Ethical Considerations in the Management of
Infants Born at Extremely Low
Gestational Age
Naveed Hussain* and Ted S. Rosenkrantz*
With ongoing improvements in technology and the understanding of neonatal physiology, there has
been increasing debate regarding the gestational age and birth weight limits of an infants’ capability
of sustaining life outside the womb and how this is to be determined. The objective of this review was
to address this issue with an analysis of current data (following the introduction of surfactant therapy
in 1990) from published studies of survival in extremely low gestational age infants. We found that
survival was possible at 22 completed weeks of gestation but only in < 4% of live births reported.
Survival increased from 21% at 23 weeks gestational age to 46% at 24 weeks gestational age.
Historically, despite continual advances in neonatology, the mortality at 22 weeks has not improved
over the past three decades. Combining the data from studies on survival with evidence from
developmental biology, we believe that it is not worthwhile to pursue aggressive support of infants
born at < 23 weeks gestational age. Given the complicated issues related to morbidity and mortality
in infants born at 22 to 25 weeks gestational age and the ethical implications of the available evidence,
we propose the need for a consensus derived framework to help in decision-making.
© 2003 Elsevier Inc. All rights reserved.
ith the introduction of new therapies, improved technologies and greater experience in the management of extremely premature infants, survival for infants with birth
weights of 500 to 1,000 g (1 lb. 2 oz-2 lbs. 3 oz)
has shown improvement.1 This enhanced survival has encouraged some health care providers
and families to contemplate lowering the threshold for offering intensive care, now 23 to 24
weeks gestation and ⬃500 g birth weight, to a
lesser gestational age or weight at birth. The
medical and ethical considerations in this matter
are not well defined at present. The evolving
literature on the outcomes of extremely premature infants includes new information on the
range of morbidities in survivors, especially neurodevelopmental issues that have life-long implications for these infants and their families. This
review 1) presents evidence from the latest survival and neurodevelopmental outcome data
W
From the *Division of Neonatology, Departments of Pediatrics, University of Connecticut School of Medicine, Farmington, CT.
Address reprint requests to Naveed Hussain, MBBS, DCH, University of Connecticut School of Medicine, 263 Farmington Ave, Farmington, CT 06030-2948; e-mail: hussain@nso1.uchc.edu.
© 2003 Elsevier Inc. All rights reserved.
0146-0005/03/2706-0005$30.00/0
doi:10.1053/j.semperi.2003.10.005
458
and 2) incorporates this new information into
an evidence-based discussion of ethical dilemmas and decision-making for extremely premature infants.
Survival of Extremely-Low-GestationalAge Infants
The survival of low birth weight babies predates
modern neonatal intensive care units (NICUs).2
However, subsequent to the development of surfactant therapy, the survival of large numbers of
extremely premature infants has become routine. Until recently, reports of short- and longterm outcomes have been largely retrospective,
single center studies with small populations.3,4
Moreover, direct comparisons of survival reports
are hampered by lack of uniformity in reporting
data including analyses by birth weight versus
gestational age, inclusion/exclusions of stillbirths and delivery room deaths and use of prenatal steroids, surfactant therapy and other recent technologies since the early 1990s.
Recently, published reports from large multicenter and regional NICU-based studies have
added substantially to the data to facilitate making better informed, evidence-based, ethical decisions.5,6
Seminars in Perinatology, Vol 27, No 6 (December), 2003: pp 458-470
Ethics in Extremely Low Gestational Age Infants
The present dilemma is the inherent uncertainty in defining: at what milestone in an infants’ fetal development does the infant achieve
the capability of sustaining life outside the womb
and how is this to be determined? It has been
clearly shown that gestational age is a better
predictor of survival than birth weight.7 Gestational age is designated in completed weeks after
the last menstrual period. Therefore an infant
with gestational age of 23 weeks and 6 days is still
considered 23 weeks. The period of conception
is about 2 weeks after the last menstrual period
and therefore a gestational age (GA) of 23 weeks
corresponds to a conceptional age of 21 weeks.
By convention all analyses in clinical perinatal
medicine and neonatology are made using the
GA in completed weeks based on the last menstrual period. Is there a gestational age where it
is biologically improbable that an infant can sustain life outside the womb? The question is complex and needs to be addressed from multiple
perspectives including review of evidence, ethical principles and socio-economical underpinnings.
Data From Developmental Biology
The major factor limiting survival in infants of
extremely-low-gestational-age is the maturity of
the lung and its ability to perform effectively as
the organ for gas exchange. A large part of the
technology involved in sustaining life in the extremely-low-gestational-age infants relates to effective support for lung function (eg, surfactant
replacement, ventilators).
The vascular elements responsible for gas exchange in the fetal lung are not functional until
21 weeks GA (19 weeks conceptional age).8 The
development of an effective air exchange interface for gas diffusion is also not developed until
about 23 weeks GA (21 weeks conceptional
age).9,10 Therefore, structurally and physiologically the lung of a human fetus at 22 weeks
gestational age is largely incapable of effective
gas exchange and any life supporting technology
that is designated to support lung function will
not usually be effective at this gestation. Unless
there is an alternative treatment option that is
developed to facilitate gas exchange that does
not involve the lung (artificial placenta, extracorporeal membrane oxigenator [ECMO]), the
support of life at 22 weeks’ gestation will in all
459
likelihood be ineffective. Biological variations or
inconsistency of pregnancy dates may account
for the occasional survivors that are reported.
Data From Studies on Survival
Survival in premature infants has been significantly improved by the use of surfactant therapy
and newer ventilator technology in the 1990s.11
The age at which there is most controversy regarding survival is in infants born at ⱕ25 weeks
GA.12
Therefore, we have focused on reports from
studies of ⱕ25 weeks GA infants or birth
weight ⬍ 750 g born after 1990 (Tables 1 and 2,
respectively). Only studies conducted in developed countries with health care sophistication
comparable to the United States were compiled
in the tables.
Large population-based reports such as the
publications from the National Center for
Health Statistics linked birth-infant death cohort
files are not very useful in making determinations of survival at extremely low GAs due to
possible inaccuracies in gestational ages.13
Therefore, more specific data from centers focused on the care of extremely low gestation
infants needs to be the basis for evaluation. In
this review, we have compiled published studies
from developed countries of extremely low gestational age infants born between the years 1990
and 2000 (Table 1). Significant among these
studies have been some large multicenter NICU
based reports from the National Institute of
Child Health and Human Development (NICHD)
and the Vermont-Oxford Network. They have
reported survival and short-term neurodevelopmental outcomes from participating institutions.1,14-17 The NICHD network reported that
the post-surfactant era survival for infants is
⬃20% for infants born at 23 weeks’ gestation;
47% for infants born at 24 weeks and 68% for
infants born at 25 weeks’ gestation. The Vermont-Oxford Network reported similar trends in
survival.18 A summary of the compiled data from
table 1 shows that survival was ⬍ 3.5% at 22
weeks, 21% at 23 weeks, 46% at 24 weeks, and
66% at 25 weeks’ gestation.
A similar compilation of studies published
before 1997 was conducted by Hack and Fanaroff, who analyzed world and local (United
States) outcomes and found that survival varies
460
Table 1. Survival in Extremely Low Gestational Age Infants (1990-2000)
Birth Date
Country-center
From
To
Nishida54
Hagan55
Philip56
Hack57
B.-Singh58
Kilpatrick59
Emsley60
Batton61
Harper62
Doyle39
Fanaroff1
Bohin63
Battin64
Tin65
Jacobs66
Effer67
Joseph68
Bottoms12
Doyle69
Cartlidge70
Stevenson71
El-Metwally72
Ahner73
Teberg74
Hernandez75
Costeloe5
Wood76
Lemons6
Macfarlane77
Horbar78
Bucher79
Summary
Japan-multiple
Aust-region
US-single
US-single
US-single
US-single
UK-single
US-single
US-single
Aust-region
US-multiple
UK-single
Canada-single
UK-region
Canada-single
Canada-multiple
Canada-multiple
US-multiple
Aust-region
UK-region
US-multiple
US-single
US-single
US-single
US-single
UK ⫹ Ireland
UK-region
US-multiple
UK-region
International
Swiss
1990
1990
1990
1990
1990
1990
1990
1990
1990
1991
1991
1991
1991
1991
1991
1991
1991
1992
1992
1993
1993
1993
1993
1994
1994
1995
1995
1995
1995
1996
1996
1990
1991
1991
1992
1993
1994
1994
1995
1998
1992
1992
1993
1993
1994
1994
1996
1996
1993
1996
1994
1994
1997
1997
1995
1996
1995
1995
1996
2000
1996
1996
230-236 wk
240-246 wk
Total
n
Surv-n
(%)
Total
n
Surv-n
(%)
Total
n
36
128
3 (8.3)
0 (0)
118
15
42 (36)
3 (20)
18
8 (44)
27
6
1 (3.7)
0 (0)
27
22
2 (7.4)
9 (41)
16
32
3 (19)
13 (41)
40
31
37
43
52
5 (9.6)
37
21
49
32
1 (2.7)
1 (4.8)
1 (2)
5 (16)
13
80
44
22
0 (0)
24 (30)
11 (25)
1 (4.5)
19 (46)
4 (44)
5 (56)
15 (19)
26 (20)
26 (11)
65 (30)
13 (8)
112 (23)
406 (21)
6
0 (0)
27
0 (0)
7
92
0 (0)
11 (12)
11
0 (0)
22
1 (4.5)
9
133
22
138
56
84
404
2 (22)
0 (0)
2 (9.1)
2 (1.4)
12 (21)
0 (0)
7 (1.7)
41
9
9
78
131
241
216
162
479
1208
41 (3.4)
1946
Surv-n
(%)
250-256 wk
Total
n
Surv-n
(%)
16 (40)
21 (68)
18 (49)
17 (40)
22
40
56
36
40
37
14 (64)
33 (83)
35 (63)
26 (72)
31 (78)
20 (54)
63
280
95
42
78
42
406
21 (33)
132 (47)
27 (28)
19 (45)
13 (17)
25 (60)
216 (53)
49
88
361
104
48
103
59
454
37 (76)
51 (58)
246 (68)
38 (37)
28 (58)
36 (35)
39 (66)
370 (81)
116
59
31
312
61
18
10
127*
298
382
301
57 (49)
31 (53)
6 (19)
165 (53)
36 (59)
9 (50)
8 (80)
123
84
41
390
87
19
7
68*
357
424
379
85 (69)
63 (75)
19 (46)
273 (70)
71 (82)
14 (74)
5 (71)
767
14
3671
100 (34)
100 (26)
151 (50)
425 (55)
2 (14)
1623 (46)
825
54
4355
186 (52)
186 (44)
280 (74)
612 (74)
25 (46)
2823 (66)
NOTE. Data shown as number (percent) for survivors (Surv).
Abbreviations: LB, All live born infants except otherwise stated: Disch, survived to discharge from institution; NICU, Only NICU admissions.
*Malformations excluded.
†Excluded from present calculations.
Include
Survival
to
LB
LB
LB
LB
LB
LB
LB
LB
LB
LB
LB
LB*
LB
LB
NICU
LB
LB
LB
LB
LB*
LB
LB
LB
LB
LB
LB
LB
LB
LB
LB
LB
1-mo end
Disch
Disch
20-month
Disch
Disch
Disch
Disch
Disch
Disch
Disch
Disch
18-month
1 year
Disch
Disch
Disch
120d
Disch
1 year
Disch
Disch
Disch
Disch
Disch
Disch
Disch
Disch
Disch
Disch
Disch
Hussain and Rosenkrantz
Study
220-226 wk
Table 2. Survival in Infants With Birth Weight ⱕ750 g (1990-2000)
⬍ 500 g
Country-center
Birth Date
*Nishida54
Philip56
Hack57
Harper62
Fanaroff1
†Doyle80
Battin64
Joseph68
Bottoms12
Cartlidge70
Stevenson71
‡Teberg74
Tyson81
Hernandez75
Costoloe5
Lemons6
Horbar78
Anonymous82
Darlow83
Summary
Japan-multiple
US-single
US-single
US-single
US-multiple
Aust-region
Canada-single
Canada-multiple
US-multiple
UK-region
US-multiple
US-single
US-multiple
US-single
UK-multiple
US-multiple
International
Aust-region
NZ-center
1990
1990-91
1990-92
1990-98
1991-92
1991-92
1991-93
1991-96
1992-93
1993-94
1993-94
1994-95
1994-95
1991-96
1995
1995-96
1996
1997
1998-99
Total n
Survival n (%)
Total n
Survival n (%)
66
6 (9.1)
67
1 (1.5)
63
9
38
39
321
17 (27)
3 (33)
6 (16)
19 (49)
74 (23)
49
26
363
22
322
247
9 (18)
1 (3.8)
116 (32)
10 (45)
103 (32)
103 (42)
317
776
17
92 (29)
287 (37)
5 (29)
2609
845 (32)
16
86
15
360
33
195
481
5
13
1337
0 (0)
5 (5.8)
1 (6.7)
19 (5.3)
2 (6.1)
21 (10.8)
80 (16.6)
0 (0)
5 (38.5)
140 (10.5)
500-750 g
Total n
Survival n (%)
869
169
382 (44)
54 (32)
41
27 (66)
999
56
490 (49)
37 (66)
497
157 (32)
2631
1147 (44)
Ethics in Extremely Low Gestational Age Infants
Study
500-600 g
NOTE. All infants were live born infants. All survival was evaluated at discharge unless otherwise noted. Data shown as number (percent) for survivors.
*Survival at 1 month after close of study.
†Survival at 2-yr.
‡Malformations excluded.
461
462
Hussain and Rosenkrantz
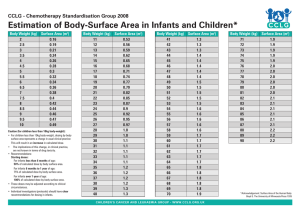
Figure 1. Temporal trends
in the survival of extremely
immature infants. (Data
from references 1, 18, 20,
56, 57, 65, and 74).
greatly.11 The reported survival ranges for infants born at 23 weeks gestation were 2%-35%; at
24 weeks were 17%-58%, and at 25 weeks were
35%-85%.11 These wide variations were reported
both within and between developed nations.
Evidence from Japan provides a unique perspective. Here, the Eugenics Protection Act
mandated resuscitation and support of infants
born at 22 weeks and they reported that survival
at 22 weeks is not impossible. However, the likelihood for survival to discharge from the hospital
was still ⬍ 10% in this population. Even if this is
not due to difference in prenatal care, racial
difference or regional variation, the very low
percent survival in this age group is not encouraging.
The contrary perspective is from a study of
practices in developing countries where a majority of neonatal centers consider the gestational
age of viability as 28 weeks.19
It could be inferred that “viability” is as much
a biologic threshold as it is a socio-economic
reality; and in a world where resources are not
limitless, this fact needs to be given sufficient
consideration.
Most of the evidence for the improbability of
technology helping in survival of an infant born
at 22 weeks comes from a compilation of available published data from developed nations like
United States, Canada, United Kingdom, Japan
and Australia; as shown in Table 1. Considering
that there is an inherent bias in published data
for evaluating results of only those infants that
survived long enough to be admitted to the intensive care units, the survival rate of ⬍ 3.5%
gives us an overly optimistic outcome. Therefore, for all practical purposes, survival of an
infant born at 22 weeks is extremely improbable.
The fact that this corresponds so closely to the
patho-physiologic limit of effective gas exchange
in the fetus reinforces its scientific basis.
The data from published studies in developed
countries on survival in infants with birth
weights ⱕ 750 g show a 10% survival in ⬍ 500 g
category (Table 2). These data based on birth
weight are not as helpful because a large number of more mature infants who were growth
restricted are also included.
Evidence From Temporal Trends in Survival
of Extremely-Low-Gestational-Age Infants
As shown in Figure 1, the gestational age at
which premature infants survived has become
lower over the past 30 years. In the early 1900s,
survival was highly unlikely in infants ⬍ 32-34
weeks. The beginning of neonatology as a disciple in the 1960s saw survivals at much younger
GA (28-30 weeks). In the 1970s, 24-26 weeks
infant survival became possible with more effective use of neonatal ventilators.20 Surfactant
therapy in the late 80s started to show improvements in survival and became standard in early
1990s. The NICHD reported the outcomes of
3 cohorts of very low birth weight infants
(⬍1500 g or 3 lbs. 5 oz) born prior to and after
Ethics in Extremely Low Gestational Age Infants
the licensure of surfactant. Survival steadily improved from presurfactant reports (1987-88) to
the mid-1990s.1,15
As of 1995-1996, about half (54%) of 501-750
g birth weight infants and over 80% of 751-1000
g infants survived to discharge home. However, a
major report from the Vermont-Oxford Network
from a total of 118,448 infants (501-1500 g birth
weight) born between 1991-1999 from 363 institutions showed no significant improvement in
survival rates for infants 501-750 g, especially
after 1994.18 One of the explanations offered to
this leveling off of mortality was that, “we may
have reached the limits of current technology to
support preterm infants at gestational ages near
the limits of viability.”18
With respect to the earliest gestational age at
which survival was seen as a reasonable possibility, there does not appear to have been a significant change since the routine use of prenatal
steroid and postnatal surfactant therapy as
shown in Figure 1. The NY State Task Force on
Life and Law: Report on Fetal Extrauterine Survivability of extremely premature infants in the
mid 1980s concluded that 23 weeks was the
lower limit of viability.21 The advent of surfactant
replacement therapy for the lungs (1991), increased use of prenatal steroids (mid 1990s) and
the use of new and sophisticated ventilatory
strategies in the 1990s have not lowered the threshold of viability (Fig 1). This may be considered
historical evidence of the gestational age-limit at
which viability is considered a reasonable possibility.
Polled Opinions of Health Care Providers
and Academics
There have been a number of surveys with questionnaires designed to determine the opinion of
doctors, nurses, parents of premature infants
and lay people regarding setting limits for active
treatment of extremely premature infants.22-29
None suggested initiation of aggressive therapy
at 22 weeks unless it was an exceptional situation. Guidelines from various professional
groups including the NY State Task Force on
Life and Law: Report on Fetal Extrauterine Survivability, Canadian Pediatric Society, British Association of Perinatal Medicine, and the American Academy of Pediatrics also reiterate that
active treatment of 22 weeks infants is not indi-
463
cated except in some special situations.21,30-34
The International Guidelines for Neonatal Resuscitation states that “the non-initiation of resuscitation in the delivery room is appropriate
for infants with confirmed gestation ⬍ 23 weeks
or birth weight ⬍ 400 g. In cases of uncertain
prognosis including uncertain gestational age,
resuscitation options include a trial of therapy
and noninitiation or discontinuation of resuscitation after assessment of the infant”.35
Influence of Site of Delivery On Survival
Does the site of delivery have an impact on the
survival or quality of life in survivors? Hack
noted that there are wide variations in survival
among developed and developing countries.11
Even among the developed countries like the
United States, there are variations in outcome
related to the site of the infant’s birth. Yeast
recently revisited this issue in a comparison of
live births and neonatal mortality (death ⬍ 28
days) in the state of Missouri for the periods
1982-1986 vs. 1990-1994.36 There was significantly decreased mortality with increased levels
of care of the birth hospital. Extremely premature infants (500-1000 g) had 66% mortality if
born at a center providing only basic newborn
care (level 1); 51% mortality at a center with
short-term care facilities for sick newborns (level
2), and only 32% mortality at a center equipped
to provide comprehensive multispecialty neonatal intensive care (level 3).36
A regional study from Vienna, Austria showed
a lower morbidity in infants who were transported prenatally in utero to tertiary care centers.37 In another large study of infants born
between 1968-1994 in North Carolina, Bode
found decreases in mortality for infants with
birth weights 500-1000 g with increasing levels of
available care.38 A regional evaluation from the
Victorian Infant Collaborative Study Group in
Australia also concluded that the prognosis for
infants born at ⱕ 27 weeks gestation is better
when delivered at tertiary care centers.39 These
studies and others continue to support the survival advantages of birth in hospitals providing
comprehensive and subspecialty care for extremely premature infants.
Time
Neurodevelopmental Outcomes in
Survivors of Extremely-Low-GestationalAge Infants
VHM
Predict
VHCM
VHCM
VHCM
VHCM
VHCM
VHCM
Predict
VHCM
VHCM
VHCM
17 (35%)
26
25 (96)
30
16 (53)
20
11 (55)
51
13 (25)
20
7 (35)
36
8 (22)
34
4 (12)
52
28 (54)
10
3 (30)
182
88 (48)
7
4 (57)
21 (100)
13 (72)
14 (82)
7 (33)
4 (29)
5 (39)
4 (17)
19 (66)
2 (22)
52 (54)
2 (66)
2 (40)
1 (100)
0 (0)
1 (20)
10 (33)
1 (33)
14 (56)
Disabled
21
18
17
21
14
13
23
29
9
97
4 (80)
1 (50)
5
2
Total N ⫽ 49
9
9 (100)
US-single
US-single
US-single
UK-single
Aust-region
Canada-single
UK-region
Canada-single
US-multiple
US-single
UK-region
Dutch-region
Hack57
B.-Singh58
Piecuch84
Emsley60
Doyle39
Battin64
Tin65
Jacobs66
Bottoms12
Ahner73
Wood76
Rijken85
1990
1990
1990
1990
1991
1991
1991
1991
1992
1993
1995
1996
1992
1993
1994
1994
1992
1993
1994
1994
1993
1997
1995
1997
All GA combined
3
5
1
1
5
15
3
25
Disabled
n (%)
Total
n
Disabled
n (%)
Total
n
Disabled
n (%)
Total
n
Disabled
n (%)
Total
n
To
From
Country-center
Study
250-256 wk
240-246 wk
230-236 wk
220-226 wk
Even these extremely premature infants with
normal cognitive abilities and global IQ ⱖ85 are
at risk for significant learning issues in school.
Whitfield compared 115 surviving ⬍ 800 g birth
weight infants born in 1974-1985 with 50 term
infants matched for age and sociodemographical factors at elementary school age (7-10
years).41 Extremely premature infants who were
in the “normal cognitive range” with global IQ
85 scored significantly lower in fine and gross
motor control, visual-motor pencil output, visual
memory and academic achievement (reading,
arithmetic and written language) compared to
term infants. Extremely premature infants were
also three times as likely to have learning disabilities (47% v 18%). Only 12% of extremely premature boys, and 35% of girls were without disabilities. A geographical cohort study of 298
Birth date
School Age Outcomes: (>5 Years)
Table 3. Neuro-developmental Disabilities in Survivors of Extremely Low Gestational Age Infants (1990-2000)
A number of studies have reported on neurodevelopmental outcomes in survivors of extremely
low gestational age infants. A summary of the
reports of infants born after 1990 classified by
gestational age at birth is shown in Table 3. One
of the largest and best designed studies on developmental and functional outcomes in infants
was recently reported from the NICHD.40 Fourteen hundred and eighty (1,480) surviving infants born between 1993-1994 with birth weights
500-1000 g, were evaluated for neurodevelopmental, neurosensory and functional assessment
at 18-22 months’ of age corrected for their prematurity. Results were reported by 100 g birth
weight increments. On the Bayley Scales of Infant Development-II Mental Development Index
(MDI), two thirds (66%) of the surviving infants
scored ⬍85, and a third (37%) scored ⬍70 (in
the mental retardation range). The Psychomotor Development Index (PDI) scores were similar. The incidence of cerebral palsy (abnormal
neurological examination) was 17%. The incidence of one or more major neurodevlopmental
handicaps (cerebral palsy, mental retardation,
blindness or deafness) was seen in 49% of infant
survivors born with birth weights 500-1000 g.
Assess
Early Outcome: (0-3 Years)
Abbreviations: V, visual deficit; H, hearing deficit; C, cerebral palsy; M, mental retardation; Disch, assessment done at discharge; Predict, predicted assessment based on neonatal
findings; Assess, parameters assessed at follow-up; Time, age at which follow-up evaluation done.
Hussain and Rosenkrantz
20-mo
Disch
1 yr
19mo-10yr
5yr
18 mo
1 year
18-24 mo
Disch-120d
1 yr
30 mo
2 yr
464
Ethics in Extremely Low Gestational Age Infants
consecutive extremely low birth weight (⬍1000 g)
survivors born between 1991-1992 in Victoria
region of Australia showed significant cognitive,
educational and behavioral deficits at 8 years of
age compared to normal birth weight controls.42
Furthermore, school function may deteriorate over time as academic tasks become more
complex. Botting followed a cohort of 138 very
low birth weight infants birth weight infants
throughout school and found that the performance in all areas of academic achievement was
worse at 12 years old than it was at 6 years.43
Newer evidence has begun to correlate decreased neurological function with decreased
brain volume in specific areas of the cerebral
cortex even in infants where there were no lesions identified on ultrasound evaluations in the
neonatal period.44,45 It is quite possible that the
development of the brain in these extremely
immature infants does not proceed normally
and the reasons may be related to their illness,
nutritional deprivation or other unknown factor(s).
Evidence-based Ethics
What are the ethical implications of the evolving
data on survival and morbidities for families and
health care providers caring for these extremely
premature infants? Earlier generations of health
care providers had only single center studies,
their own hospital’s results and their “hopes” for
improved outcomes for these tiniest of patients
to guide their decision-making. However, practicing neonatologists and families are now empowered by an evolving literature of short- and
intermediate-term survival and neurodevelopmental outcomes.
The ethical implications of this “new” literature encompass a number of areas of potential
controversy and conflict including:
1. Where does the current lower limit of viability lie?
2. What is the role of parental input in resuscitation and ongoing care decisions for extremely premature infants in light of current
outcomes data?
3. What should happen when health care providers and parents disagree?
465
The Current Limit Of Viability
Since the advent of modern newborn intensive
care the “lower limit of viability” has been reassessed due to changes in therapies and outcomes. In 1988, the NY State Task Force on Life
and Law: Report on Fetal Extrauterine Survivability, reported that epidemiological and biologic evidence suggested that the lower limit of
viability was 23-24 weeks gestational age.21 The
studies cited earlier in this review on survival and
neurodevelopmental outcomes for extremely
premature infants continue to reinforce that we
have reached a current lower biologic limit at 23
weeks’ gestation and approximately 400-500 g
birth weight. While there have been isolated
reports of surviving infants who are born at ⬍ 23
weeks’ gestation or with birth weights ⬍ 400 g,
these unusual survivals probably represent the
outliers in any normative population and fail to
make a compelling argument for routinely offering resuscitation to less mature and/or smaller
infants. Even though the determination of “limit
of viability” is a clinically and ethically simplistic
goal,46 the vast majority of health care providers
in the United States express the need for nonbinding guidelines that will establish standards
of care while leaving room for individual decisions in exceptional circumstances.47
In addition to the high mortality, especially
for infants born at 23-24 weeks’ gestation, evolving information also indicates that extremely
premature infants are at very high risk for neurological and cognitive impairment. In the
NICHD neurodevelopmental outcomes study of
infants born in the mid-1990s, even infants with
birth weights close to 1000 g had mean developmental quotients in the low average/borderline
range.
The American Academy of Pediatrics (AAP)
has published policy recommendations for management of extremely premature infants.34 However, the AAP statement is vague and does not
give substantive recommendations. The joint
group of the Canadian Pediatric Society and the
Maternal-Fetal Medicine Committee and Society
of Obstetricians and Gynecologists of Canada
have developed practical recommendations
based upon available data and provide a good
example of evidence-based medicine in this
field.32,33 Consistent with the data, the Canadian
guidelines recommend 1) withholding resuscita-
466
Hussain and Rosenkrantz
tion for infants born at ⬍ 23 weeks’ gestation; 2)
joint decision-making with families for infants
born at 23-24 weeks’ gestation; and 3) routine
initiation of resuscitation for most infants born
at 25 weeks’ gestation or older.
Important pieces of evidence can be derived
from reports from institutions that have tried a
policy of resuscitating infants at extremely low
gestational ages; and after reviewing the dismal
outcomes have reverted their policy.48,49 One is
based on a study from Leiden, Netherlands
where a policy of resuscitating infants born at
⬍25 weeks resulted in an unacceptably high
mortality and morbidity.49 The other is a study
based on a 4-year experience (1994-1998) in a
single center in California, of instituting aggressive resuscitation for all infants ⱖ 450 g or ⱖ 22
weeks GA.48 Their review of death and morbidity
led them to revise their policy to offer resuscitation only to those infants’ ⱖ 500 g or ⱖ 24
weeks. Resuscitation below 500 g birth weight or
at ⬍ 23 weeks was considered only in exceptional circumstances. The available evidence
from these quality assessment cycles of “new
policy3implementation3 assessment3policy
revision”, needs to be considered in designing
future policy.
The Role of Parental Input in Resuscitation
Decisions for Extremely Premature Infants
The philosophical framework for shared medical decision-making for infants between parents
and health care providers recognizes the primary responsibility and right of parents to make
medical decisions in the best interests of their
children. Within this framework, parents are
given considerable latitude to make decisions,
even if unpopular with the health care team.
However, this responsibility is not absolute and
inevitably, there will be occasional conflicts between parents making decisions and health care
providers who have a different view of a child’s
best interests.
Several reports suggest that the vast majority
of neonatologists consider parental wishes when
making resuscitation decisions for infants born
at 23 weeks gestational age.24,50 However, as gestational age increases by weekly increments from
24 to 26 weeks’ gestation, neonatologists become increasingly uncomfortable with a priori
decisions “not to resuscitate.”29 Among other
considerations, the knowledge that continued
re-evaluation of the benefits of ongoing intensive care after resuscitation can reopen discussions with parents may comfort some neonatologists who are ambivalent about initiating
intensive care in tiny babies.
Societal support for the role of parental decision-making in these complex cases is illustrated
by the State vs. Messenger case. While legal action
was taken against a father who discontinued life
support in a NICU from his critically ill 25 weeks
gestational age infant, the jury acquitted the
father of charges of manslaughter.51 Such tragic
cases continue to remind health care providers
of the importance of dialogue with families, of
consistency with other health care providers in
agreements with families, and of the importance
of re-evaluating care if the response to initial
resuscitation is poor or other complications intervene.52,53
Disagreements Between Parents and Health
Care Providers
For those few situations in which health care
providers and families find themselves in irreconcilable conflict, several avenues for conflict
resolution are present. Often consultation with a
peer colleague and continued discussion with
the parents will lead to reasoned resolution of
the previous disagreement. If that fails, neonatologists should take advantage of ethical consultation or formal review by an infant care review
team after informing the parents. The opportunity to openly discuss difficult issues with the full
range of health care providers with the family
present, if desired, often clarifies medical issues
and gives comfort to both the parents and the
health care team that the infant’s best interests
are being considered and protected. The recommendations of the infant care review team are
considered opinions only and are nonbinding.
In extremely unusual cases, either the parents
or the health care team will find it necessary to
seek legal action to resolve a health care crisis. If
a medical decision-making conflict appears to be
heading in the direction of outside intervention,
formal legal advice must be promptly sought.
The physician and health care team must also
Ethics in Extremely Low Gestational Age Infants
realize that legal action is easier initiated than
carried on to its final resolution. The last place
one really wants to be with any medical/ethical
conflict is in a court of law where decisions are
often made based upon narrowly defined legal
precepts. Both the health care provider(s) and
the family may find the outcome unacceptable.
Who decides if the burdens of life saving technology for a particular infant are worth the benefit? The following is a list of the possible final
decision makers and their challenges:
1. Parent or family unit alone – Historically,
legal opinions have favored the family’s right
to make decisions. Unfortunately the family
in the vast majority of situations lacks complete understanding of the infants’ problems
or potential outcomes and therefore is not in
the best situation to make informed decisions.
2. Parent-Physician team dialogue: This is the
best way to get informed opinion and consent
for potentially burdensome and untested
therapy and gives credence to surrogate (parent) autonomy, gives weight to benefit-risk
analysis and has the potential to avoid nonmalfeasance. However, each circumstance
needs a complete reappraisal of available
data and in practice, there may not be
enough time or opportunity to do this.
3. Institutional policy or protocol: This provides
an equitable approach to the problem but
suffers from lack of autonomy of both the
parent and physician group. Moreover, if different institutions have varying policies, there
will be confusion and the potential for legal
contentions may increase.
4. Societal policy-guidelines: This provides a just
and equitable approach and also takes into
account larger socio-economical and policy
issues. It takes the agony of constant re-interpretation of ethical principles away from the
delivery room or the intensive care unit and
provides a framework in which individual discussions can best be made. There are models
for effective use of this approach in the guidelines in use in Canada and in some states in
the United States. The limitation of parental
autonomy may have to be the price that is
paid with this approach.
467
Future Directions
What Should We Do With This Evolving
Information?
Given the currently available information on the
survival and intermediate-term neurodevelopmental outcomes of extremely premature infants, our efforts should focus upon improving
short- and long-term outcomes for infants for
whom we currently care, not on altering the
lower limit of viability. As part of these efforts, we
should ensure that families are given useful information both prior to and after delivery to
enhance their decisional capabilities and to empower them to advocate for their infants both in
the short and long-term. This information
should include current survival information and
morbidities both for the birth hospital and for
some regionally or nationally recognized comparison group. Given the available information
on outcomes of infants based upon the level of
neonatal services in the birth hospital, families
who will potentially deliver an extremely premature infant should routinely be offered transfer
to a center offering comprehensive neonatal intensive care services, if time and circumstances
allow.
Meeting the needs of developing, former premature infants will require cooperation and collaboration among families, neonatologists, primary health care providers after discharge, early
interventionists and educators. Neonatologists
need to extend their influence outside the nursery and into the community to ensure that the
anticipated needs of their smallest patients are
optimally addressed. They should provide data
to local schools and state Departments of Education to assist in their planning for the ongoing
educational needs of these tiny survivors. Current data suggests that nearly all surviving extremely premature boys and about two thirds of
girls will require special help in school.
Finally, we need to encourage and support
multicenter, collaborative follow-up efforts to
obtain feedback on the outcomes of these critically ill infants. Large datasets on extremely premature infants from birth through adolescence
are essential to assist us in informing parents and
planning for the future of these infants.
The advent of modern newborn intensive
468
Hussain and Rosenkrantz
care and critical technologies such as prenatal
steroids and surfactant have dramatically enhanced the likelihood of survival for extremely
premature infants, especially for those born at
greater than 24 weeks’ gestation. However, both
short- and long-term morbidity remains high.
Barring dramatic technologic breakthroughs
such as an artificial placenta, we have probably
reached a biologic limit at 23 weeks’ gestation
and/or 400-500 g birth weight. The challenge
now lies in addressing the issues compromising
the quality of survival of the tiniest and most
vulnerable of our patients.
11.
12.
13.
14.
Acknowledgment
We acknowledge the contributions of Dr Marilyn
Sanders, who was instrumental in initiating this review
and was extremely helpful in reviewing the manuscript.
15.
16.
References
1. Fanaroff AA, Wright LL, Stevenson DK, et al: Very-lowbirth-weight outcomes of the National Institute of Child
Health and Human Development Neonatal Research
Network, May 1991 through December 1992. Am J Obstet Gynecol 173:1423-1431, 1995
2. Monro JS: A premature infant weighing less than one
pound at birth who survived and developed normally.
Can Med Assoc J 40:69-70, 1939
3. Allen MC, Donohue PK, Dusman AE: The limit of viability–neonatal outcome of infants born at 22 to 25
weeks’ gestation. N Engl J Med 329:1597-1601, 1993
4. Hussain N, Galal M, Ehrenkranz RA, et al: Pre-discharge
outcomes of 22-27 weeks gestational age infants born at
tertiary care centers in Connecticut implications for
perinatal management. Conn Med 62:131-137, 1998
5. Costeloe K, Hennessy E, Gibson AT, et al: The EPICure
study: outcomes to discharge from hospital for infants
born at the threshold of viability. Pediatrics 106:659-671,
2000
6. Lemons JA, Bauer CR, Oh W, et al: Very low birth weight
outcomes of the National Institute of Child health and
human development neonatal research network, January 1995 through December 1996. NICHD Neonatal
Research Network. Pediatrics 107:E1, 2001
7. Kohn MA, Vosti CL, Lezotte D, et al: Optimal gestational
age and birth-weight cutoffs to predict neonatal morbidity. Med Decis Making 20:369-376, 2000
8. deMello DE, Reid LM: Embryonic and early fetal development of human lung vasculature and its functional
implications. Pediatr Dev Pathol 3:439-449, 2000
9. Barbet JP, Houette A, Barres D, et al: Histological assessment of gestational age in human embryos and fetuses.
Am J Forensic Med Pathol 9:40-44, 1988
10. DiMaio M, Gil J, Ciurea D, et al: Structural maturation of
17.
18.
19.
20.
21.
22.
23.
24.
25.
the human fetal lung: A morphometric study of the
development of air-blood barriers. Pediatr Res 26:88-93,
1989
Hack M, Fanaroff AA: Outcomes of children of extremely low birthweight and gestational age in the
1990’s. Early Hum Dev 53:193-218, 1999
Bottoms SF, Paul RH, Iams JD, et al: Obstetric determinants of neonatal survival: influence of willingness to
perform cesarean delivery on survival of extremely lowbirth-weight infants. National Institute of Child Health
and Human Development Network of Maternal-Fetal
Medicine Units. Am J Obstet Gynecol 176:960-966, 1997
Alexander GR, Kogan M, Bader D, et al: US birth
weight/gestational age-specific neonatal mortality: 19951997 rates for whites, hispanics, and blacks. Pediatrics
111:e61-66, 2003
Anonymous: The Vermont-Oxford Trials Network: very
low birth weight outcomes for 1990. Investigators of the
Vermont-Oxford Trials Network Database Project. Pediatrics 91:540-545, 1993
Hack M, Horbar JD, Malloy MH, et al: Very low birth
weight outcomes of the National Institute of Child
Health and Human Development Neonatal Network.
Pediatrics 87:587-597, 1991
Blair BM, O’Halloran H S, Pauly TH, et al: Decreased
incidence of retinopathy of prematurity, 1995-1997. J
Aapos 5:118-122, 2001
Bernstein IM, Horbar JD, Badger GJ, et al: Morbidity
and mortality among very-low-birth-weight neonates with
intrauterine growth restriction. The Vermont Oxford
Network. Am J Obstet Gynecol 182:198-206, 2000
Horbar JD, Badger GJ, Carpenter JH, et al: Trends in
mortality and morbidity for very low birth weight
(VLBW) infants: The Vermont Oxford Network Experience, 1991-1999. Pediatric Research 49:303A, 2001
Straughn HK, Goldenberg RL, Tolosa JE, et al: Birthweight-specific neonatal mortality in developing countries and obstetric practices. Int J Gynaecol Obstet 80:
71-78, 2003
Koops BL, Morgan LJ, Battaglia FC: Neonatal mortality
risk in relation to birth weight and gestational age: update. J Pediatr 101:969-977, 1982
Anonymous: Fetal extrauterine survivability: Report of
the Committee on Fetal and Extrauterine Survivability to
the New York State task Force on Life and the Law. New
York, New York State Task Force on Life and the Law,
1988
Streiner DL, Saigal S, Burrows E, et al: Attitudes of
parents and health care professionals toward active treatment of extremely premature infants. Pediatrics 108:
152-157, 2001
Sanders MR, Donohue PK, Oberdorf MA, et al: Perceptions of the limit of viability: neonatologists’ attitudes
toward extremely preterm infants. J Perinatol 15:494502, 1995
Sanders MR, Donohue PK, Oberdorf MA, et al: Impact
of the perception of viability on resource allocation in
the neonatal intensive care unit. J Perinatol 18:347-351,
1998
Saigal S, Stoskopf BL, Feeny D, et al: Differences in
preferences for neonatal outcomes among health care
Ethics in Extremely Low Gestational Age Infants
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
professionals, parents, and adolescents. JAMA 281:19911997, 1999
Oei J, Askie LM, Tobiansky R, et al: Attitudes of neonatal
clinicians towards resuscitation of the extremely premature infant: an exploratory survey. J Paediatr Child
Health 36:357-362, 2000
De Leeuw R, Cuttini M, Nadai M, et al: Treatment
choices for extremely preterm infants: an international
perspective. J Pediatr 137:608-616, 2000
McElrath TF, Norwitz ER, Nour N, et al: Contemporary
trends in the management of delivery at 23 weeks’ gestation. Am J Perinatol 19:9-15, 2002
Cummings B, McKay K, Hussain N: Neonatologists’
opinions regarding resuscitation of extremely premature infants in Connecticut and Rhode Island. Conn
Med 66:733-738, 2002
Fetuses and Newborn Infants at the Threshold of Viability. In A Framework for practice. Vol 2003, British Association of Perinatal Medicine, 2000, pp http://www.
bapm.org/documents/publications/threshold.pdf
ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrcian-Gynecologists: Number 38, September 2002. Perinatal care at the threshold of viability.
Obstet Gynecol 100:617-624, 2002
Anonymous: Management of the woman with threatened birth of an infant of extremely low gestational age.
Fetus and Newborn Committee, Canadian Paediatric
Society, Maternal-Fetal Medicine Committee, Society of
Obstetricians and Gynaecologists of Canada. Can Med
Assoc J 151:547-553, 1994
Anonymous: Perinatal care at the threshold of viability.
American Academy of Pediatrics Committee on Fetus
and Newborn. American College of Obstetricians and
Gynecologists Committee on Obstetric Practice. Pediatrics 96:974-976, 1995
MacDonald H: Perinatal care at the threshold of viability. Pediatrics 110:1024-1027, 2002
Niermeyer S, Kattwinkel J, Van Reempts P, et al: International Guidelines for Neonatal Resuscitation: An excerpt from the Guidelines 2000 for Cardiopulmonary
Resuscitation and Emergency Cardiovascular Care: International Consensus on Science. Contributors and Reviewers for the Neonatal Resuscitation Guidelines. Pediatrics 106:E29, 2000
Yeast JD, Poskin M, Stockbauer JW, et al: Changing
patterns in regionalization of perinatal care and the
impact on neonatal mortality. Am J Obstet Gynecol 178:
131-135, 1998
Hohlagschwandtner M, Husslein P, Klebermass K, et al:
Perinatal mortality and morbidity. Comparison between
maternal transport, neonatal transport and inpatient
antenatal treatment. Arch Gynecol Obstet 265:113-118,
2001
Bode MM, O’Shea TM, Metzguer KR, et al: Perinatal
regionalization and neonatal mortality in North Carolina, 1968-1994. Am J Obstet Gynecol 184:1302-1307,
2001
Doyle LW: Outcome at 5 years of age of children 23 to 27
weeks’ gestation: Refining the prognosis. Pediatrics 108:
134-141, 2001
Vohr BR, Wright LL, Dusick AM, et al: Neurodevelopmental and functional outcomes of extremely low birth
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
469
weight infants in the National Institute of Child Health
and Human Development Neonatal Research Network,
1993-1994. Pediatrics 105:1216-1226, 2000
Whitfield MF, Grunau RV, Holsti L: Extremely premature (⬍ or ⫽ 800 g) schoolchildren: Multiple areas of
hidden disability. Arch Dis Child Fetal Neonatal Ed 77:
F85-90, 1997
Anderson P, Doyle LW: Neurobehavioral outcomes of
school-age children born extremely low birth weight or
very preterm in the 1990s. JAMA 289:3264-3272, 2003
Botting N, Powls A, Cooke RW, et al: Cognitive and
educational outcome of very-low-birthweight children in
early adolescence. Dev Med Child Neurol 40:652-660,
1998
Ment LR, Vohr B, Allan W, et al: Change in cognitive
function over time in very low-birth-weight infants. JAMA
289:705-711, 2003
Peterson BS, Anderson AW, Ehrenkranz R, et al: Regional brain volumes and their later neurodevelopmental correlates in term and preterm infants. Pediatrics
111:939-948, 2003
Lorenz JM: Survival of the extremely preterm infant in
North America in the 1990s. Clin Perinatol 27:255-262,
2000
Catlin AJ: Physicians’ neonatal resuscitation of extremely
low-birth-weight preterm infants. Neonatal Netw 19:2532, 2000
Sweet MP, Hodgman JE, Pena I, et al: Two-year outcome
of infants weighing 600 grams or less at birth and born
1994 through 1998. Obstet Gynecol 101:18-23, 2003
Sheldon T: Dutch doctors change policy on treating
preterm babies. BMJ 322:1383, 2001
Partridge JC, Freeman H, Weiss E, et al: Delivery room
resuscitation decisions for extremely low birthweight infants in California. J Perinatol 21:27-33, 2001
State v Messenger. In Clerk of the Circuit Court. Vol File
94-67694-FY, County of Ingham, Michigan, 1994
Clark FI: Making sense of State v Messenger. Pediatrics
97:579-583, 1996
Paris JJ: Manslaughter or a legitimate parental decision?
The messenger case. J Perinatol 16:60-64, 1996
Nishida H, Ishizuka Y: Survival rate of extremely low
birthweight infants and its effect on the amendment of
the Eugenic Protection Act in Japan. Acta Paediatr Jpn
34:612-616, 1992
Hagan R, Benninger H, Chiffings D, et al: Very preterm
birth–A regional study. Part 2: The very preterm infant.
Br J Obstet Gynaecol 103:239-245, 1996
Philip AG: Neonatal mortality rate: is further improvement possible? J Pediatr 126:427-433, 1995
Hack M, Friedman H, Fanaroff AA: Outcomes of extremely low birth weight infants. Pediatrics 98:931-937,
1996
Bahado-Singh RO, Dashe J, Deren O, et al: Prenatal
prediction of neonatal outcome in the extremely lowbirth-weight infant. Am J Obstet Gynecol 178:462-468,
1998
Kilpatrick SJ, Schlueter MA, Piecuch R, et al: Outcome
of infants born at 24-26 weeks’ gestation: I. Survival and
cost. Obstet Gynecol 90:803-808, 1997
Emsley HC, Wardle SP, Sims DG, et al: Increased survival
and deteriorating developmental outcome in 23 to 25
470
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
Hussain and Rosenkrantz
week old gestation infants, 1990-4 compared with
1984-9. Arch Dis Child Fetal Neonatal Ed 78:F99-104,
1998
Batton DG, DeWitte DB, Espinosa R, et al: The impact of
fetal compromise on outcome at the border of viability.
Am J Obstet Gynecol 178:909-915, 1998
Harper RG, Rehman KU, Sia C, et al: Neonatal outcome
of infants born at 500 to 800 grams from 1990 through
1998 in a tertiary care center. J Perinatol 22:555-562,
2002
Bohin S, Draper ES, Field DJ: Impact of extremely immature infants on neonatal services. Arch Dis Child Fetal
Neonatal Ed 74:F110-113, 1996
Battin M, Ling EW, Whitfield MF, et al: Has the outcome
for extremely low gestational age (ELGA) infants improved following recent advances in neonatal intensive
care? Am J Perinatol 15:469-477, 1996
Tin W, Wariyar U, Hey E: Changing prognosis for babies
of less than 28 weeks’ gestation in the north of England
between 1983 and 1994. Northern Neonatal Network.
BMJ 314:107-111, 1997
Jacobs SE, Whyte HE, Kelly EN, et al: Pre and post
surfactant: Outcome of inborn and outborn infants,
23-26 weeks’ gestation. Pediatric Research 41:199A, 1997
Effer SB, Moutquin JM, Farine D, et al: Neonatal survival
rates in 860 singleton live births at 24 and 25 weeks
gestational age. A Canadian multicentre study. Br J Obstet Gynecol 109:740-745, 2002
Joseph KS, Marcoux S, Ohlsson A, et al: Preterm birth,
stillbirth and infant mortality among triplet births in
Canada, 1985-96. Paediatr Perinat Epidemiol 16:141148, 2002
Doyle LW, Gultom E, Chuang SL, et al: Changing mortality and causes of death in infants 23-27 weeks’ gestational age. J Paediatr Child Health 35:255-259, 1999
Cartlidge PH, Stewart JH: Survival of very low birthweight and very preterm infants in a geographically
defined population. Acta Paediatr 86:105-110, 1997
Stevenson DK, Wright LL, Lemons JA, et al: Very low
birth weight outcomes of the National Institute of Child
Health and Human Development Neonatal Research
Network, January 1993 through December 1994. Am J
Obstet Gynecol 179:1632-1639, 1998
El-Metwally D, Vohr B, Tucker R: Survival and neonatal
morbidity at the limits of viability in the mid 1990s: 22 to
25 weeks. J Pediatr 137:616-622, 2000
73. Ahner R, Bikas D, Rabl M, et al: Ethical implications of
aggressive obstetric management at less than 28 weeks of
gestation. Acta Obstet Gynecol Scand 80:120-125, 2001
74. Teberg AJ, Hodgman JE, Barton L, et al: Nursery survival
for infants of birth weight 500-1500 grams during 19821995. J Perinatol 21:97-106, 2001
75. Hernandez JA, Hall DM, Goldson EJ, et al: Impact of
infants born at the threshold of viability on the neonatal
mortality rate in Colorado. J Perinatol 20:21-26, 2000
76. Wood B, Katz V, Bose C, et al: Survival and morbidity of
extremely premature infants based on obstetric assessment of gestational age. Obstet Gynecol 74:889-892,
1989
77. Macfarlane PI, Wood S, Bennett J: Non-viable delivery at
20-23 weeks gestation: observations and signs of life after
birth. Arch Dis Child Fetal Neonatal Ed 88:F199-202,
2003
78. Horbar JD: The Vermont-Oxford Trials Network: 1996
Annual Report. Burlington, Vermont, 1997
79. Bucher HU, Ochsner Y, Fauchere JC: Two years outcome of very pre-term and very low birthweight infants
in Switzerland. Swiss Med Wkly 133:93-99, 2003
80. Improved outcome into the 1990s for infants weighing
500-999 g at birth. The Victorian Infant Collaborative
Study Group. Arch Dis Child Fetal Neonatal Ed 77:F9194, 1997
81. Tyson JE, Younes N, Verter J, et al: Viability, morbidity,
and resource use among newborns of 501- to 800-g birth
weight. National Institute of Child Health and Human
Development Neonatal Research Network. Jama 276:
1645-1651, 1996
82. NSW Mothers and Babies Report 1997. Part 5: Neonatal
Intensive Care. Vol 2003, NICUS Data Collection, 2002
83. Darlow BA, Cust AE, Donoghue DA: Improved outcomes for very low birthweight infants: evidence from
New Zealand national population based data. Arch Dis
Child Fetal Neonatal Ed 88:F23-28, 2003
84. Piecuch RE, Leonard CH, Cooper BA, et al: Outcome of
infants born at 24-26 weeks’ gestation: II. Neurodevelopmental outcome. Obstet Gynecol 90:809-814, 1997
85. Rijken M, Stoelhorst SJ, Martens SE, et al: Mortality and
neurologic, mental and psychomotor development at 2
years in infants born less than 27 weeks’ gestation: The
Leiden follow-up project on prematurity. Pediatrics 112:
351-358, 2003