Treatment of Giardiasis and Drug Resistance Abstract
advertisement

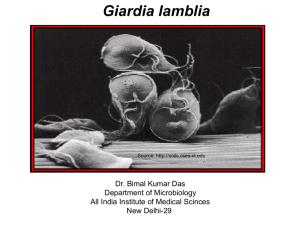
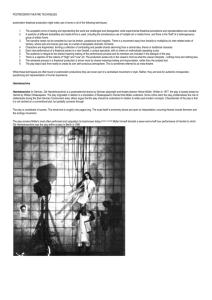
Treatment of Giardiasis and Drug Resistance Joachim Müller, Andrew Hemphill and Norbert Müller Abstract Giardia lamblia (also known as G. duodenalis or G. intestinalis), a flagellated protozoan, is the most common causative agent of persistent diarrhea worldwide. The life cycle includes motile, flagellated trophozoites parasitizing the upper intestine and thick-walled cysts forming in the lower intestine, which are subsequently shed with the feces. Chemotherapy is directed against the trophozoite stage. The current antigiardial therapy of choice is metronidazole. In the case of resistance, alternatives are other nitroimidazoles, quinacrine, albendazole, and nitazoxanide. Here, we present a review of current antigiardial drugs and of their modes of action. USA for the treatment of persistent diarrhea due to cryptosporidiosis and giardiasis in people older than 12 years (reviewed by Hemphill et al., 2006). Moreover, in vitro effects of natural compounds such as isoflavones, polyenes or saturated fatty acids against trophozoites have been described, but clinical data are lacking. An overview of antigiardial compounds with references is given in Table 1. In this chapter, we will focus on the mode of action of these drug families (so far as known) and put some new light on resistance mechanisms. Mode of Action and Drug Targets General Remarks Introduction For the treatment of giardiasis, chemotherapy is the method of choice. After the introduction of quinacrine as the first antigiardial drug in the 1940s, metronidazole (commercially known as Flagyl®) and other nitroimidazoles such as tinidazole have been used as a therapy of choice for more than five decades. In the case of resistance formation, substitution therapies include benzimidazole albendazole, the acridine derivative quinacrine – historically the first antigiardial drug –, or the aminoglycoside paromomycin alone or in combination with metronidazole (see for review Upcroft and Upcroft, 2001 and for a recent clinical study Mørch et al., 2008). In the mid-1990s, a new antiparasitic agent, the thiazolide nitazoxanide (commercially known as Alinia®), has been introduced in the market. Nitazoxanide has been approved in the Norbert Müller () Institute of Parasitology, University of Bern, Länggass-Strasse 122, 3012 Bern, Switzerland The ideal situation for the mode of action of antiparasite drugs consists of binding to a target protein (enzyme or receptor) resulting in the inhibition of essential cellular functions. Such targets are identified by analyzing structural and metabolic alterations of the parasite due to the drug followed by the isolation of drug binding proteins or the analysis of resistant vs. sensitive parasites. The isolated targets are then validated by inhibition studies in vitro, structural analysis of protein-ligand complexes, and – if possible – knock-out and overexpression studies of the corresponding gene in the target organism (see e.g. Wang, 1997). In an ideal situation, the drug-target interaction depends on distinct structural features of the target. In this case, point mutations causing the presence or absence of a single amino acid or nucleotide (in the case of rRNA as a target) discriminate between resistance or susceptibility. In reality, the situation is more complex. In resistant organisms, the “ideal” target may still be present, but the drug cannot access it due J. Müller et al. Table 1 Overview of antigiardial drugs. With regard to the efficacy, the order of magnitude of the IC50 from in vitro studies and – if available – the dose for patients are given Class Acridines Aminoglycosides Benzimidazoles Compound Quinacrine Paromomycin Albendazole Bis-benzimidazoles Efficacy Reference –7 In vitro (10 M) Bell et al., 1991; Bénéré et al., 2007 In vivo (100 mg tid + MET 750 mg tid for 2–3 weeks) Nash et al., 2001; Mørch et al., 2008 –4 –5 In vitro (10 –10 M) Edlind, 1989 In vivo: 500 mg tid for 1 week Mørch et al., 2008 –8 In vitro (10 M) Katiyar et al., 1994, Upcroft and Upcroft, 2001; Cruz et al., 2003 In vivo (400 mg bid + MET 250 mg bid or tid for 1 week) Mørch et al., 2008 –8 –6 In vitro (10 –10 M) –5 Fatty acids Dodecanoic acid In vitro (10 M) Fluoroquinolones Ciprofloxacine In vitro (10 M) Rayan et al., 2005 –4 Sousa and Poiares-da-Silva, 2001 –6 Isoflavones Genistein Formononetin In vitro (10–8 M) In vitro (10 M) Nitrofuranes Furazolidone In vitro (10 –10 M) –5 Bell et al., 1993 Khan et al., 2000; Sterck et al., 2008 –6 –6 Cedillo-Rivera and Munoz, 1992 Nitroimidazoles Metronidazole Tinidazole In vitro (10 M); in vivo Diaminidines Pentamidine and derivatives In vitro (10 –10 M) Bell et al., 1991 Anthony et al., 2005 –8 –6 Polyenes Allicin and derivatives In vitro Thiazolides Nitazoxanide In vitro (10 M) In vivo to uptake limitation or detoxification mechanisms. A search for drug targets (e.g. by protein binding studies) would thus yield detoxification enzymes, transporters or even irrelevant drug binding proteins besides the “true” target. Conversely, susceptibility to a drug may be triggered by the ability to convert a (ineffective) prodrug to the (effective) drug. In this case, search for targets have to be performed with the effective molecule, otherways, the transforming enzyme would be identified rather than the target itself. In the case of antiparasite drugs (as well as other antibiotics), the situation is rendered more complicated by the fact that the drug acts in the vicinity or even inside the host cell (in the case of intracellular pathogens). Therefore, the mode of action of the drug may be modulated if not depend on the susceptibility of the host cell and not the parasite itself. In the following paragraphs, we will discuss some examples within the framework of antigiardial drugs. –6 Gardner and Hill, 2001 Fox and Saravolatz, 2005; Hemphill et al., 2006 Methods for the Determination of Drug Efficacy In order to determine the efficacy of antigiardial drugs (e.g. in terms of IC50 values), a couple of methods are currently in use. The most classical way is counting trophozoites grown axenically in the presence of drugs (see e.g. Müller et al., 2006). The incorporation of 3H-thymidine is less subjective (see e. g. Adagu et al., 2002). Both methods are time-consuming or need high-level equipment. An elegant alternative is the use of the vital staining resazurin (Alamar Blue; Bénéré et al., 2007). Viable cells reduce resazurin forming a pink compound absorbing at 550 nm and fluorescing at >590 nm. Although it is possible to use spectrophotometry for quantifying the product, the best sensitivity is obtained with fluorimetry. Fluorimeters are, however, expensive and therefore not present in many labs. Moreover, all these methods cannot be Treatment of Giardiasis and Drug Resistance used when trophozoites are not grown axenically, but in a coculture system with intestinal cells (e.g. Caco 2). In this system, trophozoites may be quantified using real-time PCR with a Giardia-specific target (Müller et al., 2006). A suitable alternative would be the use of a reporter strain as shown for instance for Toxoplasma gondii expressing β-galactosidase (McFadden et al., 1997; see for a recent application Müller et al., 2009a). In the case of Giardia, a reporter strain expressing glucuronidase A from E. coli has been created (Müller et al., 2009b). This strain is well suited for the determination of IC50 values and for high-throughput drug screening using simple colorimetric assays. Moreover, it can be used in a coculture system with host cells thus allowing the determination of the “therapeutical window”, i.e. the gap between drug efficacy and host cell toxicity in one screen. Nucleic Acids as Targets Early studies have shown that the acridine derivative quinacrine, the first antigiardial drug, interacts with DNA inhibiting replication and RNA and protein biosynthesis in prokaryonts (Ciak and Hahn, 1967). Like other acridine derivatives, quinacrine is an intercalating agent binding to DNA with a preference for (A+T)-rich regions and thereby blocking DNA replication and RNA biosynthesis (Wilson et al., 1994). In studies concerning pentamidine derivatives (Bell et al., 1991) and bis-benzimidazoles (Bell et al., 1993), very nice correlations between the binding affinities of these compounds to calf thymus DNA and their efficacies against Giardia lamblia have been pointed out. Since DNA binding is by far not species specific and therefore prone to side effects on host cells, the relevance of a DNA binding agent as an antimicrobial drug resides in other – more species specific – properties like a differential uptake or metabolism or the presence of other targets besides DNA. For instance, pentamidines and a variety of other DNA binding compounds such as etoposide induce the cleavage of Trypanosoma DNA minicircles in a pattern that resembles the action of topoisomerase II inhibitors (Shapiro and Englund, 1990). DNA modifying enzymes may thus constitute more selective targets for antimicrobial agents. Fluoroquinolones such as ciprofloxacine inhibit DNA-gyrases and topoisomerases from prokaryonts (Kidwai et al., 1998) and are highly effective against G. lamblia as shown in a descriptive study (Sousa and Poiares-da-Silva, 2001). It is, however, unclear, which type of enzyme is inhibited there since more pronounced studies are lacking. A phylogeny analysis of type II topoisomerases shows that the gene of G. lamblia (GlTop2) is eukaryont-like and not closely related to prokaryont topoisomerases (He et al., 2005). Aminoglycosides bind to the small subunit of ribosomes, more exactly to distinct features of the 16SrRNA secondary structure and thereby inhibit protein biosynthesis (see e.g. Brodersen et al., 2000 for a detailed structural analysis). Therefore, specific mutations in this region confer resistance to various aminoglycosides in various prokaryonts. G. lamblia has a 16S-rRNA structure similar to prokaryonts with a primary sequence suggesting that only paromomycin and hygromycin are effective, other well known aminoglycosides such as kanamycin are not. This pattern correlates well with observed susceptibility or resistance to a panel of aminoglycosides (Edlind, 1989). Cytoskeleton Proteins as Targets Early studies with benzimidazoles such as albendazole showed effects on the cytoskeleton, especially in the region of the ventral disk (Fig. 1; see e.g. Chavez et al., 1992; Hemphill et al., 1996). Molecular genetics has revealed that sensitivity to albendazole (or other benzimidazoles) in evolutionary distant organisms such as fungi, nematodes, platyhelminthes, and various protozoa including G. lamblia is correlated to the presence of specific alleles of β-tubulin-genes (Kirk-Mason et al., 1988; Driscoll et al., 1989; Katiyar et al., 1994; Kwa et al., 1995; Henriquez et al., 2008), the substitution of Phe to Tyr in position 200 being sufficient for switching from benomyl sensitivity to resistance as shown in nematodes (Kwa et al., 1995). Molecular modeling of the putative albendazole binding site in albendazole resistant Acanthamoeba β-tubulin indicates that 4 of 13 residues are different from tubulins of sensitive organisms. Resistance is conferred when, besides Phe200, Phe167 is replaced (Henriquez et al., 2008). J. Müller et al. A: Albendazole B: Control Fig. 1 Examples of ultrastructural changes induced by albendazole and visualized by transmission electron microscopy, A, albendazole; B, control; N, nucleus Drugs Interfering with Intermediary Metabolism The nitroimidazole metronidazole is clearly the best studied compound affecting intermediary metabolism. When trophozoites are treated with metronidazole the cell looses motility within a few hours followed by appearance of large zones of lesions on the dorsal shield and swelling of the cell body (Fig. 2; see e.g. Müller et al., 2006). According to a widely referred theory, metronidazole (as a prodrug) is reduced to a nitro radical by electrons coming from the enzyme pyruvate:flavodoxin/ferredoxin oxidoreductase (PFOR), a protein lacking in higher eukaryotic cells (Horner et al., 1999). The radical causes irreversible damages. Results obtained with the microaerophilic parasite Trichomonas vaginalis suggest, however, another mode of action. By comparing 2-Dprotein electrophoresis patterns from treated and untreated cells, the authors suggest that metronidazole binds to the sulfhydryl group in the active center of various enzymes including thioredoxin reductase thereby impairing essential cellular functions (Leitsch et al., 2009). Also in this model, an activated form of metronidazole would act on multiple targets, the number being limited to enzymes with sulfhydryl groups in their active center. A mode of action similar to nitroimidazoles has been postulated for nitrothiazolides. Upon oral uptake, nitazoxanide, the best studied nitrothiazolide, is rapidly deacetylated to tizoxanide and further metabolized to tizoxanide-glucuronide (Fox and Saravolatz, 2005). Tizoxanide has been reported to display antimicrobial activity similar to nitazoxanide, while tizoxanide-glucuronide is largely inactive against a number of pathogens including Giardia. Thiazolides without the thiazole-associated nitro group have been shown to exhibit decreased or no efficacy against Giardia (Adagu, et al., 2001; Müller et al., 2006). Therefore, an involvement of the nitro group in the mechanism of action, with the participation of PFOR similar to metronidazole, is likely (Wright et al., 2003). The nitro group is also required for in vitro activity against anaerobic bacteria (Pankuch and Apelbaum, 2006). Moreover, nitazoxanide inhibits activities of recombinant PFOR from various bacteria and parasites including G. lamblia (Sisson et al., 2002). A reduction of nitazoxanide, however, has never been observed in vivo. Instead, there is some evidence that unreduced nitazoxanide blocks an intermediate step of the reaction thus inhibiting PFOR in a non-competitive manner (Hoffman et al., 2007). When G. lamblia trophozoites are treated with nitrothiazolides, ultrastructural analyses Treatment of Giardiasis and Drug Resistance A: Control B: NTZ C: MTZ D: MTZ Fig. 2 Examples of ultrastructural changes induced by nitazoxanide and metronidazole and visualized by scanning electron microscopy, A, control; B, nitazoxanide (NTZ); C, D, metronidazole (MTZ) reveal severe damages of the ventral disk instead of damages of the dorsal surface membrane as observed with metronidazole (Fig. 2; see e.g. Müller et al., 2006). In G. lamblia, a nitroreductase as a nitazoxanide-binding protein was identified and characterized. Nitroreductase is inhibited by nitazoxanide, and, as for PFOR, there is no evidence for a reduction by nitroreductase (Müller et al., 2007b). Overexpression of this nitroreductase is, however, correlated with increased sensitivity to metronidazole and nitazoxanide (Nillius et al., 2011). Besides nitroreductase, protein disulfide isomerases from G. lamblia (Müller et al., 2007a) and Neospora caninum (Müller et al., 2008b) are potential targets for nitazoxanide. Recent studies have shown that not only nitazoxanide, but also derivatives lacking the nitro group (reviewed in Hemphill et al., 2007) exhibit in vitro activity against the intracellular apicomplexan parasites N. caninum, Cryptosporidium parvum and Besnoitia besnoiti (Hemphill et al., 2006; Cortes et al., 2007) and as well as proliferating host cells (Müller et al., 2008c). Therefore, it cannot be excluded that the efficacy of nitazoxanide against giardiasis and cryptosporidiosis in patients is partly due to effects on intestinal cells. In vivo studies on these diseases with non-nitro-thiazolides are lacking. In proliferating host cells (Caco2), inhibition of glutathione-S-Transferase P1 (GSTP1) by nitazoxanide J. Müller et al. and some non-nitro-thiazolides is well correlated with their efficacy to induce apoptosis. Overexpression and downregulation of GSTP1 is correlated with an increase, or decrease, of sensitivity, respectively (Müller et al., 2008c). Compounds of Plant Origin with Miscellaneous Targets In order to improve the situation in chemotherapy of metronidazole resistant giardiasis, new potential pharmaceuticals from natural sources have been evaluated regarding their antigiardial activity in vitro. In general, crude extracts from traditional medicinal herbs are tested with respect to antigiardial activities and then fractionated in order to identify the active principles (see for review Anthony et al., 2005). Essential oils are a well explored source for antimicrobial compounds. A good example for a study on antigiardial properties in oregano extracts is given by Ponce-Macotela et al. (2006). Often, essential oils have a broad spectrum of efficacy and therefore a potential toxicity to host cells. A good example is a study where active compounds have been identified from Allium extracts (Harris et al., 2000). In this study, the compound with the lowest IC50 is allyl alcohol, a compound with an unspecific toxicity and a potential cancerogene. Allicin, another molecule effective against Giardia and other parasites such as Entamoeba, bind to SH-groups from cysteine proteases and other SH-proteins including thioredoxin reductase (see Ankri et al., 1997; Ankri and Mirelman, 1999), a mode of action recently postulated for metronidazole (Leitsch et al., 2009). Another well studied group are isoflavones. Isoflavones are mainly found in Leguminosae where they have anti-oxidant, anti-microbial and signalling functions (e. g. reviewed in Dakora and Phillips, 1996; Dixon and Steele, 1999). Within this group of compounds, Khan et al. (2000) identified formononetin, a major isoflavone of Ononis sp, as the most potent antigiardial agent. In vitro, formononetin has an IC50 value in the range of 10–7 M, thus one order of magnitude lower than the non-methylated daidzein and genistein, two isoflavones of soybean (Sterk et al. 2008). By daidzein-affinity chromatography, a nucleoside hydrolase was identified as daidzein-binding protein. Nucleoside hydrolase activity is inhibited by the three isoflavones mentioned above in a range of concentrations where daidzein and genistein inhibit trophozoite growth in vivo. In Crithidia (Parkin et al., 1991), Leishmania (Shi et al., 1999) or Trypanosoma (Parkin, 1996), the function of nucleoside hydrolase is central in salvaging purine nucleosides from the host and essential since the parasites lack purine de novo synthesis. Inhibition would thus lead ultimately to a block of DNA synthesis and thus cell division. This effect would be rather slow. Formononetin acts faster by stopping motility and inducing detachment within less than 2 h (Lauwaet et al., 2010, and own, unpublished data) and is inhibitory at ten times lower concentrations suggesting other mechanisms to be involved in addition such as depolarization of the membrane due to uncoupling effects or direct inhibition of membrane ATPases. However, experimental evidence for any of these possibilities is lacking. Resistance Formation Besides the search for drug binding proteins, another way to elucidate the action of drugs is the comparison of resistant vs. non-resistant trophozoites. Resistant trophozoites are created by selecting growing cells in the presence of increasing drug concentrations followed by cloning and characterization of the resistant clones vs. wildtype clones. Moreover, in some cases, drug (mainly metronidazole) resistant strains have been isolated from patients and compared to non-resistant strains. Table 2 gives an overview of selected studies. Resistance to metronidazole and other nitroimidazoles has been induced in vitro; and various genotypically distinct isolates with reduced drug susceptibility have also been found in human patients (Gardner and Hill, 2001; Upcroft and Upcroft, 1993). Formation of resistance to metronidazole is associated with an altered uptake of the drug (Boreham et al., 1988; see also Upcroft et al., 1996 for quinacrine), downregulation of the PFOR activity (Upcroft and Upcroft 2001). This is consistent with the model claiming an involvement of PFOR in metronidazole activation (Townson et al., 1996; Sisson et al., 2002). Recent findings in T. vaginalis suggest, however, that metronidazole and other nitroimidazoles covalently bind and thereby Treatment of Giardiasis and Drug Resistance Table 2 Overview of studies on resistance formation in G. lamblia Drug Source of resistance Method Important findings Reference Albendazole Induction of resistance in vitro in WB Comparison to wildtype with respect to growth Resistance at 4.5 µM for several weeks, normal cyst formation Lindquist, 1996 Induction of resistance in vitro in WB 1B Molecular genetics, ultrastructural analysis Induced resistance not related to β-tubulin modifications Upcroft et al., 1996 Patient isolates Comparison of isolates with respect to growth Isolates exhibit variations in their sensitivities prior to drug exposition Argüello-García et al., 2004 Induction of resistance in vitro in WB 1 Representational difference analysis of gene expression Induced resistance not related to β-tubulin modifications; antigenic variation Argüello-García et al., 2009 Quinacrine Induction of resistance in vitro in 7 different lines Comparison to sensitive lines with respect to growth, investigation of quinacrine uptake by fluorescence Quinacrine excluded from resistant lines, multidrug resistance in some lines Upcroft et al., 1996 Metronidazole Patient isolates with different susceptibilities Analysis of uptake growth Resistant isolates have a lower uptake Boreham et al., 1988 Patient isolates, induction of resistance formation in vitro PFOR assay PFOR activity is lower in resistant isolates Upcroft and Upcroft 1993, 2001 and references therein Patient isolates Comparison of isolates with respect to growth Isolates exhibit variations in their sensitivities prior to drug exposition Argüello-García et al., 2004 Induction of resistance in vitro in WB 1 Representational difference analysis of gene expression PFOR expression higher in resistant clones; antigenic variation Argüello-García et al., 2009 Induction in vitro T. vaginalis Comparison to wildtype by proteomics Metronidazole binds to proteins of thioredoxin pathway Leitsch et al., 2009 Nitazoxanide Induction of resistance formation in vitro in WB C6 Comparison to wildtype with respect to expression of selected genes and by microarray Cross-resistance to metronidazole. Complex changes of gene expression including antigenic variation and overexpression of chaperones in resistant clone Müller et al., 2007a, 2008a Isoflavones Induction of resistance formation in vitro in WB C6 Comparison to wildtype with respect to expression of selected genes and by microarray Most pronounced changes of gene expression concern antigenic variation Sterk et al., 2007 Unpublished data J. Müller et al. inactivate proteins related to the thioredoxin reductase pathway. Resistant cells overcome this blocking by reregulating other enzymes involved in oxidoreductive processes, such as PFORs. In this model, downregulation of PFOR would be a consequence rather than a prerequisite of resistance formation (Leitsch et al., 2009). In another study, even a positive correlation between metronidazole-resistance formation and PFOR gene transcription activity has been observed (Argüello-Garcia et al., 2009). Furthermore, possible giardial metronidazole-resistance mechanisms involving reduced uptake of the drug (Boreham et al., 1988) or complex changes in the gene expression pattern including alterations of those genes (encoding variant surface proteins, VSPs) that mediate antigenic variation of the parasite (Müller et al., 2007; 2008; see also below) have been described. In order to elucidate the biochemical nature of resistance formation against nitazoxanide metronidazole, and formononetin, G. lamblia WB C6 clones resistant to these drugs were generated (Müller et al., 2007a, 2008a; Sterck et al., 2007) and compared to the wildtype WB C6 with respect to their growth behavior and to the expression pattern of genes that are potentially involved in resistance formation. In all cases, resistance formation occurred after a small number of selection cycles. The pattern of up- and downregulated mRNAs was completely different in a nitazoxanide/metronidazole double resistant line, a line resistant for metronidazole only and a formononetin resistant line. The only annotated ORFs downregulated in all screens encoded the major surface-labeled trophozoite antigen 417 encoding the major surface antigen C6 (TSA417; Müller et al. 2007a, 2008a; Sterk et al., 2007 and unpublished data). In the nitazoxanide/metronidazole double resistant line, genes potentially involved in protein phosphorylation and network formations, especially ankyrins, and chaperonins (especially the cytosolic heat shock protein 70) are upregulated. The roles of these chaperonins in Giardia are not well understood. In human cells, molecular chaperones such as HSP72 and HSP27 prevent cells from apoptosis induced by heat shock (Gabai and Sherman, 2002). If similar mechanisms occur in Giardia, a general response to stress via induction of chaperonins could be responsible for thermotolerance as well as for drug resistance. Interestingly, a similar change in gene expression patterns has been found upon expression of neomycin phosphotransferase as a resistance marker and a subsequent selection for puromycin resistant trophozoites (Su et al., 2007). As mentioned above, nitazoxanide inhibits protein disulfide isomerases (PDIs) from G. lamblia (Müller et al., 2007a) and N. caninum (Müller et al., 2008b). Inhibition of PDIs in vivo could lead to the formation of badly folded proteins and thus to an impairment of central metabolic and regulatory processes. Cells that overexpress chaperonins and proteins involved in the stabilisation of subcellular structures such as ankyrins could overcome the deleterious effects due to PDI inhibition. Such indirect, stabilizing effects due to chaperonins or related proteins could also explain why artificially generated albendazole resistance (Upcroft et al., 1996; Argüello-Garcia et al., 2009) is not correlated to specific mutations of the β-tubulin gene as found in other albendazole resistant organisms. In this context, it is noteworthy that antigenic variation was also found to be a striking phenomenon associated with in vitro resistance formation against albendazole (Argüello-Garcia et al., 2009). Giardia populations seem to have very flexible mechanisms in order to respond to changes in the environment such as drug pressure, presence of antibodies or even changes in medium composition and to changes of the internal milieu by introduction of transgenes (Su et al., 2007) in a way that complex gene expression patterns seem to be fine-tuned in order to find an optimal compromise between speed of growth and survival. How can these changes be explained? Individual trophozoites in cultures of G. lamblia (clone WB C6) exhibit substantial variations in their degree of susceptibility/resistance to different drugs even in absence of any previous drug pressure (Argüello-Garcia et al., 2004). This suggests that resistance formation within a G. lamblia in vitro culture seems to have its origin in a drug-independent process of continuous growth competition between relatively drug-susceptible and drug-resistant trophozoite subpopulations. The differences in these subpopulations may be explained by genetic effects, i.e. random point mutations all over the genome and selection of resistant phenotypes upon drug application or by epigenetic effects (transcriptional or posttranscriptional) resulting in subpopulations with different Treatment of Giardiasis and Drug Resistance gene expression patterns. In the latter case, exposure of the trophozoites to a drug in sublethal concentrations might even enhance conversion from a sensitive to a resistant phenotype. The only common finding in all resistant lines is the change in variable surface protein gene expression (where investigated) resulting in antigenic variation (Müller and Gottstein, 1998; Svärd et al., 1998; Prucca and Lujan, 2009). Antigenic variation in G. lamblia allows the parasite to escape the host immune response (Müller and Gottstein, 1998; Müller, and von Allmen, 2005; Roxström-Lindquist et al., 2006). Epigenetic mechanisms at the transcriptional level involving histone acetylation (Kulakova et al., 2006) and at the post-transcriptional level involving RNA interference (Prucca et al., 2008) are considered as controlling antigenic variation (Prucca and Lujan, 2009). Thus, common epigenetic mechanisms may control both antigenic variation and drug resistance in Giardia. The role of epigenetics in antigenic variation and drug resistance in Giardia and other parasites is – of course – far from being understood, but may be of a broader interest since evolution of antibiotic resistance initiated by increasing sublethal doses of various antibiotics has been attributed to epigenetic inheritance also in bacteria (Adam et al., 2008). The overview in Table 2 shows that most studies have been performed with the strain WB C6 showing a high degree of antigenic variation (Nash et al., 1990b). Drug resistance studies from other strains with little variation such as GS-M-83-H7 or WB A6 (Nash et al., 1990a) are lacking but would be most useful in putting the light on the relationship between antigenic variation and drug resistance formation. Conclusions After more than 7 decades of antigiardial chemotherapy, metronidazole is still the treatment of choice. Novel drugs such as nitazoxanide or plant-derived compounds do not offer obvious advantages with respect to efficacy or resistance formation. A couple of studies concerning resistance formation suggest a more complex mechanism than the mere mutation of a target protein. Where investigated, resistance formation is correlated with antigenic variation suggesting a common, underlying mechanism far from being understood. Future approaches aimed at transgenic upor down-regulation of putative drug target proteins in G. lamblia are expected to provide conclusive insights into both the mode of action of anti-giardial drugs and the mechanisms that mediate resistance against these drugs. References Adagu IS, Nolder D, Warhurst D, and Rossignol JF (2002) In vitro activity of nitazoxanide and related compounds against isolates of Giardia intestinalis, Entamoeba histolytica and Trichomonas vaginalis. J Antimicrob Chemother 49: 103– 111 Adam M, Murali B, Glenn N, and Potter SS (2008) Epigenetic inheritance based evolution of antibiotic resistance in bacteria. BMC Evol Biol 8: 52 Argüello-García R, Cruz-Soto M, Romero-Montoya L, and Ortega-Pierres G (2004) Variability and variation in drug susceptibility among Giardia duodenalis isolates and clones exposed to 5-nitroimidazoles and benzimidazoles in vitro. J Antimicrob Chemother 54: 711–721 Argüello-García R, Cruz-Soto M, Romero-Montoya L, and Ortega-Pierres G (2009). In vitro resistance to 5-nitroimidazoles and benzimidazoles in Giardia duodenalis: variability and variation in gene expression. Infect Genet Evol 9: 1057–1064 Ankri S and Mirelman D (1999) Antimicrobial properties of allicin from garlic. Microbes Infect 1: 125–129 Ankri S, Miron T, Rabinkov A, Wilchek M, and Mirelman D (1997) Allicin from garlic strongly inhibits cysteine proteinases and cytopathic effects of Entamoeba histolytica. Antimicrob Agents Chemother 41: 2286–2288 Anthony J-P, Fyfe L, and Smith H (2005) Plant active components – a resource for antiparasitic agents? Trends Parasitol 21: 462–468 Bell CA, Dykstra CC, Naiman NA, Cory M, Fairley TA, and Tidwell RR (1993) Structure-activity studies of dicationically substituted bis-benzimidazoles against Giardia lamblia: correlation of antigiardial activity with DNA binding affinity and giardial topoisomerase II inhibition. Antimicrob Agents Chemother 37: 2668–2673 Bell CA, Hall JE, Cory M, Fairley T, and Tidwell RR (1991) Structure-activity relationships of pentamidine analogs against Giardia lamblia and correlation of antigiardial activity with DNA binding affinity. Antimicrob Agents Chemother 35: 1099–1107 Bénéré E, Inocencio da Luz RA, Vermeesch M, Cos P, and Maes L (2007) A new quantitative in vitro microculture method for Giardia duodenalis trophozoites. J Microbiol Methods 71: 101–106 Boreham PF, Phillips RE, and Shepherd RW (1988) Altered uptake of metronidazole in vitro by stocks of Giardia intestinalis with different drug sensitivities. Trans R Soc Trop Med Hyg 82: 104–106 J. Müller et al. Brodersen DE, Clemons WM Jr, Carter AP, Morgan-Warren RJ, Wimberly BT, and Ramakrishnan V (2000) The structural basis for the action of the antibiotics tetracycline, pactamycin, and hygromycin B on the 30S ribosomal subunit. Cell 103: 1143–1154 Cedillo-Rivera R, and Muñoz O (1992) In-vitro susceptibility of Giardia lamblia to albendazole, mebendazole and other chemotherapeutic agents. J Med Microbiol 37: 221–224 Chavez B, Cedillo-Rivera R, and Martinez-Palomo A (1992) Giardia lamblia: ultrastructural study of the in vitro effect of benzimidazoles. J Protozool 39: 510–515 Ciak J and Hahn FE (1967) Quinacrine (atebrin): mode of action. Science 156: 655–656 Cortes HCE, Müller N, Esposito M, Leitão A, Naguleswaran A, and Hemphill A (2007) In vitro efficacy of nitro- and bromo-thiazolyl-salicylamide compounds (thiazolides) against Besnoitia besnoiti infection in Vero cells. Parasitology 134: 975–985 Dakora FD and Phillips DA (1996) Diverse functions of isoflavonoids in legumes transcend anti-microbial definitions of phytoalexins. Physiol Mol Plant Pathol 49: 1–20 Dixon RA and Steele CL (1999) Flavonoids and isoflavonoids – a good mine for metabolic engineering. Trends Plant Sci 4, 394–400. Driscoll M, Dean E, Reilly E, Bergholz E, and Chalfie, M. (1989) Genetic and molecular analysis of a Caenorhabditis elegans β-tubulin that conveys benzimidazole sensitivity. J Cell Biol 109: 2993–3003 Edlind TD (1989) Susceptibility of Giardia lamblia to aminoglycoside protein synthesis inhibitors: correlation with rRNA structure. Antimicrob Agents Chemother 33: 484– 488 Edlind TD, Hang TL, and Chakraborty PR (1990) Activity of the anthelmintic benzimidazoles against Giardia lamblia in vitro. J Infect Dis 162: 1408–1411 Escobedo AA and Cimerman S (2007) Giardiasis: a pharmacotherapy review. Expert Opin Pharmacother 8: 1885–1902 Fox LM and Saravolatz LD (2005) Nitazoxanide: a new thiazolide antiparasitic agent. Reviews of Anti-infective Agents 40: 1173–1180 Gabai VL and Sherman MY (2002) Interplay between molecular chaperones and signaling pathways in survival of heat shock. J Appl Physiol 92: 1743–1748 Gardner TB and Hill DR (2001) Treatment of Giardiasis. Clin Microbiol Rev 14: 114–128 Harris JC, Plummer S, and Lloyd D (2001) Antigiardial drugs. Appl Microbiol Biotechnol 57: 614–619 Harris JC, Plummer S, Turner MP, and Lloyd D (2000) The microaerophilic flagellate Giardia intestinalis: Allium sativum (garlic) is an effective antigiardial. Microbiology 146: 3119–3127 Hausen MA, Freitas JC Jr, and Monteiro-Leal LH (2006) The effects of metronidazole and furazolidone during Giardia differentiation into cysts. 1: Exp Parasitol 113: 135–141 He D, Wen JF, Chen WQ, Lu SQ, and Xin DD (2005) Identification, characteristic and phylogenetic analysis of type II DNA topoisomerase gene in Giardia lamblia. Cell Res 15: 474–482 Hemphill A, Müller J, and Esposito M (2006) Nitazoxanide, a broad-spectrum thiazolide anti-infective agent for the treat- ment of gastrointestinal infections. Expert Opin Pharmacother 7: 953–964 Hemphill A, Müller N, and Müller J (2007) Structure-function relationship of thiazolides, a novel class of anti-parasitic drugs, investigated in intracellular and extracellular protozoan parasites and larval-stage cestodes. Antiinf Agents Med Chem 6: 273–282 Hemphill A, Stäger S, Gottstein B, and Müller N (1996) Electron microscopical investigation of surface alterations on Giardia lamblia trophozoites after exposure to a cytotoxic monoclonal antibody. Parasitol Res 82: 206–210 Henriquez F, Ingram PR, Muench SP, Rice DW, and Roberts CW (2008) Molecular basis for the resistance of Acanthamoeba tubulins to all major classes of antitubulin compounds. Antimicrob Agents Chemother 52: 1133–1135 Hoffman PS, Sisson G, Croxen MA, Welch K, Harman WD, Cremades N, and Morash MG (2007) Antiparasitic drug nitazoxanide inhibits the pyruvate oxidoreductases of Helicobacter pylori and selected anaerobic bacteria and parasites, and Campylobacter jejuni. Antimicrob Agents Chemother 51: 867–876 Horner DS, Hirt RP, and Embley TM (1999) A Single Eubacterial Origin of Eukaryotic Pyruvate: Ferredoxin Oxidoreductase Genes: implications for the Evolution of Anaerobic Eukaryotes. Mol Biol Evol 16: 1280–1291 Katiyar SK, Gordon VR, McLaughlin GL, and Edlind TD (1994) Antiprotozoal activities of benzimidazoles and correlations with β-tubulin sequence. Antimicrob Agents Chemother 38: 2086–2090 Khan IA, Avery MA, Burandt CL, Goins DK, Mikell JR, Nash TE, Azadegan A, and Walker LA (2000) Antigiardial activity of isoflavones from Dalbergia frutescens bark. J Nat Prod 63: 1414–1416 Kidwai M, Misra P, Kumar P (1998) The fluorinated quinolones. Curr Pharmaceut Design 4: 101–118 Kirk-Mason KE, Turner MJ, and Chakraborty PR (1988) Cloning and sequence of β-tubulin cDNA from Giardia lamblia. Nucleic acids Res 16: 2733 Kulakova L, Singer SM, Conrad J and Nash TE (2006) Epigenetic mechanisms are involved in the control of Giardia lamblia antigenic variation. Mol Microbiol 61: 1533–1542 Kwa MSG, Veenstra JG, Van Dijk, M, and Roos MH (1995) β-tubulin genes from the parasite nematode Haemonchus contortus modulate drug resistance in Caenorhabditis elegans. J Mol Biol 246: 500–516 Lauwaet T, Andersen Y, Van de Ven L, Eckmann L, and Gillin FD (2010) Rapid detachment of Giardia lamblia trophozoites as a mechanism of antimicrobial action of the isoflavone formononetin. J Antimicrob Chemother. doi:10.1093/ jac/dkp501 Leitsch D, Kolarich D, Binder M, Stadlmann J, Altmann F, and Duchêne M (2009) Trichomonas vaginalis: metronidazole and other nitroimidazole drugs are reduced by the flavin enzyme thioredoxin reductase and disrupt the cellular redox system. Implications for nitroimidazole toxicity and resistance. Mol Microbiol 72: 518–536 Lindquist AHD ( 1996) Induction of albendazole resistance in Giardia lamblia. Microb Drug Resist 2: 433–434 McFadden DC, Seeber F, and Boothroyd JC (1997) Use of Toxoplasma gondii expressing β-galactosidase for colori- Treatment of Giardiasis and Drug Resistance metric assessment of drug activity in vitro. Antimicrob Agents Chemother 41: 1849–1853 Morito K, Aomori T, and Hirose T (2002) Interaction of phytoestrogens with estrogen receptors alpha and beta (II). Biol Pharm Bull 25: 48–52 Mørch K, Hanevik K, Robertson LJ, Strand EA and Langeland N (2008) Treatment-ladder and genetic characterisation of parasites in refractory giardiasis after an outbreak in Norway. J Infect 56: 268–273 Müller J, Ley S, Felger I, Hemphill A. and Müller N (2008a) Identification of differentially expressed genes in a Giardia lamblia WB C6 clone resistant to nitazoxanide and metronidazole. J Antimicrob Chemother 62: 72–82 Müller J, Limban C, Stadelmann B, Missir AV, Chirita IC, Chifiriuc MC, Nitulescu GM and Hemphill A (2009a) Thioureides of 2-(phenoxymethyl)benzoic acid 4-R substituted: A novel class of anti-parasitic compounds. Parasitol Int 58: 128–135 Müller J, Naguleswaran A, Müller N, and Hemphill A (2008b) Neospora caninum: functional inhibition of protein disulfide isomerase by the broad-spectrum anti-parasitic drug nitazoxanide and other thiazolides. Exp Parasitol 118: 80– 88 Müller J, Nillius D, Hehl A, Hemphill A, and Müller N (2009) Stable expression of Escherichia coli beta-glucuronidase A (GusA) in Giardia lamblia: application to high-throughput drug susceptibility testing. J Antimicrob Chemother 64: 1187–1191 Müller J, Rühle G, Müller N, Rossignol, J-F, and Hemphill A. (2006) In vitro effects of thiazolides on Giardia lamblia WB C6 cultured axenically and in co-culture with Caco2 cells. Antimicrob Agents Chemother 50: 162–170 Müller J, Sidler D, Nachbur U, Wastling J, Brunner T, and Hemphill A (2008c) Thiazolides inhibit growth and induce glutathione-S-transferase pi (GSTP1)-dependent cell death in human colon cancer cells. Int J Cancer 123: 1797– 1806 Müller J, Sterck M, Hemphill A, and Müller, N (2007a) Characterization of Giardia lamblia WB C6 clones resistant to nitazoxanide and to metronidazole. J Antimicrob Chemother 60: 280–287 Müller J, Wastling J, Sanderson S, Müller N, and Hemphill A (2007b) A novel Giardia lamblia nitroreductase, GlNR1, interacts with nitazoxanide and other thiazolides. Antimicrob Agents Chemother 51: 1979–1986 Müller N and Gottstein B (1998) Antigenic variation and the murine immune response to Giardia lamblia. Int J Parasitol 28: 1829–1839 Müller N and von Allmen N (2005) Recent insights into the mucosal reactions associated with Giardia lamblia infections. Int J Parasitol 35: 1339–1347 Nash TE, Banks SM, Alling DW, Merritt JW, and Conrad JT (1990a) Frequency of variant antigens in Giardia lamblia. Exp Parasitol 71: 415–421 Nash TE, Conrad JT, and Merritt JW (1990b) Variant specific epitopes of Giardia lamblia. Mol Biochem Parasitol 42: 125–132 Nash TE, Ohl CA, Thomas E, Subramanian G, Keiser P, and Moore TA (2001) Treatment of patients with refractory giardiasis. Clin Infect Dis 33: 22–28 Nillius D, Müller J, and Müller N (2011) Nitroreductase (GlNR1) increases susceptibility of Giardia lamblia and Escherichia coli to nitro drugs. J Antimicrob Chemother 66: 1029–1035 Olekhnovich IN, Goodwin A and Hoffman PS (2009) Characterization of the NAD(P)H oxidase and metronidazole reductase activities of the RdxA nitroreductase of Helicobacter pylori. FEBS J 276: 3354–3364 Pankuch GA and Appelbaum PC (2006) Activities of tizoxanide and nitazoxanide compared to those of five other thiazolides and three other agents against anaerobic species. Antimicrob Agents Chemother 50: 1112–1117 Parkin DP (1996) Purine-specific Nucleoside N-Ribohydrolase from Trypanosoma brucei brucei. J Biol Chem 271: 21713– 21719 Parkin DP, Horenstein BA, Abdulah DA, Estupiian B, and Schramm VL (1991) Nucleoside hydrolase from Crithidia fasciculuta. J Biol Chem 266: 20658–20665 Ponce-Macotela M, Rufino-González Y, González-Maciel A, Reynoso-Robles R, and Martínez-Gordillo MN (2006) Oregano (Lippia spp.) kills Giardia intestinalis trophozoites in vitro: antigiardiasic activity and ultrastructural damage. Parasitol Res 98: 557–560 Prucca CG, Slavin I, Quiroga R, Elias EV, Rivero FD, Saura A, Carranza PG, and Lujan H (2008) Antigenic variation in Giardia lamblia is regulated by RNA interference. Nature 456: 750–754 Rayan P, Stenzel D, and McDonnell PA (2005) The effects of saturated fatty acids on Giardia duodenalis trophozoites in vitro. Parasitol Res 9: 191–200 Roxström-Lindquist K, Palm D, Reiner D, Ringqvist E, and Svärd SG (2006) Giardia immunity – an update. Trends Parasitol 22: 26–31 Shapiro TA, and Englund PT (1990) Selective cleavage of kinetoplast DNA minicircles promoted by antitrypanosomal drugs. Proc Natl Acad Sci USA 87: 950–954 Shi W, Schramm VL, and Almo SC (1999) Nucleoside hydrolase from Leishmania major. J Biol Chem 274: 21114–21120 Sisson G, Goodwin A, Raudonikiene A, Hughes NJ, Mukhopadhyay AK, Berg DA, and Hoffman PS (2002) Enzymes associated with reductive activation and action of nitazoxanide, nitrofurans, and metronidazole in Helicobacter pilori. Antimicrob Agents Chemother 46: 2116–2123 Sousa MC and Poiares-da-Silva J (2001) The cytotoxic effects of ciprofloxacin in Giardia lamblia trophozoites. Toxicol in vitro 15: 297–301 Sterk M, Müller J, Hemphill A, and Müller N (2007) Characterization of a Giardia lamblia WB C6 clone resistant to the isoflavone formononetin. Microbiol 153: 4150–4158 Su LH, Lee GA, Huang YC, Chen YH, and Sun CH (2007) Neomycin and puromycin affect gene expression in Giardia lamblia stable transfection, Mol Biochem Parasitol 156: 124–135 Svärd SG, Meng TC, and Hetsko ML, et al. (1998) Differentiation-associated surface antigen variation in the ancient eukaryote Giardia lamblia. Mol Microbiol 30: 979–989 Timmers LF, Pauli I, Barcellos GB, Rocha KB, Caceres RA, de Azevedo WF Jr, and Soares MB (2009) Genomic databases and the search of protein targets for protozoan parasites. Curr Drug Targets 10: 240–245 J. Müller et al. Townson SM, Upcroft JA, and Upcroft P (1996) Characterisation and purification of pyruvate:ferredoxin oxidoreductase from Giardia duodenalis. Mol Biochem Parasitol 79: 183– 93 Upcroft JA, Campbell RW, and Upcroft P (1996) Quinacrineresistant Giardia duodenalis. Parasitology 112: 309–313 Upcroft JA, Mitchell R, Chen N, and Upcroft P (1996) Albendazole resistance in Giardia is correlated with cytoskeletal changes but not with a mutation at amino acid 200 in β-tubulin. Microb. Drug Resist. 2: 303–308 Upcroft JA and Upcroft P (1993) Drug resistance and Giardia. Parasitol Today 9: 187–190 Upcroft P and Upcroft JA (2001) Drug targets and mechanisms of resistance in the anaerobic protozoa. Clin Microbiol Rev 14: 150–164 Wang CC (1997) Validating targets for antiparasite chemotherapy. Parasitol 114: Suppl S31–S44 Wilson WD, Mizan S, Tanious FA, Yao S, and Zon G (1994) The interaction of intercalators and groove-binding agents with DNA triple-helical structures: the influence of ligand structure, DNA backbone modifications and sequence. J Mol Recognit 7: 89–98 Wright JM, Dunn LA, Upcroft P, and Upcroft JA (2003) Efficacy of antigiardial drugs. Expert Opin Drug Saf 2: 529– 541