: 40% (14/35) indicated ‘unfamiliar’ for the motokinesthetic approach, 42% (15/36) for the morphosyntactic approach, and 44% (16/36) for the paired stimuli approach. These three techniques, as well as Hodson’s cycles approach, were the four that were used by less than 50% of the respondents (see Table 10). The technique that was used most frequently was minimal pairs – 50% (or 18) of the 36 respondents usually used it, followed by 33% (12/36) who often used it, and 11% (or 4/36) sometimes used it. This is followed by the phonemic awareness approach (which was usually, often, or sometimes used by 32 or 89% of the respondents), maximal pairs (30/36 or 83%), Van Riper traditional approach for sound elicitation (28/35 or 80%), auditory bombardment/stimulation (28/36 or 78%) and whole language approach (28/36 or 78%), the Metaphon approach (27/36 or 75%), and the Van Riper traditional approach for sound stabilization (25/34 or 74%). The remaining two techniques – distinctive feature approach and sensory motor approach – were used by half of the respondents (18/35 or 51% and 19/36 or 53%, respectively). JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 21 Table 10 The respondents’ familiarity and frequency of use of 14 therapy techniques for speech sound disorders. The number of respondents who answered this question was included at the end of each item. Familiar Unfamiliar Therapy technique Usually Often Sometimes Never Minimal pairs (n = 36) 18 (50%) 12 (33%) 4 (11%) 2 (6%) 0 Maximal pairs (n = 36) 1 (3%) 14 (39%) 15 (41%) 6 (17%) 0 Van Riper traditional approach for 7 (20%) 11 (31%) 10 (29%) 4 (11%) 3 (9%) sound elicitation (n = 35) Van Riper traditional approach for 5 (15%) 9 (26%) 11 (32%) 4 (12%) 5 (15%) sound stabilization (n = 34) Auditory bombardment/ 10 (28%) 5 (14%) 13 (36%) 7 (19%) 1 (3%) stimulation (n = 36) Hodson’s cycles approach (n = 35) 1 (3%) 1 (3%) 9 (26%) 14 (40%) 10 (28%) Metaphon approach (n = 36) 1 (3%) 9 (25%) 17 (47%) 8 (22%) 1 (3%) 12 Whole language approach (n = 36) 4 (11%) 12 (33.5%) 4 (11%) 4 (11%) (33.5%) Motokinesthetic approach (n = 35) 1 (3%) 3 (9%) 10 (28%) 7 (20%) 14 (40%) Phonemic awareness approach (n 4 (11%) 13 (36%) 15 (42%) 4 (11%) 0 = 36) Distinctive feature approach (n 2 (6%) 4 (11%) 12 (34%) 10 (29%) 7 (20%) = 35) Morphosyntactic approach (n = 0 3 (8%) 8 (22%) 10 (28%) 15 (42%) 36) Sensory motor approach (n = 36) 3 (8%) 5 (14%) 11 (31%) 10 (28%) 7 (19%) Paired stimuli approach (n = 36) 1 (3%) 3 (8%) 6 (17%) 10 (28%) 16 (44%) Summary of the main findings The present survey found that 56% (22/39) of the respondents indicated using NSOMEs. More than half of the respondents often or sometimes used NSOMEs with children with childhood apraxia of speech, dysarthria, and Down Syndrome. Most of the respondents used tongue depressors, straws, and whistles; and many used the following tasks of NSOMEs – pucker-smile alternations, tongue “push-ups”, blowing, and “big smile” exercises. Most of the respondents used NSOMEs as a “warm up” with clients and they trained JCSLS Vol. 21 2014 © IASLT/TCD/UCC 22 Use of Nonspeech Oral Motor Exercises the caregivers of children with SSDs to use NSOMEs as part of a home programme. Information from a colleague about the usefulness of NSOMEs, continuing education offerings or workshops on NSOMEs, and literature have influenced the respondents the most in their use of NSOMEs. Non-users of NSOMEs, however, did not use this treatment approach because they had not read literature that encourages its use, had not observed improved speech production skills after NSOMEs, and were not taught to use this method during their professional training. In general, most of the users and nonusers of NSOMEs disagreed with the assumptions of NSOMEs for treating SSDs, except one – nearly half of the users and about one-third of the nonusers agreed that speech develops from early oral behaviours (e.g., sucking). Finally, the majority of the respondents were familiar with and frequently used minimal pairs, maximal pairs, and phonemic awareness approaches in their practice. Discussion Percentage of respondents who used NSOMEs This study collected information on the usage of NSOMEs by SLTs who had worked or were working with children with SSDs in the Republic of Ireland through an online questionnaire developed by following the one devised by Lof and Watson (2008) for investigating the same issue in the US. The present results showed that over half of the respondents (56%) reported using NSOMEs in their clinical practice. This finding falls between the latest figures reported – 37.6% in Australia (McLeod & Baker, 2014) and 67% in the US (Brumbaugh & Smit, 2013). However, caution is needed when interpreting the results because of the small number of respondents in the present study – 39 SLTs, which is very low considering the fact that approximately 700 practising SLTs are current members of the IASLT (A. Healy, personal communication, 7 April 2014) and in comparison to the previous surveys, which ranged from 98 (Joffe & Pring, 2008) to 537 respondents (Lof & Watson, 2008). In addition, although the number of years of experience working with children with SSDs of the respondents ranged from 1–5 years to over 20 years, nearly JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 23 half of them were in the category of 1–5 years of clinical experience; hence, it is possible that the result was skewed to some extent. With whom, which, and how NSOMEs were used Regarding the clinical groups with which the clinicians used NSOMEs, the present findings were similar to those reported by Lof and Watson (2008) and Hodge et al. (2005) that this treatment was used with children with childhood apraxia of speech, dysarthria and Down Syndrome. However, the SLPs in the US also used NSOMEs with children with structural anomalies (Lof & Watson, 2008) and the SLPs in Alberta used the treatment with children with phonological/articulation disorders or cerebral palsy as well (Hodge et al., 2005). For the NSOMEs used, the four tasks that were used most frequently by clinicians in Ireland – pucker-smile alternations, tongue “push-ups”, blowing, and “big smile” exercises – were also used frequently by the SLPs who took part in Lof and Watson’s study. However, the other five tasks that were also used frequently by the SLPs in Lof and Watson’s study – tongue lateralizations, tongue-to-nose and tongue-to-chin movements, cheek puffing, blowing kisses, and tongue curling – were used (sometimes or often) by less than 50% of the respondents in the present study. Similar to the findings reported by Lof and Watson, the majority of the SLTs who reported using NSOMEs in this study used this treatment as a “warm up” (68%; Lof & Watson, 2008). However, as reviewed in previous literature (e.g., Lof & Watson, 2010), warm-up of muscles is only needed when engaging in activities that tax the muscular system, such as running. As speech production does not involve high muscular strength, warm-up is really not necessary to prepare the child to engage in speech production tasks. In the present study, most of the respondents who reported using NSOMEs also trained caregivers of children with SSDs to use this treatment as part of a home programme; whereas a small number of respondents who did not use NSOMEs (two persons) trained caregivers to use NSOMEs. For both groups of respondents – users and non-users of NSOMEs – the majority did not train other professionals to use this treatment. The finding that a small number of non-users trained others to use NSOMEs is quite surprising as JCSLS Vol. 21 2014 © IASLT/TCD/UCC 24 Use of Nonspeech Oral Motor Exercises Use of Nonspeech Oral Motor Exercises 25 one would expect that a clinician would not do so if s/he did not believe in or use the treatment approach. articles and books. This finding again highlighted the importance of accessing valid information regarding the efficacy of NSOMEs. From where the respondents learned about NSOMEs Opinions regarding some assumptions of NSOMEs There were both similarities and discrepancies between the present results and those reported by Lof and Watson (2008) concerning the sources of information from which the users of NSOMEs learned about this treatment approach. Both studies reported that most of the respondents reported having observed improved nonspeech oral motor skills after NSOMEs (92.7% of the respondents in Lof and Watson’s study) and that continuing education offerings or workshops on NSOMEs was one important factor that influenced their use of this treatment in clinical practice (87%; Lof & Watson, 2008). However, the other two factors that influenced the SLPs in Lof and Watson’s study to use NSOMEs – observed improved speech productions (86.3%) and using NSOMEs because other speech elicitation techniques did not work (68%) – were not the main reasons why the respondents in the present study used NSOMEs. Instead, the SLTs in this study used NSOMEs because many of them reported having read literature and internet sources that encourage the use of this treatment or they were convinced by a colleague that NSOMEs are useful. This finding has an important implication for SLT education and continuous professional education – students and practising clinicians should be given valid information regarding the efficacy of NSOMEs. There were also similarities and discrepancies in terms of information sources for NSOMEs between users of this treatment approach and non-users in the present study. One similarity was that more than half of the respondents in both groups indicated that they had observed improved nonspeech oral motor skills after NSOMEs. However, the differences were that fewer respondents who were non-users of NSOMEs in this study reported (1) being taught to use this treatment during SLT training, (2) having observed improved speech production after NSOMEs, and (3) having read literature and/or internet sources that encourage the use of this treatment. Interestingly, many users of NSOMEs reported having read literature that supports NSOMEs, which is one important factor that influenced them using this treatment; and at the same time, many non-users reported that they had not read literature that supports NSOMEs and this is one important reason why they did not use NSOMEs. The literature that supports NSOMEs is mostly non-peer-reviewed The present study showed that most of the respondents who reported using NSOMEs did not agree with most of the assumptions about this treatment approach. None of these respondents agreed that the use of NSOMEs for treating SSDs is supported by the research literature. There were relatively more respondents (but still less than 50%) who agreed that speech develops from early oral behaviours, such as sucking or chewing; and that NSOMEs serve as groundwork for the development of motor movements needed for speech production. Lof and Watson (2008) reported that 60% of the SLPs believed that speech develops from early oral behaviours; however, results for other assumptions were not reported. Nevertheless, it is speculated that, in general, relatively fewer clinicians in the present study believed in those assumptions of NSOMEs compared to Lof and Watson’s study which was published six years ago. Comparing the opinions of the respondents who used NSOMEs to those who did not, it was found that relatively fewer respondents who were non-users agreed with the assumptions of NSOMEs and there were three assumptions with which none of the non-users agreed: use of NSOMEs was supported by research literature; dividing complex articulatory gestures is an efficient method to treat SSDs; and treatment effect of NSOMEs will carry over to speech productions. However, relatively more respondents, regardless whether they were users of NSOMEs or not, agreed with the assumption that speech develops from early oral behaviours. As reviewed above and in previous literature (see, e.g., Lof & Watson, 2008, 2010), the neural representation is task-specific; hence, early nonspeech behaviours are not likely to generalize to later speech development. The present findings provided useful information for the planning of the content of future SLT education and continuous professional education. JCSLS Vol. 21 2014 © IASLT/TCD/UCC Opinions regarding the benefits of NSOMEs This study found that over 60% of the respondents used NSOMEs to achieve five claimed benefits; whereas Lof and Watson (2008) reported 10 benefits and JCSLS Vol. 21 2014 © IASLT/TCD/UCC 26 Use of Nonspeech Oral Motor Exercises Hodge et al. (2005) reported three. Enhancing the clients’ awareness of the articulators is the one that was considered as a benefit of NSOMEs by many respondents in the present study and the two previous studies (Hodge et al., 2005; Lof & Watson, 2008). Moreover, the respondents in this study and the one by Lof and Watson found NSOMEs useful for achieving tongue elevation, jaw stabilization, and drooling control. The respondents in the current study also found NSOMEs useful for feeding, while this was not reported in the other two previous studies (Hodge et al., 2005; Lof & Watson, 2008). According to Lof and Watson (2008), their respondents also found NSOMEs useful for attaining tongue and lip strength, lateral tongue movements, tongue and lip protrusion, velopharyngeal competence, and sucking ability. The respondents in Hodge et al.’s study found NSOMEs useful for improving strength and/or coordination of articulators and increasing intelligibility. Familiarity with research and theory related to NSOMEs This study found that over 50% of the respondents, regardless of whether they had used NSOMEs or not, indicated that they were familiar with research and theory related to NSOMEs. The main difference between the users and non-users of NSOMEs was that none of the respondents who had used this treatment indicated that they were very unfamiliar with the topic; whereas none of the respondents who had not used this treatment indicated that they were very familiar with the topic. The present findings are generally congruent with the results reported by Lof and Watson (2008) where they reported a mean rating of 3.05 (rated on a 4-point scale where 4 means very familiar) regarding the respondents’ familiarity with research that investigated the efficacy of NSOMEs and a mean rating of 2.74 for the theoretical basis that supports the use of NSOMEs. SLTs’ use of speech therapy techniques for SSDs In general, the speech therapy techniques for SSDs that were used frequently by most clinicians in Ireland were similar to those reported in previous studies conducted in other countries (Brumbaugh & Smit, 2013; Joffe & Pring, 2008; McLeod & Baker, 2014) – minimal pairs and phonological/phonemic awareness approach were the most frequently-used therapy techniques. JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 27 Limitations of the present study As stated above, a weakness of the current study is the low number of respondents. The low number of responses was likely to be a consequence of the limitations in the method of distributing the questionnaire. For example, in the two surveys conducted in the US, the investigators had access to the American Speech-Language-Hearing Association (ASHA) membership database (Brumbaugh & Smit, 2013; Lof & Watson, 2008) and the survey carried out in Canada (Hodge et al., 2005) was distributed to all registered SLPs in Alberta through the Alberta College of Speech-Language Pathologists and Audiologists (ACSLPA). Although messages about the present survey were made available to all IASLT members through the Association on their website and social media pages (Facebook and Twitter), members who were not users of those social media websites or those who do not visit these websites regularly, and the practising SLTs who are not IASLT members were probably not aware of this study. This was reflected in the results that most of our respondents were relatively recent graduates, who were more likely to be active social media users. Another limitation of the present survey is that it did not ask the respondents directly why they chose to use NSOMEs with their clients. Although the answers to some of the questions (e.g., how NSOMEs were used, from where the respondents learned about this treatment, and the sources of information that influenced them the most regarding using NSOMEs) provided some insights on the reasons for using NSOMEs, it would have been useful if an open question on why NSOMEs were used was included in the questionnaire. Clinical implications of the present findings The present study showed that 56% (22 out of 39 respondents) reported using NSOMEs in their clinical practice despite the lack of evidence that supports the efficacy of this treatment approach. The treatment was still used mostly with children with childhood apraxia of speech, dysarthria, and Down Syndrome and often as a “warm up”. One clinical implication of the present findings is that we should continue our efforts in educating our students (SLT-intraining) and bring the attention of practising clinicians to the importance JCSLS Vol. 21 2014 © IASLT/TCD/UCC 28 Use of Nonspeech Oral Motor Exercises Use of Nonspeech Oral Motor Exercises of applying evidence-based practice in clinics. This could be achieved by ensuring that relevant topics are covered in the SLT curriculum, as well as providing continuous education offerings where SLTs are given access to valid sources of information or literature concerning the theory and efficacy of NSOMEs. This suggestion is feasible and very likely to be useful, as this study revealed that literature and professional training were the important factors that could influence clinicians’ practice. In addition, future continuous professional education could also include courses or talks on other speech therapy techniques with which efficacy have been established in the literature, so that clinicians are equipped with a wider range of techniques for managing clients, especially those with complicated speech problems. Another clinical implication is the need of well-designed treatment studies for answering the question regarding the efficacy of NSOMEs. As shown in the recent systematic reviews (Lass & Pannbacker, 2008; Lee & Gibbon, 2015; McCauley et al., 2009; Ruscello, 2008), the current evidence on the efficacy of NSOMEs comes mainly from small-scale controlled studies that were associated with a number of serious methodological limitations. For example, Lee and Gibbon (2015) found three NSOMEs treatment studies: two did not find combined NSOMEs and conventional articulation and/or phonological therapy to be more effective than conventional articulation and/or phonological therapy alone; and one study reported changes (possibly improvement) in articulation after the combined NSOMEs and speech therapy. However, the inappropriate statistical test used and the ambiguous presentation of results made it impossible to draw any meaningful conclusions regarding the efficacy of NSOMEs. Hence, at present, clinicians should be aware that there is no strong evidence of treatment efficacy of NSOMTs (Lee & Gibbon, 2015) and that they should use other speech therapy techniques for which the efficacy has already been established in the literature (McCauley et al., 2009). Acknowledgements The authors would like to thank Gregory Lof and Maggie Watson for their useful suggestions on the development of the questionnaire and the speech and language therapists-in-training who provided helpful feedback on the initial version of the questionnaire. Sincerest thanks also go to the Irish Association of Speech and Language Therapists and the speech and language JCSLS Vol. 21 2014 © IASLT/TCD/UCC 29 therapy managers of SLT services in southern Ireland for distributing the questionnaire. Lastly, the authors are most grateful to the speech and language therapists who had taken the time to participate in this study. The paper was based on a final-year honours project titled “The use of nonspeech oral motor exercises in the treatment of developmental speech sound disorders by speech and language therapists in the Republic of Ireland” by Niamh Moore (the second author), University College Cork, Ireland, 2014. References Bowen, C. (2005). What is the evidence for oral motor therapy? ACQuiring Knowledge in Speech, Language and Hearing, 7, 144–147. Brumbaugh, K.M. & Smit, A.B. (2013). Treating children ages 3–6 who have speech sound disorder: A survey. Language, Speech, and Hearing Services in Schools, 44, 306–319. Hodge, M., Salonka, R. & Kollias, S. (2005, November). Use of nonspeech oral-motor exercises in children’s speech therapy. Paper presented at the 2005 ASHA (American Speech-Language-Hearing Association) Convention, San Diego. International Expert Panel on Multilingual Children’s Speech. (2012). Multilingual children with speech sound disorders: Position paper. Bathurst, NSW, Australia: Research Institute for Professional Practice, Learning and Education (RIPPLE), Charles Sturt University. Retrieved from http://www.csu.edu.au/research/multilingualspeech/position-paper Joffe, V. & Pring, T. (2008). Children with phonological problems: A survey of clinical practice. International Journal of Language & Communication Disorders, 43, 154–164. Lass, N.J. & Pannbacker, M. (2008). The application of evidence-based practice to nonspeech oral motor treatments. Language Speech and Hearing Services in Schools, 39(3), 408–421. Lee, A.S.-Y. & Gibbon, F.E. (2015). Non-speech oral motor treatment for developmental speech sound disorders in children. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No.: CD009383. DOI: 10.1002/14651858.CD009383.pub2. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 30 Use of Nonspeech Oral Motor Exercises Use of Nonspeech Oral Motor Exercises Lof, G.L. (2003, April). Oral motor exercises and treatment outcomes. Perspectives on Language Learning and Education, 10(1), 7–11. Appendix Lof, G.L. (2006, November). Logic, theory and evidence against the use of non-speech oral motor exercises to change speech sound productions. Paper presented at the 2006 ASHA (American Speech-Language-Hearing Association) Convention, Miami Beach, USA. Questionnaire Lof, G.L. (2007, November). Reasons why non-speech oral motor exercises should not be used for speech sound disorders. Paper presented at the 2007 ASHA Convention, Boston, USA. Lof, G.L. (2009a, November). Non-speech oral motor exercises: An update on the controversy. Paper presented at the 2009 ASHA Convention, New Orleans, USA. Lof, G.L. (2009b). The nonspeech-oral motor exercise phenomenon in speech pathology practice. In C. Bowen (Ed.), Children’s Speech Sound Disorders (pp. 180–184). West Sussex: Wiley-Blackwell. Lof, G.L. & Watson, M. (2010). Five reasons why Nonspeech Oral Motor Exercises (NSOME) do not work. Perspectives on School-Based Issues, 11, 109–117. Lof, G.L. & Watson, M.M. (2008). A nationwide survey of nonspeech oral motor exercise use: Implications for evidence-based practice. Language, Speech & Hearing Services in the Schools, 39, 392–407. Marshalla, P. (2000). Oral-motor Techniques in Articulation and Phonological Therapy. Kirkland, WA: Marshall Speech and Language. McCauley, R.J., Strand, E., Lof, G.L., Schooling, T. & Frymark, T. (2009). Evidence-based systematic review: Effects of nonspeech oral motor exercises on speech. American Journal of Speech-Language Pathology, 18(4), 343–360. McLeod, S. & Baker, E. (2014). Speech-language pathologists’ practices regarding assessment, analysis, target selection, intervention, and service delivery for children with speech sound disorders. Clinical Linguistics & Phonetics, 28(7–8), 508–531. Pallant, J. (2005). SPSS Survival Manual: A Step by Step Guide to Data Analysis using SPSS for Windows (Version 12) (2nd ed.). Maidenhead, Berkshire: Open University Press. Rosenfeld-Johnson, S. (2001). Oral-motor Exercises for Speech Clarity. Tucson, AZ: Innovative Therapists. Ruscello, D.M. (2008). Treating Articulation and Phonological Disorders in Children. St. Louis, MO: Mosby Elsevier. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 31 The first box shows the first page of the online questionnaire where consent from the each respondent was obtained, and the second box shows the second page which was displayed after the respondents had clicked on the “next” button. The second page gives the definition of nonspeech oral motor exercises and instructions on completing the questionnaire. The content of the entire questionnaire follows. A Questionnaire on the Use of Nonspeech Oral Motor Exercises in Ireland Department of Speech and Hearing Sciences University College Cork Please read the following statements carefully. Please click the “next” button at the bottom of this page if you agree with these statements; this will constitute as your willingness to participate. “I am a Speech and Language Therapist who has worked or works with developmental speech sound problems in the Republic of Ireland. I have read the information sheet of this study (sent to me by email). I am aware of the aims of this research study and I know that I can ask questions if I want to. I am also aware that my participation is completely voluntary and that I can withdraw from the study at any time without consequence. In addition, I am aware that my participation in this study and the information I give will be kept completely confidential.” Nonspeech oral motor exercises are defined as any exercise that does not require the child to produce a speech sound but is used to influence the development of speech abilities. Part A must be completed by all participants. Part B must be completed only by participants who use nonspeech oral motor exercises. Part C must be completed only by participants who do not use nonspeech oral motor exercises. Part D must be completed by all participants. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 32 Use of Nonspeech Oral Motor Exercises PART A: DEMOGRAPHIC INFORMATION Part A must be completed by all participants. Enter the year each of your degrees were obtained (leave it blank if it does not apply): Masters Phd Other Bachelors Enter the name(s) of the county/counties in which you are working: Enter the percentage of time you work at each of the following settings. The total should add up to 100%: Language Class in School Community Care Hospital Disability Services Private Practice Other Tick the number of years you have worked with children with speech sound problems: 1-5 years 6-10 years 11-15 years 15-20 years More than 20 years Tick the total number of children currently on your caseload: 1-10 11-20 21-30 31-40 41-50 51-60 61-70 More than 71 Among the children currently on your caseload, tick the total number of children receiving services for some type of speech sound disorders: 1-10 11-20 21-30 31-40 41-50 51-60 61-70 More than 71 PART B: YOUR USE OF NONSPEECH ORAL MOTOR EXERCISES Part B must be completed only by participants who use nonspeech oral motor exercises. 1a. I was taught to use nonspeech oral motor exercises during my Speech and Language Therapy training (lectures/tutorials). Yes No 1b. I was taught to use nonspeech oral motor exercises during my Speech and Language Therapy training (clinical placement). Yes No 1c. I have observed improved speech production skills as a result of using nonspeech oral motor exercises. Yes No 1d. I have observed improved nonspeech oral motor skills as a result of using nonspeech oral motor exercises. Yes No JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 33 1e. I use nonspeech oral motor exercises as I have found that other types of speech elicitation exercises did not work for some of my clients. Yes No 1f. A colleague informed me about the usefulness of nonspeech oral motor exercises. Yes No 1g. I have attended continuing education offerings, workshops, and/or in-services on the use of nonspeech oral motor exercises. Yes No 1h. I have read literature (e.g. journal articles, book chapters) that encourages the use of nonspeech oral motor exercises. Yes No 1i. I have read internet sources (e.g. websites, blogs) that encourage the use of nonspeech oral motor exercises. Yes No In relation to Question 1 above, which TWO sources of information have influenced you the most regarding your use of nonspeech oral motor exercises? Please put the question numbers in the boxes below. 3a. The development of intelligible speech requires the use of separate oral motor tasks. Strong Agree Agree Neutral Disagree Strongly Disagree 3b. Children with speech sound disorders frequently lack the strength necessary to produce intelligible speech. Strong Agree Agree Neutral Disagree Strongly Disagree 3c. Speech develops from early oral behaviours, such as sucking or chewing. Strong Agree Agree Neutral Disagree Strongly Disagree 3d. Oral motor exercises serve as a groundwork for the development of more sophisticated motor movements necessary for speech production. Strong Agree Agree Neutral Disagree Strongly Disagree 3e. The use of nonspeech oral motor exercises for treating speech sound disorders is supported by the research literature. Strong Agree Agree Neutral Disagree Strongly Disagree 3f. Dividing the complex behaviours of speech into component oral motor movements is an efficient method to treat speech sound disorders. Strong Agree Agree Neutral Disagree Strongly Disagree 3g. Muscle movements for nonspeech oral tasks will carry over to muscle movements for speech sound productions. Strong Agree Agree Neutral Disagree Strongly Disagree 4a. Indicate how often you use nonspeech oral motor exercises with children with phonological disorders. Usually Often Sometimes Never JCSLS Vol. 21 2014 © IASLT/TCD/UCC 34 Use of Nonspeech Oral Motor Exercises 4b. Indicate how often you use nonspeech oral motor exercises with children with Childhood Apraxia of Speech. Usually Often Sometimes Never 4c. Indicate how often you use nonspeech oral motor exercises with children with Dysarthria. Usually Often Sometimes Never 4d. Indicate how often you use nonspeech oral motor exercises with children with Functional Articulation Disorders. Usually Often Sometimes Never 4e. Indicate how often you use nonspeech oral motor exercises with children with Structural Anomalies (e.g. cleft palate). Usually Often Sometimes Never 4f. Indicate how often you use nonspeech oral motor exercises with children with Down Syndrome. Usually Often Sometimes Never 4g. Indicate how often you use nonspeech oral motor exercises with children who are “late talkers”. Usually Often Sometimes Never 4h. Indicate how often you use nonspeech oral motor exercises with children with hearing impairment. Usually Often Sometimes Never 4i. Name other client groups with which you are nonspeech oral motor exercises and indicate how often you use nonspeech oral motor exercises with these groups (usually or sometimes). 5a. Nonspeech oral motor exercises often involve various materials. How often do you use horns in nonspeech oral motor exercises? Usually Often Sometimes Never 5b. How often do you use balloons in nonspeech oral motor exercises? Usually Often Sometimes Never 5c. How often do you use tongue depressors in nonspeech oral motor exercises? Usually Often Sometimes Never 5d. How often do you use straws in nonspeech oral motor exercises? Usually Often Sometimes Never 5e. How often do you use bite sticks or bite blocks in nonspeech oral motor exercises? Usually Often Sometimes Never JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 35 5f. How often do you use brushes in nonspeech oral motor exercises? Usually Often Sometimes Never 5g. How often do you use whistles in nonspeech oral motor exercises? Usually Often Sometimes Never 5h. How often do you use kazoos in nonspeech oral motor exercises? Usually Often Sometimes Never 5i. How often do you use Facial Flex in nonspeech oral motor exercises? Usually Often Sometimes Never 5j. Name any other materials you use for nonspeech oral motor exercises and state how often you use them (usually or sometimes). 6a. Nonspeech oral motor exercises often involve a variety of procedures. How often do you use whistling in nonspeech oral motor exercises? Usually Often Sometimes Never 6b. How often do you use pucker-smile alternations in nonspeech oral motor exercises? Usually Often Sometimes Never 6c. How often do you use tongue “push-ups” in nonspeech oral motor exercises? Usually Often Sometimes Never 6d. How often do you use tongue lateralizations (wags) in nonspeech oral motor exercises? Usually Often Sometimes Never 6e. How often do you use tongue curling in nonspeech oral motor exercises? Usually Often Sometimes Never 6f. How often do you use tongue grooving in nonspeech oral motor exercises? Usually Often Sometimes Never 6g. How often do you use cheek puffing in nonspeech oral motor exercises? Usually Often Sometimes Never 6h. How often do you use tongue to nose and tongue to chin movements in nonspeech oral motor exercises? Usually Often Sometimes Never 6i. How often do you use jaw lateral and vertical movements in nonspeech oral motor exercises? Usually Often Sometimes Never 6j. How often do you use blowing (e.g. cotton balls) in nonspeech oral motor exercises? Usually Often Sometimes Never 6k. How often do you use “big smile” exercises in nonspeech oral motor exercises? Usually Often Sometimes Never JCSLS Vol. 21 2014 © IASLT/TCD/UCC 36 Use of Nonspeech Oral Motor Exercises 6l. How often do you use exaggerated lip licking in nonspeech oral motor exercises? Usually Often Sometimes Never 6m. How often do you use kiss blowing in nonspeech oral motor exercises? Usually Often Sometimes Never 6n. Name any other procedures you use for nonspeech oral motor exercises and state how often you use them (usually or sometimes). Please tick one box below to select which of the four options best defines your use of nonspeech oral motor exercises (NSOMEs) when working with children who have speech sound disorders: I almost restrict my sessions to NSOMEs. When the client reaches a set criterion I stop using NSOMEs. I divide therapy time equally between NSOMEs and targeting speech productions. I use NSOMEs as a “warm up”. 8a. How familiar are you with research that has investigated the effectiveness of using nonspeech oral motor exercises. Very familiar Familiar Neutral Unfamiliar Very unfamiliar 8b. How familiar are you with the relationship between nonspeech oral motor exercises and the development of speech. Very familiar Familiar Neutral Unfamiliar Very unfamiliar 8c. How familiar are you with the theory related to nonspeech oral motor skills and the relationship to speech. Very familiar Familiar Neutral Unfamiliar Very unfamiliar 9a. How often do you use nonspeech oral motor exercises to improve lateral tongue movements? Usually Often Sometimes Never 9b. How often do you use nonspeech oral motor exercises to improve tongue protrusion? Usually Often Sometimes Never 9c. How often do you use nonspeech oral motor exercises to improve tongue strength? Usually Often Sometimes Never 9d. How often do you use nonspeech oral motor exercises to improve lip protrusion? Usually Often Sometimes Never 9e. How often do you use nonspeech oral motor exercises to improve lip strength? Usually Often Sometimes Never 9f. How often do you use nonspeech oral motor exercises to improve tongue elevation? Usually Often Sometimes Never JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 37 9g. How often do you use nonspeech oral motor exercises to improve jaw stabilization? Usually Often Sometimes Never 9h. How often do you use nonspeech oral motor exercises to improve sucking ability? Usually Often Sometimes Never 9i. How often do you use nonspeech oral motor exercises to improve drooling control? Usually Often Sometimes Never 9j. How often do you use nonspeech oral motor exercises to improve movement of the frenulum? Usually Often Sometimes Never 9k. How often do you use nonspeech oral motor exercises to improve biting? Usually Often Sometimes Never 9l. How often do you use nonspeech oral motor exercises to improve velopharyngeal competence? Usually Often Sometimes Never 9m. How often do you use nonspeech oral motor exercises to improve client’s awareness of the articulators? Usually Often Sometimes Never 9n. How often do you use nonspeech oral motor exercises to improve swallowing? Usually Often Sometimes Never 9o. How often do you use nonspeech oral motor exercises to improve feeding? Usually Often Sometimes Never 9p. Name other areas you target using nonspeech oral motor exercises. Also state how often you use nonspeech oral motor exercises to improve these areas (usually or sometimes). I generally train caregivers to carry out nonspeech oral motor exercises as part of a home program. Yes No I generally train other professionals (e.g. teachers, Occupational Therapists, Physiotherapists) to carry out nonspeech oral motor exercises as part of a treatment program. Yes No I am of the opinion that nonspeech oral motor exercises can favour children of any age. Yes No PART C: YOUR OPINION ON THE USE OF NONSPEECH ORAL MOTOR EXERCISES Part C must be completed only by participants who do not use nonspeech oral motor exercises. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 38 Use of Nonspeech Oral Motor Exercises 1a. During my Speech and Language Therapy training I was taught to use nonspeech oral motor exercises. Yes No 1b. I have observed improved speech production skills as a result of using nonspeech oral motor exercises. Yes No 1c. I have observed improved nonspeech oral motor skills as a result of using nonspeech oral motor exercises. Yes No 1d. A colleague informed me about the usefulness of nonspeech oral motor exercises. Yes No 1e. I have attended continuing education offerings, workshops, and/or in-services on the use of nonspeech oral motor exercises. Yes No 1f. I have read literature (e.g. journal articles, book chapters) that encourages the use of nonspeech oral motor exercises. Yes No 1g. I have read internet sources (e.g. websites, blogs) that encourage the use of nonspeech oral motor exercises. Yes No In relation to Question 1 above, which TWO sources of information have influenced you the most regarding your opinion concerning nonspeech oral motor exercises? Please put the question numbers in the boxes below. 3a. The development of intelligible speech requires the use of separate oral motor tasks. Strong Agree Agree Neutral Disagree Strongly Disagree 3b. Children with speech sound disorders frequently lack the strength necessary to produce intelligible speech. Strong Agree Agree Neutral Disagree Strongly Disagree 3c. Speech develops from early oral behaviours, such as sucking or chewing. Strong Agree Agree Neutral Disagree Strongly Disagree 3d. Oral motor exercises serve as a groundwork for the development of more sophisticated motor movements necessary for speech production. Strong Agree Agree Neutral Disagree Strongly Disagree 3e. The use of nonspeech oral motor exercises for treating speech sound disorders is supported by the research literature. Strong Agree Agree Neutral Disagree Strongly Disagree 3f. Dividing the complex behaviours of speech into component oral motor movements is an efficient method to treat speech sound disorders. JCSLS Vol. 21 2014 © IASLT/TCD/UCC Use of Nonspeech Oral Motor Exercises 39 Strong Agree Agree Neutral Disagree Strongly Disagree 3g. Muscle movements for nonspeech oral tasks will carry over to muscle movements for speech sound productions. Strong Agree Agree Neutral Disagree Strongly Disagree 4a. How familiar are you with research that has investigated the effectiveness of using nonspeech oral motor exercises. Very familiar Familiar Neutral Unfamiliar Very unfamiliar 4b. How familiar are you with the relationship between nonspeech oral motor exercises and the development of speech. Very familiar Familiar Neutral Unfamiliar Very unfamiliar 4c. How familiar are you with the theory concerning nonspeech oral motor skills and the relationship to speech. Very familiar Familiar Neutral Unfamiliar Very unfamiliar I generally train caregivers to carry out nonspeech oral motor exercises as part of a home program. Yes No I generally train other professionals (e.g. teachers, Occupational Therapists, Physiotherapists) to carry out nonspeech oral motor exercises as part of a treatment program. Yes No PART D: THERAPY TECHNIQUES FOR SPEECH SOUND PROBLEMS Part D must be completed by all participants. Listed below are some techniques used in therapy for speech sound disorders. If you are not familiar with an approach then tick the “unfamiliar” box. If you are familiar with an approach, then place a tick in only one box to indicate how often you use the approach. Minimal pairs Usually use Often us Sometimes use Never use Unfamiliar Maximal pairs Usually use Often us Sometimes use Never use Unfamiliar Van Riper traditional approach for sound elicitation Usually use Often us Sometimes use Never use Unfamiliar Van Riper traditional approach for sound stabilization Usually use Often us Sometimes use Never use Unfamiliar Auditory bombardment/stimulation Usually use Often us Sometimes use Never use Unfamiliar Hodson’s cycles approach Usually use Often us Sometimes use Never use Unfamiliar Metaphon approach Usually use Often us Sometimes use Never use Unfamiliar JCSLS Vol. 21 2014 © IASLT/TCD/UCC 40 Use of Nonspeech Oral Motor Exercises Whole language approach Usually use Often us Sometimes use Never use Unfamiliar Motokinesthetic approach Usually use Often us Sometimes use Never use Unfamiliar Unfamiliar Phonemic awareness approach Usually use Often us Sometimes use Never use Unfamiliar Distinctive feature approach Usually use Often us Sometimes use Never use Unfamiliar Morphosyntactic approach Usually use Often us Sometimes use Never use Unfamiliar Sensory motor approach Usually use Often us Sometimes use Never use Unfamiliar Paired stimuli approach Usually use Often us Sometimes use Never use Unfamiliar Other (name any other approaches you use and state how often you use them [usually, often, sometimes]) A Qualitative Exploration of Maternal Perspectives on the Impact of Stuttering on the lives of 6–10-year-old children Elizabeth Armstrong1, Mary-Pat O’Malley Keighran1, Patricia Collins2 and Clare Carroll1 1National University of Ireland, Galway, Ireland 2Health Service Executive, Shantalla, Galway, Ireland Correspondence to: Elizabeth Armstrong, Discipline of Speech and Language Therapy, School of Health Sciences, Aras Moyola, NUI Galway, Galway, Ireland Email: betharmstrong91@gmail.com Abstract Objective: The study aimed to explore maternal perspectives of the impact of stuttering on the lives of 6–10-year-old children’s relationships, self-identity, and academic development. Method: A qualitative design was used: five semi-structured interviews were conducted with mothers of children aged 6–10 years who stutter. The data was analyzed using thematic network analysis. Main results: While participants differed in their perceptions of the extent to which stuttering influenced their child’s life, all five discussed aspects of how their child’s relationships, self-identity and academic development had been impacted. Mothers described their child’s personal characteristics, their school environment, how their child communicated with family members and peers and how others related to their child. JCSLS Vol. 21 2014 © IASLT/TCD/UCC JCSLS Vol. 21 2014 © IASLT/TCD/UCC 42 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering Conclusion: The findings indicate that, when developing goals for therapy, speech and language therapists should consider how stuttering may be affecting a child in all areas of his/her life. An unexpected finding related to maternal stress levels associated with their child’s stuttering which may be an important variable to consider in treatment. The findings can inform clinical decision-making regarding treatment goals for children who stutter and their parents. Keywords: Stuttering, impact of stuttering on children, mothers’ perceptions, relationships, communication Background “Stuttering is like an iceberg, with only a small part above the waterline and a much bigger part below” (Sheehan, 1970, p. 184). There is little agreement amongst researchers regarding a description of stuttering and the emotions surrounding it, with some describing it as a primarily physiological entity and others in terms of its psychological or social limitations. Attempting to define stuttering is therefore problematic (Acton & Hird, 2004). For the purposes of this study, stuttering is described as a complex communication impairment which can obstruct the forward flow of speech and create negative emotions and reactions in both speakers and listeners (Guitar, 2006). A review of the literature suggests that, as well as communication difficulties, stuttering can affect an individual’s daily activities, relationships, mental health and educational or career choices (Craig, Blumgart & Tran, 2009; Enderby et al., 2009; Yaruss, 2010). Research exists regarding teenage (Zuckner, 2010) and preschool stuttering (Langevin, Packman & Onslow, 2010), with the age range of preschoolers differing slightly from country to country. Children between the ages of 6 and 10, the focus of the current study, have unique psychosocial, emotional and behavioural developmental patterns that differ from younger children and adolescents (Lau, Beilby, Byrnes & Hennessey, 2012). Family relationships A school-aged child’s primary relationships are with their parents, siblings, peers and teachers. The majority of parents in Langevin et al.’s (2010) study JCSLS Vol. 21 2014 © IASLT/TCD/UCC 43 believed stuttering had not influenced their relationship with their preschool child; however, these findings may not relate to older children. Children who stutter (CWS) have been found to be less attached to their parents than their non-stuttering peers (Beilby, 2014; Lau et al., 2012). Having a child who stutters can be stressful for parents and some experience guilt and find it difficult to cope, especially when stuttering first emerges (Goodhue et al., 2010; Plexico & Burrus, 2012). Parents may also perceive stuttering to have a greater effect on their child than does the child him- or herself (Cook & Howell, 2013). Beilby, Byrnes and Young (2012) found that approximately 50% of their sample of siblings of CWS reported that having a sibling who stuttered affected their relationship. Although many siblings reported having a strong bond and a protective role, participants also described instances of conflict due to perceived parental favouritism of CWS. They also reported their occasional frustration with or embarrassment about the CWS. While the study had a robust design and produced valuable findings, its sample size was small (n=12) and the researchers did not compare the experiences of younger siblings of CWS with those of older siblings. Siblings of CWS have also been reported to engage in teasing behaviours (Langevin et al., 2010). Peer relationships A child’s participation in social discourse may be disrupted by stuttering, and CWS often avoid communicatively difficult situations (Lau et al., 2012). Crichton-Smith’s (2002) study revealed strong themes of social limitations, beginning in childhood and continuing into adulthood. CWS are commonly affected by bullying (Klompas & Ross, 2004; Langevin & Narasimha Prasad, 2012) and are perceived by their peers to be less popular and are often rejected, even though educational systems have generally become more inclusive of children with disabilities (Davis, Howell & Cooke, 2002). But not all CWS are socially isolated. Hugh-Jones and Smith (1999) and Lau et al. (2012) found that some of their participants were outgoing and generally reported having enjoyable and supportive friendships, but the number and extent of friends was variable and limited, and many reported feelings of loneliness at school. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 44 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering School environment Unlike a preschool child whose main occupation is play, the school environment places greater emphasis on verbal communication and can be a communicatively demanding situation for CWS (Lau et al., 2012). Marshall, Ralph and Palmer (2002) found that few teachers felt competent to teach children with speech and language difficulties while Crichton-Smith (2002) notes that teachers can often have negative reactions to their students’ stuttering. Plexico, Plumb and Beacham (2013) found that a majority of teachers surveyed felt helpless or anxious when a child in their class stuttered and more than half reported having witnessed bullying of CWS. However, these findings should be interpreted cautiously as the study had a low response rate and those who did respond may have had a particular bias with regard to childhood stuttering. Nonetheless, it is likely that the response of teachers to a child’s stuttering impacts on the child’s ability to communicate and participate in classroom activities. O’Brian et al. (2011) found a significant negative association between stuttering severity and educational achievement, but did not ascertain the extent of its impact. Difficulties with reading for CWS are commonly discussed: Guitar (2006) notes that CWS often stutter more while reading than in spontaneous speech as they cannot alter their words, whilst Ardila et al. (1994) found that adults who stutter had significantly higher risks of having co-occurring dyslexia. Self identity Identity is described as the representation of oneself that emerges through participation with others across varying social contexts (Hagstrom & Daniels, 2004). Self identity is developed throughout the lifespan, and school-age children are beginning to form their identity (Daniels & Gabel, 2004; Lau et al., 2012). Although the relationship between stuttering and identity has been recently examined (Zuckner, 2010), there is little research specific to 6–10-year-old children. If a child’s communication is frequently interrupted by stuttering, he/she can start to experience associated negative emotions that may become part of their way of communicating and thus affect their self-identity (Hagstrom & Daniels, 2004). Similarly, Boey et al. (2009) found JCSLS Vol. 21 2014 © IASLT/TCD/UCC 45 that the majority of CWS were aware of their stutter and responded negatively to it. Vanryckeghem, Hylebos, Brutten and Peleman (2001) found that such negative emotions increased with age and stutter severity. Self-esteem refers to a person’s disposition to evaluate one’s self positively or negatively in a spontaneous, automatic or unconscious manner (Zuckner, 2010). Whilst Yovetich, Leschied and Flicht (2000) found that CWS, aged 7–11 years, indicated average to high levels of self-esteem, Anderson, Pellowski, Conture and Kelly (2003) found that they were often shy, quiet, cautious or fearful when confronted with unfamiliarity. Karrass et al. (2006) found that, when compared to non-stuttering peers, CWS were more reactive, less able to regulate their emotions and had poorer attention skills. However, Yaruss and Quesal (2004) argue that researchers have not devoted enough attention to the potential positives of having a stutter. Notably, Lau et al. (2012) found that some CWS are self-motivated to work towards achieving fluency. Current study Markham and Dean (2006) identified a link between speech and language disorders and children’s quality of life and recommended that future research should focus on specific clinical sub-groups, for example, CWS. By developing our understanding of the way stuttering can limit a child’s activities and their participation in society, clinicians may be better able to address the needs of CWS and their families in a more holistic manner (McCormack et al., 2010). Yaruss, Coleman and Quesal (2012) state that, by addressing a child’s entire experience of stuttering, clinicians can help children reduce its adverse educational and social impact. The choice of this research area and age cohort was informed by these recommendations and by the fact that much of the research regarding CWS comes from Australia (Langevin et al., 2010; Lau et al., 2012) and relates to preschool children of varying ages, when spontaneous recovery is common (Mansson, 2000). It was also influenced by an appreciation of the critical role of parents in the management of childhood speech and language impairments (Paul, 2007). Lau et al.’s (2012) study was particularly useful in shaping this research although it was not directly comparable as it used a quantitative and qualitative design and interviewed both CWS and their parents. Neither is it representative of the school-age population because of the sample size (n=20) and age JCSLS Vol. 21 2014 © IASLT/TCD/UCC 46 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering range (8–14 years). The current study sought to add to the evidence base by qualitatively exploring mothers’ perspectives on the impact of stuttering on the lives of children aged 6–10 years, in terms of their relationships, selfidentity and academic development. Method 47 medical conditions, hearing, cognitive, or speech and language impairments. Table 1 outlines the profile of the participants. The children’s ages ranged from 6–10 years, with a mean age of 8.6 years. The severity of the stutter was not assessed as the focus was on the perceived impact of the stutter on the child’s life rather than on its severity. Procedure Much research on stuttering has focused on experimental designs (Langevin et al., 2010; Vanryckeghem et al., 2001; Yovetich et al., 2000). Since human communication is complex and multi-dimensional, it is difficult to apply a quantitative framework to such research (Tetnowski & Damico, 2001). Qualitative methods focus on social phenomena which are fundamental in speech and language therapy (Damico & Simmons-Mackie, 2003). A qualitative methodology was therefore selected as it allowed the researchers to gather rich data from mothers of CWS. Participants Following purposive sampling, five mothers of children attending speech and language therapy for stuttering in a Health Service Executive (HSE) clinic in County Galway were recruited. The aim was not to generate a representative sample but to produce rich data for an in-depth exploration (Creswell, 2007). The inclusion criteria were parents who speak fluent English and had a child attending primary school who: had a primary stutter; was attending speech and language therapy; had been stuttering for at least a year; and had no other Table 1 Characteristics of parents and children. Participant number Participant characteristics Gender of child Age of child P1 P2 P3 P4 P5 Mother Mother Mother Mother Mother Male Male Male Male Male 8 6 10 9 10 JCSLS Vol. 21 2014 © IASLT/TCD/UCC The study used one-to-one, semi-structured interviews using a topic guide (see Appendix) with a flexible order and open-ended questions (Denscombe, 2010). Interviews are one of the most commonly recognized forms of qualitative research and are recommended when the researcher is interested in people’s perceptions (Mason, 2002). Ethical approval was granted by the ethics committees from both the University and the HSE. The SLT manager facilitated the first author to contact an SLT who acted as gatekeeper. The gatekeeper sent information sheets to potential participants who satisfied the inclusion criteria, inviting them to contact the first author. Five mothers gave their informed consent, and the interviews took place in a quiet clinic room to maximize their comfort and to ensure adequate audio-recording. To support the trustworthiness of the data, the first author checked with the participants during the interviews to ensure her understandings matched the participant’s intended meanings. The first author also minimized any verbal or non-verbal cues that might inadvertently influence the participants (Taylor, 2005). Data analysis was based on the principles of thematic network analysis (Attride-Stirling, 2001). Following completion of the interviews, they were transcribed verbatim by the first author to ensure accuracy, which allowed for a thorough examination of the utterances (Braun & Clarke, 2006). Themes were identified, extracted and refined from the coded text segments (AttrideStirling, 2001). Thematic networks were then built by selecting basic themes and rearranging them into organizing and global themes. This was achieved through repeated reading of the data in an active manner, seeking out meanings and patterns (Braun & Clarke, 2006) and exercising vigilance to minimize any predisposed biases in the interpretation of the results (Tetnowski & Damico, 2001). The first author analyzed the data in the first instance. The last author, with definitions of themes and supporting participant statements, facilitated JCSLS Vol. 21 2014 © IASLT/TCD/UCC 48 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering 49 verification of the thematic framework by using her insight and experience. This process verified that the description of the phenomenon was faithful (Koch & Harrington, 1998). The researchers ensured that confidentiality was maintained throughout with regard to participant anonymity and data storage. Results Ten basic themes emerged which were subsequently grouped into four organizing themes under a global theme of communication. This global theme relates to the act of communication and the context and circumstances in which it takes place. The thematic network is illustrated in Figure 1 and the organizing themes and their corresponding basic themes are then explored. Settings Parents spoke frequently about the different settings in which their child interacted and, in particular, about situations which depended on a high level of communicative skill. Figure 1 The thematic network Home environment JCSLS Vol. 21 2014 © IASLT/TCD/UCC One mother commented on her busy household which she feels is impacting on her child’s stuttering severity: “Nobody can get a word in, and least of all myself sometimes” (P2). She also described how she and her husband strive to create a relaxed environment: “We’ve tried to kind of keep you know dinnertime calm” (P2). This idea was mirrored by two other participants, one of whom stated that they “always try to be more relaxed around him” (P5) and another who ensures that her children do not talk over each other: “just make sure that they all get turns” (P1). School life One mother commented that her son was “very bright” (P4). While none of the participants perceived that stuttering was affecting their child’s general academic performance, current or past difficulties with reading were commonly JCSLS Vol. 21 2014 © IASLT/TCD/UCC 50 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering discussed: “He was really bad with the reading” (P3). One mother said her son’s teacher only occasionally noticed his stuttering and another said that her son’s speech was quite fluent at school: “He was able to stand up in school and give his news without anything really” (P2). One mother described how her son’s teacher was enthusiastic about helping him to achieve fluency: “They do anything they can to help him, they’re really good” (P3). Another described how her son stuttered mostly when he was talking to adults as he got nervous in those situations. Communicatively challenging situations Parents described how their child typically reacted when they were confronted with situations that were communicatively challenging, such as speaking in front of the class, talking to people they were unfamiliar with, or when they got excited: “It would come if he was coming home from school and wanted to tell me a lot of things” (P1). Three participants explained how their child had a part in their school play, whilst one described her son’s disappointment when he did not get a speaking part. Another described how her child was limited by his stutter, often refusing to communicate in situations which were dependent on fluent speech. “He wouldn’t go into a shop and ask for something” (P3). Relationships Participants’ perception of their child’s relationships emerged as a strong theme. Some described close relationships whilst others explained how the stutter hindered the child’s ability to form close relationships. Friendships Three of the participants noted that their child had many different friends and that stuttering did not affect their friendships: “He has a lot of friends; he’d have no problem going up and making friends with somebody” (P4). One mother described how her son’s friends at school tended to help him out if he was stuttering: “They’ll let him speak or they’ll finish his sentence for him but he doesn’t mind that because they’re all good friends” (P3). Another felt JCSLS Vol. 21 2014 © IASLT/TCD/UCC 51 her son did not have a lot of friends and tended not to initiate friendships: “they’d probably have to come to him now first” (P5). However, she related this to his personality rather than his stutter: “he’d be shy, quiet kind of...wouldn’t be very outgoing” (P5). Family Most participants described how their child had positive relationships with their siblings and felt stuttering did not explicitly affect that relationship: “they’d be very close” (P1). Two participants mentioned occasional disagreements but they regarded this as normal sibling behaviour. Another mother described how siblings would get frustrated if it took the child a long time to get his message across: “they don’t make fun of him, they’ll just say ‘oh spit it out” (P2). Another said her son would not stay at his grandparents’ house without his parents “in case they try making conversation” (P3). Most participants spoke of having a close relationship with their son. One mother said: “I suppose I would be looking out for him more” (P1), while another described how her son “felt worse for me than he did for himself ” (P3) as he was conscious that his stuttering upset her. Behaviour and reaction of others Two mothers described how their son’s peers commented on their speech: one said: “Someone said to him that he has ‘bumpy talk’” (P1), while another believed that her son’s peers “don’t really notice the stuttering” or had never “made it out to be a bad thing” (P4). A common subject discussed related to bullying although, with one exception, participants believed their child had never been bullied. One participant described how her son’s friends often “answer for him” or “finish his sentences” but she believed “it doesn’t faze him” (P2). Another commented on how she thought other adults perceived her child’s stuttering: “people kind of think it’s cute” (P4). Child’s characteristics This theme incorporated participants’ views of their child’s personality, how he felt about himself and activities he enjoyed. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 52 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering Personality and self-identity Although there were some similarities, the participants generally differed in their perceptions of their child’s personality, with words such as ‘outgoing’ (P1, P2, P3) ‘confident’ (P1, P2) ‘active’ (P4), ‘messer’ (P4), ‘friendly’ (P3), ‘chatty’ (P3), ‘quiet’ (P5), ‘sensitive’ (P1, P4) and ‘good’ (P4) being used. With regard to the emergence of self-identity, one mother described how her son was becoming more self-aware of his stutter and beginning to notice others who stutter, including people on television, and said that he was “coming around to it” (P1). She told how her son, in response to his friend’s questions about his stutter, had explained: “I’ve bumpy talk and I’m going to speech therapy” and that “once he is confident it sort of overrides the speech” (P1). However, another described her son as “lacking in confidence” (P5) because of his stutter. The mother of the 6-year-old felt he didn’t notice his stuttering and it was not part of how he viewed himself (P2). This was especially clear when she described his delight at being given a narrator part in his school play. Hobbies Four mothers named sports and playing outside as their child’s favourite pastimes with two describing their sons as “very active” (P4, P1). One mother felt her child’s main hobby was playing computer games. None perceived that stuttering negatively impacted on their chosen activity with one mother noting that her child: “will never back out of things because of his stammer” (P5). 53 stutter: “He kind of gets mad… he says why am I like this?” (P5). Another stated that her son had previously told his SLT that he felt bad, embarrassed, did not feel confident and was afraid to ask questions (P3). One mother described her child’s acceptance of stuttering: “I think he kind of accepts it” (P1), while another described his frustration with it. Two mothers described what they perceived to be positive aspects of their child’s stuttering. One attributed her son’s sensitivity to children with disabilities to his own experience of stuttering, while another believed that stuttering gave her child “a bit of a focus” and “something to really work towards” (P4). She also described him as being brave and having character because of it. Mothers’ hopes and fears Many participants recognized their own feelings and their impact on their child’s reaction to his stuttering. Two commented on its early identification and intervention and how they hoped this would benefit their child in the long run. Some referred to the cause of their son’s speech difficulties and wondered if it was something they themselves had done or neglected to do: “Was it me, did I not do enough reading with him” (P1), while others recognized their own worries: “I just wonder as well myself... I suppose that’s just what a mother does” (P4). Each mother spoke about their hopes for their child’s future: “Hopefully there’ll be some improvements with him” (P4) and one expressed her concerns for her child’s transition to secondary school. Another commented on other people’s perception of her child: “When someone has a speech, like goes to speech therapy, they would kind of think, maybe they’re slow in other things” (P1). Emotions This theme encompassed the feelings associated with stuttering and included both the mothers’ emotions and those they attributed to their child. Child’s response to stuttering Three participants felt their son did not notice the stuttering much or that it did not affect their daily lives: “The dysfluency doesn’t really bother him day to day” (P2). One mother believed her son sometimes felt angry because of his JCSLS Vol. 21 2014 © IASLT/TCD/UCC Discussion The study explored maternal perspectives on the impact of stuttering on the lives of their child in terms of their relationships, self-identity, and academic development. The data revealed a central theme of communication, with mothers perceiving that many different factors influenced their child’s stuttering. The results are discussed below under the organizing themes and are related to the literature. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 54 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering Relationships Most participants believed that stuttering is not negatively impacting on their child’s relationships within the immediate family. While these findings are at variance with Lau et al. (2012), who found that CWS were less attached to their parents, there is little other research specifically on parent–child relationships in CWS with which to compare them. The findings in relation to siblings, with all of the participants describing strong sibling bonds, are generally consistent with those of Beilby et al. (2012). Some described how siblings get frustrated or occasionally tease the child, similar to Langevin et al. (2010). However, participants felt this was normal sibling behaviour. Participants differed in their perceptions of how stuttering affected their child’s peer relationships, as reflected in the literature. Some felt their child found it easy to make friends (Lau et al., 2012), whilst others believed their child had relatively few friends (Hugh-Jones & Smiths, 1999). For some children, the fact that a peer finished sentences or said words for him was seen as an attempt to help him (Lau et al., 2012). Alternatively, it could reflect impatience with the time it takes him to speak. One mother believed her son’s shyness, rather than stuttering, was the main factor in his reluctance to initiate friendships. However, it could be argued that stuttering is contributing to his shyness, as found by Anderson et al. (2003). Notably, the mothers of the younger children believed that their friends were not aware or were not bothered, whereas friends of the older children tended to be more aware and to make comments. This finding reflects that of Langevin et al. (2010) and suggests that age may be an important variable. Although bullying was mentioned and is well documented in the literature (Klompas & Ross, 2004; Langevin & Narasimha Prasad, 2012), only one mother was aware that her child had been bullied. 55 suggesting they were less affected in the classroom. One mother commented on how her son’s speech was more fluent at school because of the structured classroom environment. These findings are rarely supported in the literature, as most studies have found that children perceive the classroom to be a demanding setting for communication (Lau et al., 2012). Each participant mentioned that their child had, or had at some stage, difficulties with reading. This is consistent with research on stuttering, reading and dyslexia (Ardila et al., 1994; Guitar, 2006). All participants felt their child had no other academic difficulties. There has been little research on academic achievement in CWS and further exploration is warranted to gain a better understanding of how CWS are impacted academically. Child’s characteristics Participants differed in their portrayal of their child’s personality, with some describing them as shy and sensitive (Anderson et al., 2003) and others as outgoing and confident (Yovetich et al., 2000). Similarly, not all believed that their child’s stuttering was a factor in his personality and self-identity. While the children differed in their favourite pastimes, they were not perceived to be limited in activities that they enjoyed, contrary to other findings (Yaruss, 2010). The results regarding the children’s perceived responses to potentially challenging communicative situations were also mixed. Some mothers described their child’s excitement at being involved in their school play, suggesting that these children have good self-esteem and did not view stuttering as a reason not to speak in public (Yovetich et al., 2000). Contrary to this, one mother stated that her child would not ask for something in a shop, suggesting that he anticipated difficulties with initiating such a request and that his stutter was emerging as a negative aspect of his self-identity. This idea is also discussed by Anderson et al. (2003). Settings Some mothers facilitated their child’s fluency by promoting a calm home environment, as described by Plexico and Burrus (2012). Although some commented on instances in which their child stuttered in class, most believed that stuttering was not negatively impacting on their school experience. Two participants felt that the teachers were not conscious of their child’s stuttering, JCSLS Vol. 21 2014 © IASLT/TCD/UCC Emotions In describing how their child felt about himself, some believed they did not notice or were not bothered by their stuttering, whilst others reported feelings of anger, embarrassment, fear and a lack of confidence. These latter findings are consistent with those of Vanryckeghem et al. (2001) and suggest JCSLS Vol. 21 2014 © IASLT/TCD/UCC 56 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering that these children had strong negative emotions about their stuttering and their ability to communicate. However, similar to Lau et al.’s (2012) study, one mother commented on her son’s acceptance of his stutter whilst others described their sons as being motivated to improve their speech, suggesting that not all children perceive their stutter in a negative light. Some mothers recognized their own feelings and behaviours surrounding stuttering; the fact that one believed her son felt worse for her than he did for himself suggests that, in this case at least, the stuttering had a greater impact on the mother than on the child. Some mothers experienced guilt and wondered if they had contributed to their child’s stuttering. This notion of guilt is also discussed by Goodhue et al. (2010). Strengths and limitations This study was conducted in a methodical manner, using reflexivity, and adhered to ethical standards. It had some limitations: principally, its sample size and make-up, and the data analysis could be further strengthened by a more rigorous peer review process. The findings need to be interpreted with caution as they are not representative of all mothers of all children who stutter. Each child involved was male, and the experiences of female children may be different (Zuckner, 2010). Some mothers were more articulate than others, resulting in disproportionate responses in some instances. The views of fathers or teachers were not sought. In addition, the participants’ descriptions of how they felt stuttering impacted their child’s life may not match how the children themselves perceive this, as parents can often perceive the psychosocial impact of stuttering to be greater than the child (Cook & Howell, 2013). While the first author established good rapport with the participants who related well to her, they may have been more relaxed in a location of their choice. Future research and clinical implications Further gender-specific research is required, using more representative and longitudinal studies to determine whether the impact that stuttering has on a child will change as they move into adolescence and adulthood. Future studies could also interview children themselves to see if their perceptions match those of their mothers. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 57 Craig, Blumgart and Tran (2009) found that stuttering negatively impacted on the emotional stability and mental health of adults who stutter. In light of this, the current findings highlight the need for families and clinicians to be aware of and monitor the potential psychosocial impact of stuttering and support the overall wellbeing of CWS. Yaruss (2010) recommends that evaluation of treatment should include more than just an assessment of changes in fluency. Depending on the age of the child and the severity of their stuttering, possible options include involving parents more in therapy sessions for this age group, therapists facilitating conversation within families about the role stuttering plays in their child’s everyday life, and identifying areas of particular difficulty. Effective strategies to help manage the child’s fluency at home highlighted by participants, for example, introducing turn-taking activities between siblings competing for speaking time, could be shared with parents. Children may also benefit from therapists liaising with their teachers and providing them with information and strategies to ensure the child achieves their maximum potential in the classroom. Conclusion The findings demonstrate that stuttering is a complex communication impairment which is difficult to define (Acton & Hird, 2004) and can manifest itself differently in children. Although generalisability was not the goal of the research, the findings suggest that stuttering has the potential to influence a child’s life in many different ways. Age and personality appear to be important factors in how CWS perceive themselves. As one parent put it: “different kids differ” (P1). It also demonstrates that, while SLTs should be aware of the potential for stuttering to have a negative impact on a child’s life, they should not assume that all children will perceive it as a negative factor in their self-identity. The study also suggests that SLTs should consider the emotional stress that parents of CWS may be struggling to deal with. Acknowledgements The work reported in this paper constituted a final year honours thesis by Elizabeth Armstrong, National University of Ireland, Galway. The authors JCSLS Vol. 21 2014 © IASLT/TCD/UCC 58 Maternal Perspectives on the Impact of Stuttering would like to sincerely thank each of the mothers who participated in the study. Declaration of interest The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The authors received no financial support for the research, authorship, and/or publication of this article. References Acton, C. & Hird, M.J. (2004). Toward a sociology of stammering. Sociology, 38, 495–513. Anderson, J.D., Pellowski, M.W., Conture, E.G. & Kelly, E.M. (2003). Temperamental characteristics of young children who stutter. Journal of Speech, Language & Hearing Research, 46, 1221–1233. Ardila A., Bateman, J.R., Nino, C.R., Pulido, E., Rivera, D.B., & Vanegas, C.J. (1994). An epidemiologic study of stuttering. Journal of Communication Disorders 27, 37–48. Attride-Stirling, J. (2001). Thematic Networks: An analytic tool for qualitative research. Qualitative Research, 1, 385–405. Beilby, J. (2014). Psychosocial impact of living with a stuttering disorder: Knowing is not enough. Seminars in Speech and Language, 35, 132–143. Maternal Perspectives on the Impact of Stuttering 59 Craig, A., Blumgart, E., & Tran, Y. (2009). The impact of stuttering on the quality of life in adults who stutter. Journal of Fluency Disorders, 34, 61–71. Creswell, J.W. (2007). Qualitative Inquiry and Research Design: Choosing among Five Approaches. London: Sage Publications. Crichton-Smith, I. (2002). Communicating in the real world: Accounts from people who stammer. Journal of Fluency Disorders, 27, 33–352. Damico, J.S. & Simmons-Mackie, N.N. (2003). Qualitative research and speech-language pathology: A tutorial of clinical realm. American Journal of Speech-Language Pathology, 12, 131–143. Daniels, D.E. & Gabel, R.M. (2004). The impact of stuttering on identity construction. Topics in Language Disorders, 24, 200–215. Davis, S., Howell, P., & Cooke, F. (2002). Sociodynamic relationships between children who stutter and their non-stuttering classmates. Journal of Child Psychology and Psychiatry, 43, 939–947. Denscombe, M. (2010). The Good Research Guide for Small-Scale Social Research Projects (4th ed.). New York: Open University Press. Enderby, P., Pickstone, C., John, A., Fryer, K., Cantrell, A., & Papaioannou, D. (2009). Royal College of Speech and Language Therapists: Resource manual for commissioning and planning services for SLCN. Retrieved from http://www. rcslt.org/speech_and_language_therapy/commissioning/aac_plus_intro Goodhue, R., Onslow, M., Quine, S., O’Brian, S. & Hearne, A. (2010). The Lidcombe Program of early stuttering intervention: Mother’s experiences. Journal of Fluency Disorders, 35, 70–84. Guitar, B. (2006). Stuttering: An Integrated Approach to its Nature and Treatment (3rd ed.). Baltimore: Lippincott Williams & Wilkins. Beilby, J.M., Byrnes, M.L., & Young, K.N. (2012). The experiences of living with a sibling who stutters: A preliminary study. Journal of Fluency Disorders, 37, 135–148. Hagstrom, F. & Daniels, D.E. (2004). Social identity and the stuttering experience. Contemporary Issues in Communication Science and Disorders, 31, 215–224. Boey, R.A., Van de Heyning, P.H., Wuyts, F.L., Heylen, L., Stoop, R., & De Bodt, M.S. (2009). Awareness and reactions of young stuttering children aged 2–7 years old towards their speech dysfluency. Journal of Communication Disorders, 42, 334–346. Hugh-Jones, S. & Smith, P.K. (1999). Self-reports of short- and long-term effects of bullying on children who stammer. British Journal of Educational Psychology, 69, 141–158. Braun, V. & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. Karrass, J., Walden, T.A., Conture, E.G., Graham, C.G., Arnold, H.S., Hartfield, K.N., & Schwenk, K.A. (2006). Relation of emotional reactivity and regulation to childhood stuttering. Journal of Communication Disorders, 39, 402–423. Cook, S. & Howell, P. (2013, September). Children’s and parents’ perspectives of psychosocial impact of stuttering and stuttering related bullying. Poster presented at the Stuttering Attitude Conference in Morganstown, West Virginia University. Klompas, M. & Ross, E. (2004). Life experiences of people who stutter, and the perceived impact of stuttering on quality of life: Personal accounts of South African individuals. Journal of Fluency Disorders, 29, 275–305. JCSLS Vol. 21 2014 © IASLT/TCD/UCC JCSLS Vol. 21 2014 © IASLT/TCD/UCC 60 Maternal Perspectives on the Impact of Stuttering Maternal Perspectives on the Impact of Stuttering 61 Koch, T. & Harrington, A. (1998). Reconceptualizing rigour: The case for reflexivity. Journal of Advanced Nursing, 28, 882–890. Tetnowski, J.A. & Damico, J.S. (2001). A demonstration of the advantages of qualitative methodologies in stuttering research. Journal of Fluency Disorders, 26, 14–42. Langevin, M. & Narasimha Prasad, N.G. (2012). A stuttering education and bullying awareness and prevention resource: A feasibility study. Language, Speech, and Hearing Services in Schools, 43, 344–358. Vanryckeghem, M., Hylebos, C., Brutten, G.J., & Peleman, M. (2001). The relationship between communication attitude and emotion of children who stutter. Journal of Fluency Disorders, 26, 1–15. Langevin, M., Packman, A., & Onslow, M. (2010). Parent perspectives of the impact of stuttering on their preschoolers and themselves. Journal of Communication Disorders, 43, 407–423. Yarrus, J.S. & Quesal, R.W. (2004). Stuttering and the International Classification of Functioning, Disability, and Health (ICF): An update. Journal of Communication Disorders, 37, 35–52. Lau, S.R., Beilby, J.M., Byrnes, M.L., & Hennessey, N.W. (2012). Parenting styles and attachment in school-aged children who stutter. Journal of Communication Disorders, 45, 98–110. Yarrus, J.S. (2010). Assessing quality of life in stuttering treatment outcomes research. Journal of Fluency Disorders, 35, 190–202. Mansson, H. (2000). Childhood stuttering: Incidence and development. Journal of Fluency Disorders, 25, 47–57. Yaruss, J.S., Coleman, C.E., & Quesal, R.W. (2012). Stuttering in school-age children: A comprehensive approach to treatment. Language, Speech and Hearing Services in Schools, 43, 536–548. Markham, C. & Dean, T. (2006). Parents’ and professionals’ perceptions of quality of life in children with speech and language difficulty. International Journal of Language and Communication Disorders, 41, 189–212. Marshall, J., Ralph, S., & Palmer, S. (2002). ‘I wasn’t trained to work with them’: Mainstream teachers’ attitudes to children with speech and language difficulties. International Journal of Inclusive Education, 6, 199–215. Yovetich, W.M.S., Leschied, A.W., & Flicht, J. (2000). Self-esteem of school-age children who stutter. Journal of Fluency Disorders, 25, 143–153. Zuckner, H. (2010). Self-esteem of 8–16 year old persons who stutter: Effects on speech behavior and therapy. Retrieved from http://www.ecsf.eu/userfiles/files/Zuckner%20 Selfesteem%20ECSF%20Ant%202010.pdf Mason, J. (2002). Qualitative Researching (2nd ed.). London: Sage Publications. McCormack, J., McLeod, S., Harrison, L.J., & McAllister, L. (2010). The impact of speech impairment in early childhood: Investigating parents’ and speech-language pathologists’ perspectives using the ICF-CY. Journal of Communication Disorders, 43, 378–397. O’Brian, S., Jones, M., Packman, A., Menzies, R., & Onslow, M. (2011). Stuttering severity and educational attainment. Journal of Fluency Disorders, 36, 86–92. Paul, R. (2007). Language Disorders from Infancy through Adolescence: Assessment and Intervention (3rd ed.). Missouri: Mosby Elsevier. Plexico, L.W. & Burrus, E. (2012). Coping with a child who stutters: A phenomenological analysis. Journal of Fluency Disorders, 37, 275–288. Plexico, L.W., Plumb, A.M., & Beacham, J. (2013). Teacher knowledge and perceptions of stuttering and bullying in school-age children. SIG 4 Perspectives on Fluency and Fluency Disorders, 23, 39–53. Sheehan, J.G. (1970). Stuttering: Research and Therapy. New York: Harper & Row. Taylor, M.C. (2005). Interviewing. In I. Holloway (Ed.), Qualitative Research in Health Care (pp. 39–55). Berkshire: Open University Press. JCSLS Vol. 21 2014 © IASLT/TCD/UCC Appendix Interview Topic Guide 1. Can you tell me a little bit about your child? 2. Can you tell me about his stuttering? 3. Could you tell me how you think stuttering affects him in his everyday life? ÎHow would you describe X’s relationship with the rest of the family? ÎAre his siblings aware of his stutter? ÎHow does his stuttering impact on his relationship with his brothers/sisters? ÎHow does he get on with the extended family? JCSLS Vol. 21 2014 © IASLT/TCD/UCC 62 Maternal Perspectives on the Impact of Stuttering Î How would you describe your relationship with X? Does having a stutter impact on this relationship? ÎDoes X make friends easily? If so, what makes it easy for him? If not, what makes it more difficult for him? ÎAre X’s friends aware of his stuttering? If so, how does this impact on their relationship? What’s in an Accent? Perceptions of Young Adult Listeners in Cork and Kilkenny ÎHow would you describe X’s personality? Nicola Bessell and Eimear Mulhall ÎHow do you think X feels about himself? Do you think having a stutter affects the way he feels about himself? University College Cork, Ireland ÎHow does X himself react to his stuttering? ÎDoes X ever get frustrated with himself when he stutters? How does he show this frustration? ÎWhat would X’s typical reaction to a new or different social situation be, such as somewhere where he has never been or involving people he has never met? ÎCan you tell me about how X is getting on in school? ÎWhat kind of relationship does he have with his teacher? ÎDoes X ever avoid situations where it may be difficult to communicate, e.g., talking in front of the class, reading aloud, presentations, speech and drama, etc? If so, how or why do you think this is? ÎDo you know if X has ever been bullied? If so, can you tell me a bit about it? ÎDo any of X’s friends ever try to help him out when he starts to stutter? How do they help? ÎAre there any aspects of having a stutter that have been positive for X? JCSLS Vol. 21 2014 © IASLT/TCD/UCC Correspondence to: Nicola Bessell, Department of Speech and Hearing Sciences, Brookfield Health Sciences Complex, College Road, Cork City, Co. Cork, Ireland Email: n.bessell@ucc.ie Abstract Objective: To investigate the perceptions of Irish listeners concerning geographical origin, occupation and socio-economic class, based on speech samples from County Cork; to relate this information to phonetic features of each speaker’s accent and recent changes in Irish English. Methods: Recordings of speakers from three locations in County Cork were analyzed for features of supra-regional and advanced Irish English (Hickey, 1998, 2003, 2010). These recordings were played to young adult listeners from counties Cork and Kilkenny. Listeners completed a questionnaire assessing the location, occupation and socio-economic class of each speaker. The results of the questionnaire were compared with the phonetic features of the speakers. Main results: Diphthongization of FACE and GOAT vowels, [θ, ð] for TH, GOOSE-fronting and emerging velarised /l/ in syllable final position tilt listener judgements towards non-regional, professional and upper middle class. Cork City listeners are most accurate in terms of locating Cork city speakers. Kilkenny listeners are least accurate in identifying speaker location. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 64 What’s in an Accent? Conclusions: Irish English speech varies depending on location and gender. Perceptions of class and occupation are closely tied to gender of speaker and type of phonetic features present. Supra-regional features are increasingly used by young adults in County Cork, and recognized by young adult listeners. Key words: Accent perception, Irish English, supra-regional Irish English, gender, socio-economic class. Introduction In Ireland, as in many countries, speaker accent can be a cue to geographical origin and social class (Hickey, 2004; McWilliams, 2005). Nonetheless, Hickey (1998, p. 83) notes that in the Republic “there is something like a supra-regional standard which is characterized by the speech of middle-class urbanites”. Features of this supra-regional standard include dental [t̪, d̪] in words with TH spellings, apical alveolar fricatives [θ͇, ð͇]1 for /t, d/ in certain positions, and clear /l/ in all syllable positions. Hickey (2010) notes that English as spoken in Ireland over the centuries has, for various reasons, moved away from some of its more conservative or Irish-influenced features. For instance, the early Middle English pronunciation of /u:/ has long been replaced by the diphthong /au/ in the MOUTH lexical set2, though this happened in Ireland later than in England. In this sense, supra-regionalization in Irish English has a long history, continuing in the 19th century with the introduction of compulsory primary education and the rise of an Irish middle class (Hickey, 2002). In the 20th century, the move to supra-regional norms accelerated during the so-called Celtic Tiger years (1990s to approximately 2005) and continues to the present day. This most recent wave of supra-regionalization 1 We follow Pandeli, Eska, Ball and Rahilly (1997) in using the IPA-based symbols [θ͇, ð͇] for the Irish English apical alveolar fricative pronunciation of the stop phonemes/t, d/. Hickey uses [ṱ, ḓ], which has the advantage of highlighting the allophonic relationship with /t, d/ . Kallen (2012) follows O’Baoill (1990) in using [t̞], which signifies a ‘lowered’ alveolar stop. This also preserves a relationship with /t/. 2 We follow the use of Wells’ lexical sets to identify vowel classes (Wells, 1982). Each lexical set, for example MOUTH, contains words that share the pronunciation of the key word. JCSLS Vol. 21 2014 © IASLT/TCD/UCC What’s in an Accent? 65 has brought some new features into Irish English. It is these features that are examined in this paper. Hickey terms this speech style New Dublin English (1998) and Advanced Dublin English (2005). Hickey (2010) argues that the driving force behind Advanced Dublin English is dissociation. He suggests that young workers coming to the booming capital in the 1990s wanted to dissociate from the distinct local Dublin vernacular as well as their own regional varieties of Irish English. These speakers developed phonetic cues that extended existing differences between educated mainstream Dublin speech and the local Dublin vernacular. These cues included a velarised /l/ in final position, fronting of the MOUTH diphthong from [aʊ] to [æʊ, ɛʊ], and the Dublin Vowel Shift (Hickey, 1998). The Dublin Vowel Shift involves retraction of /aɪ/ in PRIDE to [ɑɪ]3; raising of /ɒɪ/ in CHOICE to [ɔɪ, oɪ] and raising of the back vowels /ɒ, ɒː/ in COT and THOUGHT to [ɔ, ɔː]. Hickey (2003) notes that these advanced Dublin features were widespread throughout the south of Ireland by the early 2000s, particularly among young female speakers. O’Sullivan (2013) lends support for the increase in use of advanced Dublin features. She traced the use of these features in radio advertisements in the Republic of Ireland, noting their absence in data from 1977 and 1987, a minority presence in 1997 advertisements with mostly women using them, and an increased presence in 2007 with both men and women using the features. Cork city is the second largest city in the Republic, yet there is very little published information on Irish English as it is spoken in the city or in County Cork (Hickey, 2002). The county accent is generally known for its characteristic intonational patterns (Murphy, 1994; Hickey, 2011). Within Cork city there is a broadly recognized north/south accent distinction based on location relative to the River Lee, which runs through the city on an east–west axis. The population north of the river tends to use a strong vernacular and readily identifiable ‘North Cork’ accent. South of the river, the population in many areas uses a more standardized, middle-class accent, although there are certainly some areas with strong working-class affiliation south of the river. According to Frost (2000), the north-south accent divide in Cork city is better understood as an instance of more broadly-based class distinctions, 3 Hickey (2013) notes that this feature is receding from advanced Dublin English and it is not investigated in this study. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 66 What’s in an Accent? What’s in an Accent? 67 with a clear working-class accent spoken in north Cork and some locales south of the river, but overall a more prestigious middle-class accent spoken in most areas south of the River Lee. (See Haase and Pratschke (2012) and Pobal (2006) for demographic information on Cork City.) Currently, the extent of supra-regional and advanced Dublin features in County Cork and Cork city, and whether some features are more dominant than others, is known only anecdotally. Similarly, although perception and attitudes to language change have a role in the spread of innovative features, the perception of accents of any sort within Ireland is little investigated (but see Hickey, 2005). Very little is known about Cork speakers’ perceptions of local or non-local accents. To address these gaps, this paper analyzes data from male and female speakers from three different locations in and outside Cork city, and assesses the perceptions of young adult Irish listeners concerning the occupation, socio-economic class and regional origin of these speakers. Using this data, we investigate the relationship between perceived class, occupation and location on the one hand and the degree to which each speaker adopts the features of new Dublin English on the other. Method Participants Following similar research by Bayard, Weatherall, Gallois and Pittam (2001), two speakers aged 18–24 (one female, one male) from three different locations were recorded reading a short paragraph (see Figure 1 for maps detailing location of speakers). Speakers were chosen to be representative of the two major accents within Cork city, with Macroom speakers representing a relatively urban County Cork accent, thus avoiding the complicating factor of rural versus urban accents. To control for educational and socio-economic background, brother–sister pairings were recruited for Cork city south and Macroom, but were not available for Cork city north. Female and male listeners aged 18–19 were recruited from secondary schools in north Cork city (n=14), south Cork city (n=15), Macroom (n=17) and Kilkenny (n=17). There were 25 female listeners and 38 male listeners for a total of 63. JCSLS Vol. 21 2014 © IASLT/TCD/UCC Figure 1 Speaker locations within County Cork (top) and Cork City (bottom). JCSLS Vol. 21 2014 © IASLT/TCD/UCC 68 What’s in an Accent? Materials Speakers read a short paragraph designed to elicit a range of vowels, as well as specific consonantal features attested in supra-regional and advanced Dublin English, as summarized below. See Appendix 1 for text of recorded data. 1. Allophones of /t/ in initial, medial and final position, e.g., Tom, rainwater, boat. 2. Allophones of sounds spelled with TH, e.g., thought and breathe. 3. /l/ in medial and final position, e.g., leaf and feel. 4. Vowels in the following lexical sets FLEECE, e.g., meet TRAP, e.g., trap GOOSE, e.g., Bruce DRESS, e.g., instead MOUTH, e.g., mouth CHOICE, e.g., choice THOUGHT, e.g., thought FACE, e.g., rain GOAT, e.g., boat Procedure The speakers were recorded in a quiet room with an Audio Technica AT831b cardiod condenser microphone and a 24 bit digital recorder (Roland R-05), at a sampling rate of 44 kHz. To assess the representativeness of the speaker data, a colleague with personal and academic knowledge of Cork area accents evaluated the recordings. Recordings were then analyzed acoustically using broad band spectrograms and the formant tracking facilities in PRAAT JCSLS Vol. 21 2014 © IASLT/TCD/UCC What’s in an Accent? 69 (Boersma & Weenink, 2014). Following procedures in Labov, Ash and Boburg (2006), monophthongs were analyzed for first and second formant values (F1 and F2) taken at the F1 maximum. If no F1 maximum was achieved, then frequency readings for both formants were taken at the point of F2 maximum or minimum. If both formants were in transition throughout the duration of the vowel, frequency readings were taken at the temporal midpoint of the vowel. Diphthongs were measured for F1 and F2 values at one-third and twothirds of their duration. Vowel formant values were normalized and plotted using the Watt and Fabricius modified algorithm in NORM (Fabricius, Watt & Johnson, 2009; Thomas & Kendall, 2007). To assess clear and dark (velarized) /l/, formant readings were taken at the temporal midpoint of word-initial and word-final /l/. Spectrograms of /t/ were assessed visually and perceptually for stop, flap, glottal stop, fricative or deleted allophones. Productions of words spelled with TH were likewise visually and perceptually analyzed for realization as stops or fricatives. School principals in secondary schools were approached for permission to invite Year 6 students over the age of 18 to listen to the recordings and complete two questionnaires. Principals and participants were provided with information sheets and signed consent was obtained. On-site classroom computer and speaker systems were used to play the speech data. For each participant group, a trial run was conducted using non-test data and participants were instructed to listen to the accent of the speaker rather than the content of the recording. After one presentation of one speaker’s data, participants filled out a questionnaire assessing that speaker’s personal characteristics along three dimensions of competence, power and solidarity, as in Bayard, Weatherall, Gallois and Pittam (2001). These data are not reported on here. After listening to the recording a second time, participants completed a second questionnaire, assessing the speaker’s geographical location, occupation and social class. Participants wrote down where they thought the speaker was from and chose from four categories of occupational type (unskilled, semi-skilled, skilled, professional) and three categories of socio-economic class (lower, middle and upper class). Participants then listened to the next speaker and filled out questionnaires for that speaker. Speech samples were played in a random order until all six speakers had been assessed. Prior to recruiting participants, ethical approval was granted by the Clinical Research Ethics Committee of the Cork Teaching Hospitals. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 70 71 What’s in an Accent? What’s in an Accent? Results Allophones of /t/ A Cork native and linguist confirmed that both north Cork speakers had a recognizable Cork accent, the Macroom speakers less obviously so. Both south Cork speakers were considered ‘metropolitan’ Irish English speakers, meaning educated, middle class and lacking cues to region of origin. Our consultant placed the age of all speakers as under forty. Word initial /t/ for all speakers was a voiceless aspirated alveolar stop [th]. Medial /t/ had several allophones: a flap [ɾ] (NCF and SCM); an apico-alveolar fricative [θ͇] (SCF and MF); [th] (NCM) and an unaspirated [t] (MM). All speakers used [θ͇] for most final /t/s, with some speaker-specific variation depending on the following word context. For example, both North Cork speakers deleted the final /t/ in midnight, whilst both SCM and MM produced a weakly articulated voiced allophone [d͉] when the following word began with a vowel, as in sight of. Consonants The results of acoustic and perceptual analysis of /t/, /l/ and words spelled with TH are summarized in Tables 1 and 2. Speakers are referred to as: NCF (North Cork Female) and NCM (North Cork Male); SCF (South Cork Female) and SCM (South Cork Male); MF (Macroom Female) and MM (Macroom Male). Table 1 Production of /t/ and TH for all speakers Target Word initial /t/ Tom Word medial /t/ rainwater Word final /t/ midnight meet (an) boat sight (of) fight thought Word initial TH thought Word final TH mouth breathe Speakers NCF NCM SCF SCM MF MM th th th th th th ɾ th θ͇ ɾ θ͇ t Deleted* d θ͇ θ͇ θ͇ θ͇ Deleted* θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ d͉ θ͇ d͉ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ θ͇ d͉ θ͇ θ͇ th th θ t̪ʰ t̪ʰ θ Allophones of words spelled with TH Words with TH spellings have varied productions. Word–initially (in the word ‘thought’), both NC speakers produced an aspirated alveolar stop [tʰ]. SCM and MF produced an aspirated dental stop [t̪ʰ], whilst SCF and MM produced a fricative [θ], which may be dental or interdental. Final voiceless TH (in the word ‘mouth’) is reduced to glottal stop with a creaky preceding vowel [V̰ʔ] (North Cork speakers), weakly articulated [t͉ʰ] (MM) and voiceless fricative [θ] by the other three speakers. Final voiced TH (in the word ‘breathe’) is produced as a voiced alveolar stop with full, aspirated release [dʰ] by NCM and MF, but [ð] by all other speakers. Allophones of /l/ V̰ʔ ð * phoneme not produced JCSLS Vol. 21 2014 © IASLT/TCD/UCC V̰ʔ dʰ θ ð θ ð θ dʰ t͉h ð Two speakers (NCM and NCF) show no evidence of dark /l/, transcribed [ l̴]. Three speakers (SCF, SCM and MF) show a modest rise in F1 on final /l/, Table 2 F1 and F2 values for /l/ of all speakers. Formant values are in Hertz. Target Word initial /l/ leaf Word final /l/ feel F1 F2 F1 F2 NCF 453 1518 380 1660 NCM 342 1585 336 1669 Speakers SCF SCM 418 353 1917 1280 653 405 2061 1266 MF 402 1570 552 1601 MM 402 1501 397 1337 JCSLS Vol. 21 2014 © IASLT/TCD/UCC 72 What’s in an Accent? What’s in an Accent? 73 consistent with some tongue lowering. MM has some F2 lowering consistent with velarization, but no F1 rising. Vowels Figure 2 Scatterplot of vowel formant means for six speakers (NCF, NCM, SCF, SCM, MF, MM), normalized using modified Watt and Fabricius method and plotted using NORM (Thomas & Kendall, 2007). Figure 3 Scatterplot of vowel formant means for North Cork speakers normalized using modified Watt and Fabricius method and plotted using NORM (Thomas & Kendall, 2007). JCSLS Vol. 21 2014 © IASLT/TCD/UCC Figure 2 presents normalized vowel data for all speakers. Figures 3–5 present vowel plots for male and female pairs from each of the three locations of North Cork, South Cork and Macroom. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 74 What’s in an Accent? Figure 4 Scatterplot of vowel formant means for South Cork speakers, normalized using modified Watt and Fabricius method and plotted using NORM (Thomas & Kendall, 2007). JCSLS Vol. 21 2014 © IASLT/TCD/UCC What’s in an Accent? 75 Figure 5 Scatterplot of vowel formant means for Macroom speakers, normalized using modified Watt and Fabricius method and plotted using NORM (Thomas & Kendall, 2007). JCSLS Vol. 21 2014 © IASLT/TCD/UCC 76 What’s in an Accent? What’s in an Accent? 77 MOUTH fronting Location of speakers The MOUTH vowel was considered fronted if the onset F2 reading placed it in front of the central TRAP vowel. By this measure, two speakers (SCF and SCM) have strong MOUTH-fronting with an F2 onset in the region of the DRESS vowel, two speakers have minimal MOUTH-fronting (MF and NCF) and two speakers (MM and NCM) have no evidence of MOUTHfronting at all. Responses to location are grouped in terms of locations within North Cork (NC), South Cork (SC), Macroom/West Cork (M), and locations outside County Cork (OCC). Results are presented by listener group, starting with North Cork listeners. NC listeners assigned NC speakers to north Cork locations (90%) and SC speakers were mostly assigned to south Cork locations (69%). NC listeners assigned Macroom speakers predominantly to south Cork locations (69%). SC listeners produced a similar pattern, identifying NC speaker location with 87% accuracy, and SC speaker location with 81% accuracy. Like the NC listeners, SC listeners assigned Macroom speakers to SC locations (93%). Macroom listeners were less accurate in their assignment of correct location to NC (62%), SC (59%) and M speakers (25%), citing locations outside County Cork for all speakers. Kilkenny listeners placed virtually all speakers outside County Cork (94%). CHOICE raising The onset of CHOICE vowels was considered raised if its F1 value was higher than that of DRESS vowels. By this measure, both North Cork speakers and MM do not raise CHOICE, while both South Cork speakers and MF do. THOUGHT raising Using the same measure as with CHOICE raising, both North Cork speakers and male speakers MM, SCM do not raise THOUGHT. SCF and MF both raise THOUGHT. GOOSE fronting The GOOSE vowel falls into three clear categories. Both North Cork speakers have a mid-back vowel whose F2 value does not exceed that of TRAP, which is a central vowel. The Macroom speakers front GOOSE to almost exactly the F2 value of TRAP, producing a central vowel. The SC speakers both produce strongly fronted /u/. FACE and GOAT diphthongization FACE is a monophthong for three speakers: NCM, MF and MM. For all other speakers, it is a diphthong with endpoint approaching the MEET vowel (see Figures 3, 4, and 5). GOAT is a monophthong for NCM, MF; a wide diphthong for SCF and a narrower diphthong for NCF, MM and SCM. JCSLS Vol. 21 2014 © IASLT/TCD/UCC Class of speakers All four listener groups perceived NC speakers as mostly lower class (71%) with some middle-class perceptions (28%) mostly for NCF. All listener groups perceived SC speakers as mostly middle class (55%) or upper class (38%), especially for SCF. All listener groups perceived M speakers as mostly middle class (67%), with upper-class judgements (25%) mostly for MF. In general, females in all speaker groups received higher socio-economic rankings than the males. Occupation of speakers NC speakers are viewed by all listener groups as primarily unskilled (65% of listener responses), with some semi-skilled perceptions (24%), particularly from Macroom listeners. SC speakers are viewed by all listener groups as primarily skilled (45%), with some semi-skilled (18%), particularly for the male speaker, and some professional (28%), particularly for the female speaker. Macroom speakers were perceived by all listeners as mostly semi-skilled (37%) and skilled (26%) with professional (20%) for the MF only. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 78 What’s in an Accent? Discussion New Cork features4 Recent GOOSE-fronting is reported in varieties of British English (Jansen, 2010; Docherty, 2010; Wells, 1982), Ulster English (Kallen, 2012) and American English (Fridland, 2008). It is not reported for local Dublin English by Ferragne and Pellegrino (2010), nor for advanced Dublin English in Hickey’s (2005) work. However, fieldwork documents young speakers from the Cork area and Waterford with varying degrees of GOOSE-fronting (Bessell, 2013; fieldnotes) and acoustic analysis of some of Hickey’s advanced young Dublin speakers indicates GOOSE-fronting (Hickey, 2013). It is unlikely that this feature is confined to young speakers of any particular region, but acoustic documentation is sporadic. Diphthong realizations of FACE and GOAT are found in General American English and Canadian English, as well as Southern British English (Wells, 1982). Hickey (2004, p. 57) records [e:] and [oʊ, o:] as the Irish English supra-regional mainstream norm for these two vowels. Hickey (2013) notes GOAT-diphthongization in advanced Dublin speakers, but reiterates that FACE remains a monophthong. Ferragne and Pellegrino (2010, p. 23) note some FACE and GOAT diphthongs among the Dublin speakers in their survey. The more advanced supra-regional Munster English speakers recorded for this study tend to diphthongize both vowels. There is too little data to be certain that FACE or GOAT diphthongization are changes with a regional origin (Cork or Dublin) but, like GOOSE-fronting, these cues are increasingly used by young adult speakers. O hUrdail (1997) documents the wide use of dental [t̪, d̪] for TH spellings and Hickey (2004) notes that this is the supra-regional educated norm in Ireland. The production of fricatives for TH words is not reported for new Dublin English (Hickey, 2004, 2013), but in our experience a genuine fricative does occur in the conversational speech of some young adults, particularly 4 The term “new Cork” is used since this paper documents these particular features in the English of speakers from County Cork. If they are genuinely supra-regional features, which is highly likely, then a more accurate term might be “new supra-regional”. JCSLS Vol. 21 2014 © IASLT/TCD/UCC What’s in an Accent? 79 women, attending University College Cork. Kallen (2012) notes the use of affricates [t̪͡θ] and [d̪͡ð] outside of Ulster English. O hUrdail (1997) also comments that the dental stop pronunciation is often a focus in elocution and drama lessons, with fricatives being taught in their place. Students at UCC often report being taught the rhyme, “This, that, these, those, that’s the way the TH goes”, with emphasis on a fricative production, both at school and in drama lessons. This may be having some influence on the use of [θ, ð]. Whilst reading tasks such as the one used in this study may elicit more formal fricative productions of TH words, the current database does not allow us to assess this variable. What we term the “new Cork” features of GOOSE fronting, FACE/GOAT dipthongization and TH as fricatives are most frequent in the speech of SC speakers, with the following cline: SCF>SCM>MM>MF>NCF>NCM (see Figure 6). This distribution is very close to the pattern of class and occupation rankings from all listeners except that MF is usually ahead of MM. If new Dublin features are added to new Cork features, we get exactly the same distribution as the occupation and class rankings. From a linguistic point of view, it seems that perception of class and occupation is sensitive to the number of new Dublin and newer Cork features. Whilst our study adopted the class divisions used by Bayard et al. (2001) this may not be a good fit for the Irish population, which is commonly regarded as composed of working class and middle class (Convery, 2013). However, our occupation categories, which also follow Bayard et al. (2001), are close to the divisions used in modern demographic studies of Irish society, such as Pobal (2006). We note there is a great deal of similarity in participant judgements of occupation and class, and it may be that future studies could reference occupation alone. Despite the reasonably clear three-part grouping of speakers by accent features, location assessments by all County Cork listeners divide the speakers into two groups: north Cork city on the one hand; south Cork city and Macroom on the other. For NC and SC listeners, more regional features relative to supra-regional and new features mean a north Cork location and perceptions of lower class and less skilled professions. For the same listeners, supra-regional, new Dublin and new Cork features cue a south Cork location and perception of higher socio-economic class and occupation. Macroom listeners are less accurate and give a broader range of locations. For these JCSLS Vol. 21 2014 © IASLT/TCD/UCC 80 What’s in an Accent? What’s in an Accent? listeners, accent is not as reliable an indicator of location as it is for NC and SC listeners. Nonetheless, Macroom listeners perceive occupation and class in the same way as NC and SC listeners. Therefore, Macroom listeners must be relying on phonetic cues to class and occupation independent of the knowledge of Cork city accents and their locations that SC and NC speakers have. Kilkenny listeners are not able to place any of the speakers geographically, putting all speakers outside Cork city and County Cork. Nonetheless, Kilkenny listeners have similar class and occupation perceptions as the NC, SC and Macroom listeners. It seems that Kilkenny listeners are relying on phonetic cues alone to assess occupation and class, but these same phonetic cues do not trigger accurate location. 81 with occupation and class a level higher than their male counterparts. This parallels the general correspondence in our data between increased use of supra-regional, new Dublin and new Cork features on the one hand, and higher occupation and class perceptions on the other. Given that both the south and west Cork speakers are brother and sister pairings, this difference in perception of class and occupation is notable. We know that the sisters are more advanced than their brothers in shifting away from regional and even supra-regional norms to newer Dublin and Cork features, so either this fact, or simply being female, is triggering the difference in perception between the genders. Our finding that the female member of each speaker pair uses more supra-regional and new supra-regional features is consistent with work by Trudgill (1972), Eckert and McConnell-Ginet (1999), and Labov (2001). Gender Overall, females are ahead of males in using features along the supra-regional, new Dublin, new Cork cline. Likewise, females are generally perceived Figure 6 Use of phonetic features per speaker. JCSLS Vol. 21 2014 © IASLT/TCD/UCC Conclusions and implications Our data are consistent with the advance of new features of supra-regionalization in modern-day Irish English, as noted in the literature (Hickey, 2013; O’Sullivan, 2013). We have documented the use of an expanding set of supra-regional speech features in a location that is geographically and socially relatively independent of the capital of Dublin. Some aspects of this expansion are towards norms that are well established in standard international varieties of English, such as General American English, Standard Canadian English, and Southern British English. At the same time, uniquely Irish English features such as final t-frication are stable and used consistently by all our speakers. The Dublin Vowel Shift is also evident in some speakers’ vowel systems. Based on our findings, we can predict that listeners from other regions in the Republic of Ireland will evaluate speakers on the same model as the Kilkenny listeners. This remains to be seen but, if so, we would have a larger body of evidence for the decoupling of speech and location cues on the one hand, and the tight relationship between supra-regional cues and perceptions of higher class/occupation on the other. Both of these trends are consistent with the effects and uses of supra-regionalization in Irish English. Our findings contribute to an understanding of language use and perception during a period of immense change in Ireland, so they are relevant from the perspective of sociolinguistic variation and dialect studies in general. However, from a clinical perspective, it is important for speech and language JCSLS Vol. 21 2014 © IASLT/TCD/UCC 82 What’s in an Accent? therapists to be aware of speech variation in the general population as well as age- and region-related changes such as the ones reported here (Howard & Heselwood, 2013). This is of increasing importance as the pool of speech and language therapists practising in Ireland includes professionals who may not be native Irish English speakers or may not be native speakers of English at all. Watt (2013) notes the importance of speech professionals understanding the linguistic structure of accent variation, and communicating to clients and their families the linguistic equivalence of all accents, despite popular notions of the “correctness” of standard varieties. Related to this point, the socio-indexical information contained in the speech analyzed here is very much tied to concepts of personal and social identity that may need to be recognized and supported in the context of speech and language therapy. Acknowledgements Some of the work reported here is part of a final-year honours project by Eimear Mulhall, University College Cork, Ireland. References Bayard, D., Weatherall, A., Gallois, C., & Pittam, J. (2001). Pax Americana: Accent attitudinal evaluations in New Zealand, Australia and America. Journal of Sociolinguistics, 5(1), 22–49. Boersma, P. & Weenink, D. (2014). Praat: Doing phonetics by computer (Version 5.3.84) [Computer program]. Retrieved from http://www.praat.org/ Convey, D. (Ed.) (2013). Locked Out: A Century of Irish Working Class Life. Sallins: Irish Academic Press. Docherty, G. (2010). Phonological innovation in contemporary spoken British English. In A. Kirkpatrick (Ed.), The Routledge Handbook of World Englishes (pp. 59–75). London: Routledge. Eckert, P. & McConnell-Ginet, S. (1999). New generalizations and explanations in language and gender research. Language in Society, 28, 185–201. Ferragne, E. & Pelligrino, E. (2010). Formant frequencies of vowels in 13 accents of the British Isles. Journal of the International Phonetic Association, 40(1), 1–34. JCSLS Vol. 21 2014 © IASLT/TCD/UCC What’s in an Accent? 83 Fabricius, A.H., Watt, D., & Johnson, K. (2009). A comparision of three speaker-instrinsic vowel formant frequency normalization algorithms of sociophonetics. Language Variation and Change, 21, 413–435. Fridland, V. (2008). Patterns of /uw/, /ʊ/ and /ow/ fronting in Reno, Nevada. American Speech, 83(4), 432–454. Frost, P. (2000). Phonetic variation and change in the English of Cork, 2000AD: With particular reference to substratum influence (Unpublished master’s thesis). University College Cork, Cork, Ireland. Haase, T., & Pratschke, J. (2012). The 2011 HP Deprivation Index for small areas: Introduction and reference tables. Retrieved from http://trutzhaase.eu/wp/wp-content/uploads/ HP-Index-2011-SA-An-Introduction-02.pdf Hickey, R. (1998). The Dublin Vowel Shift and the historical perspective. In J. Fisiak & M. Krygier (Eds), English Historical Linguistics 1996 (pp. 79–106). Berlin: Mouton de Gruyter. Hickey, R. (2002). Historical input and the regional differentiation of English in the Republic of Ireland. In K. Lenz & M. Görlach (Eds), Of dyuersitie & chaunge of langage: Essays presented to Manfred Görlach on the occasion of his 65th birthday (pp. 199–211). Heidelberg: Winter. Hickey, R. (2003). What’s cool in Irish English? Linguistic change in contemporary Ireland. In H.L.C. Tristram (Ed.), Celtic Englishes III (pp. 357–73). Heidelberg: Winter. Hickey, R. (2004). A Sound Atlas of Irish English. Berlin: Mouton de Gruyter. Hickey, R. (2005). Dublin English: Evolution and Change. Amsterdam: John Benjamins. Hickey, R. (2010). Supraregionalisation. In L. Brinton & A. Bergs (Eds), Historical Linguistics of English. HSK series. Berlin: Mouton de Gruyter. Retrieved from https://www. uni-due.de/~lan300/16_Supraregionalisation_(Hickey).pdf Hickey, R. (2013). Variation and change in Dublin English. Retrieved from https://www. uni-due.de/VCDE/ Hickey, R. (2014). Dublin English. Retrieved from https://www.uni-due.de/IERC/ Howard, S. & Heselwood, B. (2013). The contribution of phonetics to the study of vowel development and disorders. In M. Ball & F. Gibbon (Eds), Handbook of Vowels and Vowel Disorders (pp. 61–112). New York: Psychology Press. Jansen, S. (2010). High back vowel fronting in the north-west of England. Proceedings of Sociophonetics, At the Crossroads of Speech Variation Processing and Communication. Retrieved from http://www.academia.edu/2221538/High_ back_vowel_fronting_in_the_north-west_of_England JCSLS Vol. 21 2014 © IASLT/TCD/UCC 84 What’s in an Accent? What’s in an Accent? Kallen J. (2012). The English language in Ireland: An introduction. International Journal of Language, Translation and International Communication, 1(1), 25–41. Labov, W. (2001). Principles of Linguistic Change. Volume 2: Social Factors. Oxford: Blackwell. Labov, W., Ash, S., & Boburg, C. (2006). Atlas of North American English: Phonetics, Phonology and Sound Change. New York: Mouton de Gruyter. McWilliams, D. (2005). The Pope’s Children: Ireland’s New Elite. Dublin: Gill & Macmillan. Murphy, S. (1994). A description of Cork English (Unpublished master’s thesis). University College Cork, Cork, Ireland. 85 Appendix 1 Text of recorded data Tom could feel the rainwater landing on his face as it poured down. It was five minutes to midnight. He was walking to the pier as was arranged, to meet an incoming boat. But when he arrived, facing him instead was Bruce. He opened his mouth in surprise at the sight of him. He almost forgot to breathe. He was shaking like a leaf. “It’s a trap”, he thought. He had a choice to make, to run and hide or to stand and fight. O’Baoill, D.P. (1990). Language contact in Ireland: The Irish phonological substratum in Irish-English. In J.A. Edmonson, C. Feagin & P. Mühlhäusler (Eds), Development and Diversity: Language Variation across Time and Space (pp. 147–172). Dallas: Summer Institute of Linguistics. O hUrdail, R. (1997). Confusion of dentality and alveolarity in dialects of HibernoEnglish. In J. Kallen (Ed.), Focus on Ireland (pp. 133–151). Amsterdam: John Benjamins. O’Sullivan, J. (2013). Advanced Dublin English in Irish radio advertising. World Englishes, 32(3), 358–376. Pandeli, H., Eska, J., Ball, M., & Rahilly, J. (1997) Problems of phonetic transcription: The case of the Hiberno-English slit-t. Journal of the International Phonetic Association, 27, 65–75. Pobal, (2006). Cork City: Baseline Data Report. Cork: Gamma. Thomas, E. & Kendall, T. (2007). NORM: The vowel normalization and plotting suite. [Online resource]. Retrieved from http://ncslaap.lib.ncsu.edu/tools/norm/ Trudgill, P. (1972). Sex, covert prestige and linguistic change in the urban British English of Norwich. Language and Society, 1, 179–195. Watt, D. (2013). Sociolinguistic variation in vowels. In M. Ball & F. Gibbon (Eds), Handbook of Vowels and Vowel Disorders (pp. 207–228). New York: Psychology Press. Wells, J. (1982). Accents of English. Cambridge: Cambridge University Press. JCSLS Vol. 21 2014 © IASLT/TCD/UCC JCSLS Vol. 21 2014 © IASLT/TCD/UCC Book Review Whitworth, N. & Knight, R-A. (Eds) Methods in Teaching Clinical Linguistics and Phonetics J&R Press Ltd., Guildford, UK [196 pages]. ISBN: 978-1-907826-19-1. Price £29.99/€36.49 Future d a Positive This volume, as its title suggests, focuses on teaching methods in the linguistics curriculum of speech and g in ch language therapy training programmes. The text is a Te Methods inonetics h P l written from the perspective of clinical linguistics a ic Clin tics ight Kn and Linguis e nn rather than traditional linguistics, and addresses l-A ae orth and Rach Nicole Whitw a large gap in readily available clinical linguistics teaching materials. The text contains chapters on each of the standard modules of linguistic analysis, written by mostly UK specialists and teachers in speech and language therapy programmes. After the editors’ introduction, there are chapters on articulatory phonetics, acoustic phonetics, phonology, morphology, syntax, semantics and pragmatics. Along with the clinical focus, there is a strong, welcome focus on teaching pedagogy and curriculum design. Each chapter addresses the alignment of teaching and assessment methods with learning outcomes (Biggs, 2003) and provides practical examples of this alignment. There is an accompanying Facebook page that provides additional samples of teaching and assessment material, though at the time of review material was not available for all chapters. Book chapters are structured around consideration of learning outcomes, core curriculum components, teaching and assessment methods (including materials and resources), and pitfalls. For instance, Chapter 2, Articulatory Phonetics, identifies learning outcomes as contemporaneous transcription of client speech, perception (identification, labelling, use of IPA symbols) and production knowledge of all speech sounds. The delivery of this core curriculum assumes two hours of phonetics per week over four terms in both undergraduate and graduate programmes. This is an optimistic assumption, in my experience, and hours dedicated to phonetics will vary depending on e Janet O’Keef (Editor) JCSLS Vol. 21 2014 © IASLT/TCD/UCC 88 Book Review Book Review design and delivery methods. The core curriculum components suggested for articulatory phonetics are no different than those that would be taught in an introductory linguistics course; however, the authors stress the inclusion of clinical data, integration with practice education, and classroom analysis of speech samples that emphasize the link with diagnosis and treatment choices. Teaching techniques in support of this, the authors note, might include small tutorial groups for production and perception practice, lectures, frequent informal testing, labs, use of interactive IPA charts, podcasts of lectures, transcription materials on virtual learning environments and so on. A useful and much needed emphasis throughout the text is on encouraging enjoyment of clinical linguistics, and demystifying the analytic component. Student learning and satisfaction is strongly supported by classroom activities and resources that reinforce the clinical relevance of their developing skills. Barbara Dodd’s chapter on phonology foregrounds the need for clinical therapists to have a firm grasp of the categorical difference between disorders of organic as opposed to functional origin, and disorders that affect articulation rather than phonology. The latter is related to the distinction in generative linguistics between errors of ‘performance’ versus errors of ‘competence’. Students of linguistics often require time to absorb this distinction and understand its consequences (as well as its limitations), despite exposure to the concept in all domains of formal linguistics. Students of clinical linguistics are no different, and require a lot of support and guided analysis of relevant data. Dodd proposes co-teaching (SLT and clinical linguist) of some assessment and intervention components as a way of compensating for the limitations of a single perspective. Subsequent chapters provide similar coverage of teaching practice in other areas of linguistics, from acoustic phonetics through to pragmatics. In all cases the authors present useful guidelines and practical suggestions that will be of interest to lecturers and practice educators. One outcome of this collection is a tentative identification of effective teaching practice(s) in clinical linguistics. We all know that effective teaching involves many factors. It is valuable, therefore, to have some of these factors outlined and discussed so thoroughly, as in this volume. As a linguist teaching in a clinical programme, I found this a valuable and very useful book. In various places the chapter authors note the diversity of training backgrounds of lecturers within Speech and Language Therapy/ JCSLS Vol. 21 2014 © IASLT/TCD/UCC 89 Human Communication departments and indeed, the wealth of perspectives and expertise that this diversity brings. I was relieved to see that as a linguist, I was doing many of the things that the chapter authors recommend for their clinical audience. Of particular value for lecturers is the discussion of lecture coverage, activities, and the practical resources mentioned in the text and provided on the Facebook page. In general, there is a huge need for access to structured clinical data that can be used for classroom teaching and for independent learning. This need is only beginning to be met. National or association-sponsored databases would contribute hugely to the quality of teaching and self-directed learning opportunities for practitioners and students of speech and language therapy. Dr Nicola Bessell, Adjunct Lecturer, Department of Speech and Hearing Sciences, University College Cork, Ireland. E-mail: n.bessell@ucc.ie References Biggs, J. (2003). Teaching for Quality Learning at University (2nd ed.). Maidenhead: Society for Research into Higher Education/Open University Press. JCSLS Vol. 21 2014 © IASLT/TCD/UCC 91 90 IALP /ŶƚĞƌŶĂƟŽŶĂůƐƐŽĐŝĂƟŽŶŽĨ >ŽŐŽƉĞĚŝĐƐĂŶĚWŚŽŶŝĂƚƌŝĐƐ 30th World Congress of the I.A.L.P CityWest Hotel Conference & Event Centre Dublin, Ireland 21 – 25 August 2016 J&R Press For more information about our Human Communication Science books please visit our website: www.jr-press.co.uk Learn about cutting edge research Present your Discover new developments and products in the industry Network with leading international academics and clinicians The worldwide own research organization of Registration professionals and Call and scientists in for Abstracts Opens communication, voice, August 2015 speech language Exhibition and Sponsorship pathology, audiology Opportunities and swallowing The Congress Main Report Themes Neuro-scientific implications in assessment and intervention in acquired communication disorders Technological advances and innovation in voice and dysphagia Biological and environmental influences in prevention and early intervention in speech and language disorders Creating the Future Now: Advancing Research and Clinical Practice www.ialpdublin2016.org JCSLS Vol. 21 2014 © IASLT/TCD/UCC JCSLS Vol. 21 2014 © IASLT/TCD/UCC