Ontogeny of Renal Sodium Transport
Michel Baum*† and Raymond Quigley*
One of the main functions of the adult kidney is to maintain a constant extracellular fluid balance.
The adult kidney does this, by and large, by filtering a massive quantity of fluid and reabsorbing the
solutes needed to maintain volume and electrolyte homeostasis, while leaving the waste products to
be excreted in the urine. One of the most precisely regulated functions of the adult kidney is to
maintain sodium balance. The challenge of the neonatal kidney is even greater. It must maintain a
positive salt balance for growth while the neonate is fed a diet that is very low in sodium. This review
focuses on how the neonatal kidney reabsorbs NaCl with a special emphasis on the differences
between the neonatal and adult kidney.
© 2004 Elsevier Inc. All rights reserved.
f the 150 L the adult kidney filters a day,
only ⬃1% is excreted in the urine. Thus,
one of the primary roles of the renal tubules is to
reabsorb most of the salt and water filtered by
the glomerulus. The problem is much more
complicated as the kidney has to maintain NaCl
balance in the face of a variable salt intake. If an
adult changes his diet from a moderate NaCl
intake to a diet rich in pepperoni pizzas the
kidney will excrete this salt load to maintain salt
balance. If NaCl output did not match NaCl
intake hypertension, edema and congestive
heart failure would be the result of this dietary
indiscretion. On the other hand, the kidney can
adapt to a low sodium intake or states of volume
depletion to excrete almost no sodium. This
balance of sodium intake to excretion maintains
a constant extracellular fluid balance.
Unlike the adult who has a variable salt intake, the neonate only drinks milk, a fluid that is
very low in sodium and chloride. While a major
task of the adult kidney is to maintain salt balance, this would be ill suited for a neonate that
must constantly be in positive NaCl balance in
order to grow. Thus, the neonatal kidney is challenged to maintain a positive salt balance in
spite of the fact that the dietary intake of salt is
extremely low. The difference in the neonatal
and adult kidney is exemplified by an experiment where neonatal and adult dogs were both
given an isotonic NaCl load equal to 10% of
their weight.1 While the adult dog excreted 50%
of the sodium load within 2 hours, the newborn
dog had excreted only 10% by that time.1
Sodium handling is quite different in extremely premature neonates. The challenge of
reabsorbing all of the filtered sodium is not met
in these neonates, let alone maintaining positive
O
sodium and chloride balance for growth. The
renal salt wasting is due to tubular immaturity,
which results in hyponatremia unless extra sodium is provided or unless the neonate is fluid
restricted.
How does the neonatal kidney maintain positive salt balance in spite of the fact that mother’s
milk is so low in sodium? The kidney of a term
infant only filters one twenty-fifth the volume of
fluid as that of the adult. The glomerular filtration rate is much lower than that of the adult
even if one corrects for the body surface area.
The low glomerular filtration rate makes the job
of NaCl reabsorption a lot easier because less salt
is delivered to the tubules. None-the-less the
renal tubules of the neonate must reabsorb almost all of the filtered salt and water. In this
short review, the mechanisms of renal salt reabsorption are discussed with an emphasis on the
differences between the neonatal and adult kidney. As a general rule of thumb, almost all transport is secondary to the sodium pump (Na⫹-K⫹ATPase) on the basolateral membrane. The
Na⫹-K⫹-ATPase transports 3 sodium ions out of
the cell in exchange for 2 potassium ions into
the cell. This results in a cell with sodium conFrom the Department of *Pediatrics; †Internal Medicine, The University of Texas Southwestern Medical Center, Dallas, TX.
This work was supported by National Institute of Diabetes and
Digestive and Kidney Disease Grant DK-41612 (to M. B.).
Address reprint requests to Michel Baum, MD, Professor of Pediatrics
and Internal Medicine, Sara M. and Charles E. Chair in Pediatric
Research, Department of Pediatrics, University of Texas Southwestern Medical Center, 5323 Harry Hines Blvd, Dallas, Texas 752359063; e-mail: Michel.Baum@UTSouthwestern.edu
© 2004 Elsevier Inc. All rights reserved.
0146-0005/04/2802-0002$30.00/0
doi:10.1053/j.semperi.2003.11.008
Seminars in Perinatology, Vol 28, No 2 (April), 2004: pp 91-96
91
92
Baum and Quigley
centration approximately one tenth that of the
blood and with a potential difference of -60 mV.
Most solute transport, either directly or indirectly, uses this huge electrochemical gradient as
the driving force for solute entry. Most solute
exit across the basolateral membrane is via passive diffusion. The transporters responsible for
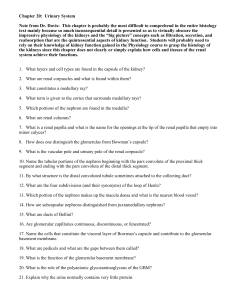
NaCl transport along the nephron are shown in
Figure 1.
Proximal Tubule Transport
The proximal tubule receives an ultrafiltrate of
plasma and reabsorbs all the filtered glucose and
amino acids, three quarters of the filtered bicarbonate, and two thirds of the filtered chloride.
There are several different mechanisms for the
reabsorption of NaCl by the proximal tubule.
The early proximal tubule preferentially reabsorbs glucose, amino acids, and bicarbonate
over chloride ions.2,3 This leaves the late proxi-
mal tubule luminal fluid without organic solutes
and with a very low concentration of bicarbonate. Sodium and chloride are essentially the only
solutes in the lumen of the distal half of the
proximal tubule.3
The proximal tubule is the hardest working
tubular segment, yet it does try to get as much
NaCl transport reabsorption as possible while
doing the minimum amount of work. The trick
that the proximal tubule uses is to separate the
reabsorption of solutes into the 2 phases described above. During the first phase where all
the glucose and amino acids are reabsorbed,
solute entry into the proximal tubule cell is via
sodium-dependent transporters. The reabsorption of the positively charged sodium along with
glucose or amino acids leaves a lumen negative
transepithelial potential difference. This negative potential provides a driving force for passive
chloride transport across the paracellular pathway. Thus for each glucose molecule reabsorbed
Figure 1. The nephron with the transporters responsible for sodium transport in the various nephron segments.
Ontogeny of Renal Sodium Transport
one also gets the reabsorption of a Na and Cl
molecule.
The vast majority of NaCl transport occurs in
the late proximal tubule where in the adult segment half of NaCl transport is active and transcellular and half is passive and paracellular.4-6
The active component of NaCl transport is mediated by the parallel operation of a Na⫹/H⫹
exchanger and a Cl⫺/OH⫺ exchanger.6-10 When
both of these transporters turn over, we have the
net reabsorption of a sodium and a chloride ion
and the secretion of a H⫹ and a OH- ion or
simply a water molecule. The Na⫹/H⫹ exchanger actually plays a role not only in sodium
reabsorption but it is the primary mechanism for
luminal proton secretion and thus the reabsorption of bicarbonate in the early proximal tubule.
As mentioned above the preferential reabsorption of organic solutes and bicarbonate in
the initial phase of proximal tubule reabsorption results in a luminal fluid that is essentially
composed of NaCl. This provides another way of
getting something for nothing. In the adult
proximal tubule, the chloride permeability of
the tight junction is very high.11 Because the
luminal chloride concentration is higher than
that in the peritubular plasma, the chloride concentration gradient provides a driving force for
passive chloride diffusion from the lumen across
the tight junction into the peritubular plasma.
The paracellular diffusion of the negatively
charged chloride results in a lumen positive potential difference, which provides the driving
force for passive paracellular NaCl transport.3
Well, how about the neonatal proximal tubule? There are several important differences in
transport between the adult and the neonate.
The overall theme, not only in the proximal
tubule, but down the entire nephron is that the
transporters responsible for solute absorption
are exactly the same, but the abundance is lower
in the neonatal tubule. This is true for the first
part of NaCl transport as well as active NaCl
transport where the apical Na⫹/H⫹ exchanger
and Cl⫺/OH⫺ exchangers are in lower abundance,5,12-14 as well as the basolateral Na⫹-K⫹ATPase and the basolateral chloride transporters.15,16 This is no tragedy because the amount of
fluid filtered and delivered to the tubules is
much less in the neonate. Studies have shown
that the fraction of the total fluid reabsorbed in
the proximal tubule is the same in the neonate
as the adult proximal tubule.
93
There are surprising differences in the fraction of NaCl transported across the paracellular
pathway in the neonatal proximal tubule compared to the adult proximal tubule. Although
half of chloride transport is passive and paracellular in the adult, because of the concentration
gradient and the high chloride permeability in
the adult segment, the neonatal proximal tubule
has no passive chloride transport.11 While a gradient develops favoring passive diffusion in the
neonatal tubule as it does in the adult, the neonatal proximal tubule is completely impermeable to chloride.11
The above issues raise the question as to what
causes the maturational changes in transporter
abundance and paracellular permeability. There
are a number of hormonal changes that occur
during the postnatal period. The neonate has
low serum levels of glucocorticoids and thyroid
hormone that increase to adult levels around the
time of weaning in most animals. As an example
of how the neonatal transporters change, the
authors discuss the apical Na⫹/H⫹ exchanger
because this is an important transporter and we
know the most about how this changes during
development. The newborn kidney has extremely low Na⫹/H⫹ antiporter activity compared to adults.6,10,14,17-20 If one adrenalectomizes a neonate to prevent the maturational
increase in glucocorticoids, the postnatal increase in Na⫹/H⫹ exchanger activity, mRNA
and brush border membrane protein abundance is markedly attenuated.21 On the other
hand, if one administers glucocorticoids to the
fetus and studies the neonate after delivery, the
rate and abundance of the Na⫹/H⫹ exchanger
is comparable to that of the adult tubule.14,19
Thus, glucocorticoids appear to be the main
factor causing the maturation of not only this
but most transporters along the nephron.
The factors causing the maturational changes
that occur in the paracellular pathway are quite
different. The tight junction is made up of proteins that shake hands with the neighboring cells
to cause the ion selective and restrictive permeability barrier. The changes in abundance in
tight junction proteins during postnatal maturation cause the change in the permeability barrier to chloride transport seen in the proximal
tubule. It appears that the maturational change
in thyroid hormone causes the change in the
permeability properties of the proximal tubule
to chloride ions.6 Animals made hypothyroid at
94
Baum and Quigley
birth never increase their proximal tubule paracellular permeability to chloride ions, whereas
neonates that are administered thyroid hormone have a paracellular chloride permeability
comparable to that of adults.
Finally, we must discuss water transport across
the proximal tubule. The glomerulus produces
an ultrafiltrate of plasma with an osmolality the
same as that of blood. By the end of the proximal tubule most of the glomerular ultrafiltrate
has been absorbed yet the osmolality of the tubular fluid has not changed. Thus, the proximal
tubule must be very permeable to water. The
adult tubule transports water across the apical
and basolateral membranes through water channels called aquaporins. The neonatal proximal
tubule is as permeable to water as the adult
segment, despite the fact that the abundance of
aquaporin water channels is very low. Water
transport in the neonatal tubule is via a nonaquaporin mediated mechanism, likely via other
transporters promiscuous for water, the paracellular pathway, or a more water permeable cell
membrane. Whereas the apical and basolateral
membrane are less permeable to water in the
neonatal segment, the cytoplasm of the neonate
allows water to pass with less restriction than the
adult segment.22-28 The postnatal increase in
aquaporin expression is also mediated by glucocorticoids.23
Thick Ascending Limb and Distal
Convoluted Tubule
Because the neonate drinks a hypotonic fluid,
the neonatal kidney must have a way of producing dilute urine. The neonate can actually dilute
urine to the same minimal osmolality as that of
an adult, 50 mOsm/kg water. To do this there
must be a nephron segments that reabsorb salt
but are impermeable to water. These segments
are the thick ascending limb and distal convoluted tubule that reabsorb 25% and 5% of the
filtered sodium, respectively.
The thick ascending limb reabsorbs sodium
via an electroneutral sodium-potassium-2 chloride cotransporter (NKCC2). This is the transporter that is inhibited by furosemide and bumetanide. This is also one the transporters that
has been found to be mutated in Bartter’s Syndrome along with the basolateral chloride channel and luminal potassium channel.29-33 This
transporter is electroneutral, but because of the
apical membrane potassium channel, potassium
diffuses back from the cell into the tubular lumen. This leaves the tubular lumen with a large
lumen positive potential difference. The tight
junction of the thick ascending limb is very permeable to cations and the positive potential difference provides a driving force for the paracellular absorption of calcium, magnesium,
potassium, and sodium. This is clinically significant since administration of furosemide will result in an increase in not only sodium excretion,
but also magnesium and calcium excretion. The
hypercalciuria that results from furosemide administration is the reason that neonates develop
nephrocalcinosis if treated for extended periods
of time with furosemide. On the other hand, the
fact that it inhibits calcium absorption makes it a
useful drug to treat hypercalcemia in a wellhydrated patient.
The distal convoluted tubule reabsorbs sodium chloride via an electroneutral NaCl cotransporter. This cotransporter results in the reabsorption of 5% of the filtered NaCl and is the
site of action of the thiazide diuretics. Gitelman’s syndrome, an autosomal recessive salt
wasting disease, is caused by a mutation of this
transporter.32-36 Patients with this disorder have
a hypokalemic alkalosis, as with Bartter’s syndrome, but patients with Gitelman’s syndrome
are less severely affected. They are distinguished
from Bartter’s Syndrome by presentation outside of the neonatal period, low calcium excretion rates, and profound hypomagnesemia. Thiazide diuretics result in an increase in calcium
reabsorption in this segment and are thus clinically useful as a diuretic in neonates to prevent
nephrocalcinosis. Although it is not completely
clear how thiazides increase calcium absorption,
one theory is that by decreasing NaCl absorption
they increase chloride entry across the basolateral membrane via passive diffusion resulting in
a more negative transcellular potential difference. This negative potential increases the driving force for calcium transport into the cell, the
rate-limiting step in calcium absorption.
All of the transporters in the thick ascending
limb and distal convoluted tubule, that have
been studied, are in lower abundance than that
of the mature segment.15,37-39 The maturation of
the Na⫹-K⫹-ATPase in the thick ascending limb
is mediated by perinatal increase in glucocorticoids.38 While all of the transporters are in lower
abundance, one of the primary function of this
Ontogeny of Renal Sodium Transport
segment is to reabsorb salt without water and
generate a dilute urine so that infants do not
develop hyponatremia when drinking mothers
milk; a function that these segments perform
adequately with the relatively small amount of
sodium delivered to them.
Collecting Duct
The collecting duct reabsorbs only 1% to 3% of
the filtered sodium but nonetheless plays a vital
role in sodium homeostasis because the final
modulation of sodium reabsorption is performed here. As is shown in Figure 1, the reabsorption of sodium is via a sodium channel in
principal cells in the collecting tubule. The reabsorption of sodium in this segment results in a
large lumen negative potential difference that
results in either the secretion of potassium, reabsorption of chloride through the paracellular
pathway, or the secretion of a proton. The driving force for sodium absorption is the basolateral Na⫹-K⫹-ATPase. All of the aforementioned
transporters in this segment are regulated by
aldosterone. This is why aldosterone deficiency
or damage to the collecting tubule from obstructive uropathy results in hyperkalemic metabolic
acidosis (type IV RTA), while hyperaldosteronism results in hypertension associated with hypokalemic metabolic alkalosis.
The sodium channel in this segment has been
designated ENaC. Its surface expression is increased in Liddle’s syndrome,40-42 which results
in hypertension associated with hypokalemic alkalosis, but low serum aldosterone levels. A defect in either the aldosterone receptor or the
sodium channel itself leads to pseudohypoaldosteronism. Neonates with the channel defect are
more severely affected than those with the aldosterone receptor mutation and have respiratory
distress as neonates, since the reabsorption of
perinatal pulmonary fluid is partially dependent
on the pulmonary ENaC function.43-47
The rate of sodium reabsorption in the immature collecting tubule is much less than that
of the adult segment.48-50 This is not caused by a
lower plasma concentration of aldosterone or a
paucity of aldosterone receptors in the neonatal
segment. There is, however, a paucity of sodium
channels in the neonatal collecting tubule and
the ones that are there have a lower probability
of being open to allow sodium passage into the
cell than that in the adult segment.49 In addition
95
the activity of the basolateral Na⫹-K⫹-ATPase is
also lower in the neonatal cortical collecting
tubule than in the adult segment.15,51
References
1. Goldsmith DI, Drukker A, Blaufox MD, et al: Hemodynamic and excretory response of the neonatal canine
kidney to acute volume expansion. Am J Physiol 237:
F392-F397, 1979
2. Liu FY, Cogan MG: Axial heterogeneity of bicarbonate,
chloride, and water transport in the rat proximal convoluted tubule. Effects of change in luminal flow rate and
of alkalemia. J Clin Invest 78:1547-1557, 1986
3. Rector FC Jr: Sodium, bicarbonate, and chloride absorption by the proximal tubule. Am J Physiol 244:F461-F471,
1983
4. Baum M, Berry CA: Evidence for neutral transcellular
NaCl transport and neutral basolateral chloride exit in
the rabbit convoluted tubule. J Clin Invest 74:205-211,
1984
5. Shah M, Quigley R, Baum M: Maturation of rabbit proximal straight tubule chloride/base exchange. Am J
Physiol 274:F883-F888, 1998
6. Shah M, Quigley R, Baum M: Maturation of proximal
straight tubule NaCl transport: Role of thyroid hormone. Am J Physiol Renal Physiol 278:F596-F602, 2000
7. Aronson PS: Ion exchangers mediating NaCl transport
in the renal proximal tubule. Cell Biochem Biophys
36:147-153, 2002
8. Aronson PS, Giebisch G: Mechanisms of chloride transport in the proximal tubule. Am J Physiol 273:F179-F192,
1997
9. Kurtz I, Nagami G, Yanagawa N, et al: Mechanism of
apical and basolateral Na(⫹)-independent Cl-/base exchange in the rabbit superficial proximal straight tubule.
J Clin Invest 94:173-183, 1994
10. Shah M, Quigley R, Baum M: Neonatal rabbit proximal
tubule basolateral membrane Na⫹/H⫹ antiporter and
Cl-/base exchange. Am J Physiol 276:R1792-R1797, 1999
11. Quigley R, Baum M: Developmental changes in rabbit
proximal straight tubule paracellular permeability. Am J
Physiol Renal Physiol 283:F525-F531, 2002
12. Baum M, Quigley R: Maturation of proximal tubular
acidification. Pediatr Nephrol 7:785-791, 1993
13. Baum M, Quigley R: Ontogeny of proximal tubule acidification [editorial]. Kidney Int 48:1697-1704, 1995
14. Beck JC, Lipkowitz MS, Abramson RG: Ontogeny of
Na/H antiporter activity in rabbit renal brush border
membrane vesicles. J Clin Invest 87:2067-2076, 1991
15. Schmidt U, Horster M: Na-K-activated ATPase: Activity
maturation in rabbit nephron segments dissected in
vitro. Am J Physiol 233:F55-F60, 1977
16. Schwartz GH, Evan AP: Development of solute transport
in rabbit proximal tubule. III. Na-K-ATPase activity. Am J
Physiol 246:F845-F852, 1984
17. Baum M: Neonatal rabbit juxtamedullary proximal convoluted tubule acidification. J Clin Invest 85:499-506,
1990
18. Baum M, Biemesderfer D, Gentry D: Ontogeny of rabbit
renal cortical NHE3 and NHE1: effect of glucocorticoids. Am J Physiol 268:F815-F820, 1995
96
Baum and Quigley
19. Baum M, Quigley R: Prenatal glucocorticoids stimulate
neonatal juxtamedullary proximal convoluted tubule
acidification. Am J Physiol 261:F746-F752, 1991
20. Shah M, Gupta N, Dwarakanath V, et al: Ontogeny of
Na⫹/H⫹ antiporter activity in rat proximal convoluted
tubules. Pediatr Res 48:206-210, 2000
21. Gupta N, Tarif SR, Seikaly M, et al: Role of glucocorticoids in the maturation of the rat renal Na⫹/H⫹ antiporter (NHE3). Kidney Int 60:173-181, 2001
22. Mulder J, Baum M, Quigley R: Diffusional water permeability (PDW) of adult and neonatal rabbit renal brush
border membrane vesicles. J Membr Biol 187:167-174,
2002
23. Mulder J, Haddad MN, Baum M, et al: Glucocorticoids
increase osmotic water permeability in neonatal proximal tubule brush border membrane. J Am Soc Nephrol
12:20A(abstr), 2001
24. Quigley R, Baum M: Developmental changes in rabbit
juxtamedullary proximal convoluted tubule water permeability. Am J Physiol 271:F871-F876, 1996
25. Quigley R, Baum M: Water transport in neonatal and
adult rabbit proximal tubules. Am J Physiol Renal
Physiol 283:F280-F285, 2002
26. Quigley R, Gupta N, Lisec A, et al: Maturational changes
in rabbit renal basolateral membrane vesicle osmotic
water permeability. J Membr Biol 174:53-58, 2000
27. Quigley R, Harkins EW, Baum M: Maturational changes
in rabbit brush border membrane vesicle (BBMV) osmotic water permeability (Pf). Pediatr Res 41:282A, 1997
28. Quigley R, Harkins EW, Thomas PJ, et al: Maturational
changes in rabbit renal brush border membrane vesicle
osmotic water permeability. J Membr Biol 164:177-185,
1998
29. Simon DB, Bindra RS, Mansfield TA, et al: Mutations in
the chloride channel gene, CLCNKB, cause Bartter’s
syndrome type III. Nat Genet 17:171-178, 1997
30. Simon DB, Karet FE, Hamdan JM, et al: Bartter’s syndrome, hypokalaemic alkalosis with hypercalciuria, is
caused by mutations in the Na-K-2Cl cotransporter
NKCC2. Nat Genet 13:183-188, 1996
31. Simon DB, Karet FE, Rodriguez-Soriano J, et al: Genetic
heterogeneity of Bartter’s syndrome revealed by mutations in the K⫹ channel, ROMK. Nat Genet 14:152-156,
1996
32. Simon DB, Lifton RP: Ion transporter mutations in
Gitelman’s and Bartter’s syndromes. Curr Opin Nephrol
Hypertens 7:43-47, 1998
33. Simon DB, Lifton RP: Mutations in Na(K)Cl transporters in Gitelman’s and Bartter’s syndromes. Curr Opin
Cell Biol 10:450-454, 1998
34. Cruz DN, Shaer AJ, Bia MJ, et al: Gitelman’s syndrome
revisited: An evaluation of symptoms and health- related
quality of life. Kidney Int 59:710-717, 2001
35. Simon DB, Lifton RP: Mutations in renal ion transporters cause Gitelman’s and Bartter’s syndromes of inherited hypokalemic alkalosis. Adv Nephrol Necker Hosp
27:343-359, 1997
36. Simon DB, Nelson-Williams C, Bia MJ, et al: Gitelman’s
variant of Bartter’s syndrome, inherited hypokalaemic
alkalosis, is caused by mutations in the thiazide-sensitive
Na-Cl cotransporter. Nat Genet 12:24-30, 1996
37. Bachmann S, Bostanjoglo M, Schmitt R, et al: Sodium
transport-related proteins in the mammalian distal
nephron-Distribution, ontogeny and functional aspects.
Anat Embryol (Berl) 200:447-468, 1999
38. Rane S, Aperia A: Ontogeny of Na-K-ATPase activity in
thick ascending limb and of concentrating capacity.
Am J Physiol 249:F723-F728, 1985
39. Schmitt R, Ellison DH, Farman N, et al: Developmental
expression of sodium entry pathways in rat nephron.
Am J Physiol 276:F367-F381, 1999
40. Bubien JK, Ismailov II, Berdiev BK, et al: Liddle’s disease: abnormal regulation of amiloride-sensitive Na⫹
channels by beta-subunit mutation. Am J Physiol 270:
C208-C213, 1996
41. Findling JW, Raff H, Hansson JH, et al: Liddle’s syndrome: prospective genetic screening and suppressed
aldosterone secretion in an extended kindred. J Clin
Endocrinol Metab 82:1071-1074, 1997
42. Schild L, Lu Y, Gautschi I, et al: Identification of a PY
motif in the epithelial Na channel subunits as a target
sequence for mutations causing channel activation
found in Liddle syndrome. EMBO J 15:2381-2387, 1996
43. Chang SS, Grunder S, Hanukoglu A, et al: Mutations in
subunits of the epithelial sodium channel cause salt
wasting with hyperkalaemic acidosis, pseudohypoaldosteronism type 1. Nat Genet 12:248-253, 1996
44. Fuller PJ, Rogerson FM: Pseudohypoaldosteronism: kidney, lungs and colon. Clin Endocrinol (Oxf) 56:571-572,
2002
45. Geller DS, Rodriguez-Soriano J, Vallo BA, et al: Mutations in the mineralocorticoid receptor gene cause autosomal dominant pseudohypoaldosteronism type I. Nat
Genet 19:279-281, 1998
46. Prince LS, Launspach JL, Geller DS, et al: Absence of
amiloride-sensitive sodium absorption in the airway of
an infant with pseudohypoaldosteronism. J Pediatr 135:
786-789, 1999
47. Rossier BC, Pradervand S, Schild L, et al: Epithelial
sodium channel and the control of sodium balance:
Interaction between genetic and environmental factors.
Annu Rev Physiol 64:877-897, 2002
48. Satlin LM: Postnatal maturation of potassium transport
in rabbit cortical collecting duct. Am J Physiol 266:F57F65, 1994
49. Satlin LM, Palmer LG: Apical Na⫹ conductance in maturing rabbit principal cell. Am J Physiol 270:F391-F397,
1996
50. Vehaskari VM: Ontogeny of cortical collecting duct sodium transport. Am J Physiol 267:F49-F54, 1994
51. Constantinescu AR, Lane JC, Mak J, et al: Na(⫹)-K(⫹)ATPase-mediated basolateral rubidium uptake in the
maturing rabbit cortical collecting duct. Am J Physiol
Renal Physiol 279:F1161-F1168, 2000