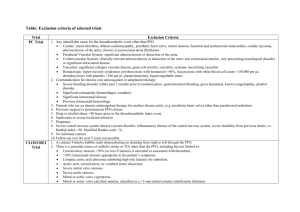
Anesthesia Student Survival Guide Jesse Ehrenfeld, Richard Urman, and Scott Segal, editors
advertisement

Anesthesia Student Survival Guide Jesse Ehrenfeld, Richard Urman, and Scott Segal, editors © 2010 Springer Science and Business Media CASE STUDY Chapter 17: Physiology & Anesthesia for Cardiac and Thoracic Surgery A 48 year-old woman presents for resection of extensive rectal hemorrhoids. She first developed the condition during pregnancies in her late 30s and now has had unremitting symptoms of pain, itching, and occasional bleeding. Her surgeon also plans to perform a “tension free vaginal tape” (TVT) procedure for moderate stress urinary incontinence. She has a history of rheumatic heart disease and has had progressively worsening mitral stenosis. She takes digoxin and a baby aspirin daily. How will you assess the severity of her mitral valve disease? The history and physical exam are important. One should evaluate for the presence and severity of symptoms of elevated left atrial and pulmonary pressures and systolic dysfunction (positional or exertional dyspnea, edema, weakness, exercise tolerance). An echocardiogram is usually done to follow the mitral valve disease, and you should obtain the most recent one (and older ones if possible, to evaluate progression of her disease). Even if these were done at an outside hospital, you should make the effort and even delay surgery, to obtain the reports prior to this elective procedure. On the echocardiogram report, you will focus on the valve area and estimated LVEDP (left atrial pressure estimate), pulmonary artery pressures, presence of mitral regurgitation and/or other valve lesions, regional wall motion abnormalities, and systolic function. You conclude that she has moderately severe mitral stenosis with moderately reduced systolic function. What are your hemodynamic goals for the perioperative period? A rule of thumb for valve disease is that stenotic lesions are kept “slow and tight,” while regurgitant lesions are kept “fast and full.” This means that you will avoid excessive volume loading to avoid pulmonary edema, peripheral vasodilation to avoid hypotension and compensatory increases in heart rate, and tachycardia. Patients with mitral stenosis are not able to increase stroke volume markedly in response to decreased arterial tone, and they do not tolerate the usual physiologic response to hypotension, an increase in heart rate, because it does not allow adequate time for ventricular filling across the stenotic mitral valve. Sinus rhythm is very beneficial in these patients, as the atrial kick can significantly augment ventricular filling. However, many patients are in atrial fibrillation due to the enlarged left atrium. In this case, ventricular rate control is vitally important. If she is in sinus rhythm, you will try to avoid triggers of atrial fibrillation such as excessive sympathetic activation or atrial stretch, and you will have drugs and cardioversion capability available should she develop uncompensated atrial fibrillation in the perioperative period. Anesthesia Student Survival Guide Jesse Ehrenfeld, Richard Urman, and Scott Segal, editors © 2010 Springer Science and Business Media Her cousin had a very similar procedure performed recently and had spinal anesthesia. She had spinal anesthesia herself for a cesarean section and was very pleased with it. She asks you if she can have this form of anesthesia for her current procedure. How will you respond? Spinal anesthesia is relatively contraindicated in significant mitral stenosis. This is because the decreases in preload due to venodilation and in “afterload” or peripheral arterial tone are poorly tolerated. Relatively high filling pressures are needed to fill the left ventricle across the stenosis, and as noted above, decreases in arterial tone cannot be compensated for by increasing stroke volume or heart rate. A carefully and slowly titrated epidural block has been successfully employed in cases of mitral stenosis, but this case will require dense sacral blockade, and epidural analgesia may spare or only partially block the sacral roots. Does she need antibiotic prophylaxis? Not necessarily. Previously, American Heart Association guidelines called for antibiotic prophylaxis for patients with valvular heart disease, including rheumatic heart disease, when undergoing dental, GI, or GU procedures. The most recent guidelines, published in 2007, now limit antibiotic recommendations to those with synthetic prosthetic valves, complex congenital heart disease, and patients with a previous history of infective endocarditis. The severity of the disease and likelihood of sustained bacteremia are potential factors that might elevate her risk and thus lead to recommended antibiotics, but routine GU and GI procedures are no longer considered indications for antibiotics solely on the basis of the risk of endocarditis. However, most surgical patients should receive prophylactic antibiotics to reduce the risk of surgical site infection, so you may choose to broaden your antibiotic coverage to include prophylaxis for her heart. You decide to administer general anesthesia. What drugs will you avoid? Which will you choose? You will avoid drugs with potent vasodilatory effects or tendency to produce tachycardia. Therefore, you may avoid propofol (vasodilation) and desflurane, pancuronium, ketamine, and anticholinergics (tachycardia). Nitrous oxide is controversial, since it can increase pulmonary artery pressure. Thiopental or etomidate would be reasonable choices for induction. Sevoflurane and short-acting opioids would be reasonable choices for maintenance. What other special precautions will you take in the intra- and post-operative periods? You will watch for bleeding, and treat volume loss aggressively, but avoid volume overload or accidentally infusing excess fluids without a specific indication. You wish to avoid shivering and other stimulants that could cause tachycardia. Therefore, good Anesthesia Student Survival Guide Jesse Ehrenfeld, Richard Urman, and Scott Segal, editors © 2010 Springer Science and Business Media pain and nausea prophylaxis are important. You will monitor her heart rhythm carefully and be prepared for rate control and cardioversion should she develop atrial fibrillation. Finally, you will be wary of position changes, such as putting the patient’s feet up into the lithotomy position, or down at the end of the case, which may cause hemodynamic challenges.