Promoting pulmonary maturity
advertisement

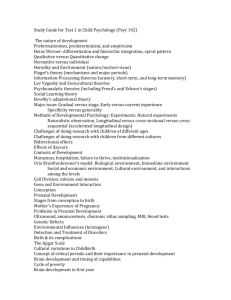
1 2 3 4 5 6 7 8 9 10 1 2 3 4 5 6 7 8 9 20 1 2 3 4 5 6 7 8 9 30 1 2 3 4 5 6 7 8 9 40 41 Promoting pulmonary maturity 1 Introduction 2 Benefits of prenatal corticosteroid administration 2.1 Respiratory distress syndrome 2.2 Other neonatal morbidity and mortality 3 Potential risks of prenatal corticosteroid administration 3.1 Risks to the mother 3.2 Risks to the baby 4 Prenatal corticosteroid administration in special situations 4.1 Hypertensive disease 4.2 Intra-uterine growth restriction 4.3 Diabetes mellitus 4.4 Rhesus iso-immunization 5 Other agents to promote pulmonary maturity 5.1 Ambroxol 5.2 Thyrotropin-releasing hormone 6 Conclusions 1 Introduction Respiratory distress syndrome is the most common complication of preterm birth, affecting over 50% of babies born before 32 weeks’ gestation. It remains a significant cause of death and severe morbidity in preterm infants. A number of agents can promote fetal lung maturation and thereby reduce the risk of respiratory distress syndrome in the newborn. Only three of these have been evaluated in controlled trials: corticosteroids, ambroxol, and thyrotropin-releasing hormone (TRH) administered in combination with corticosteroids. Of these, corticosteroids and TRH in combination with corticosteroids have been evaluated thoroughly, and only prenatal corticosteroids are of benefit. SOURCE: Murray Enkin, Marc J.N.C. Keirse, James Neilson, Caroline Crowther, Lelia Duley, Ellen Hodnett, and Justus Hofmeyr. A Guide to Effective Care in Pregnancy and Childbirth, 3rd ed. Oxford, UK: Oxford University Press, 2000. DOWNLOAD SOURCE: Maternity Wise™ website at www.maternitywise.org/prof/ © Oxford University Press 2000 1 2 3 4 5 6 7 8 9 10 1 2 3 4 5 6 7 8 9 20 1 2 3 4 5 6 7 8 9 30 1 2 3 4 5 6 7 8 9 40 41 2 Benefits of prenatal corticosteroid administration 2.1 Respiratory distress syndrome Prenatal administration of corticosteroids that pass through the placenta to the fetus results in a clinically important and statistically significant decrease in the risk of respiratory distress syndrome. Betamethasone (24 mg) and dexamethasone (24 mg) are both associated with an important and statistically significant reduction of respiratory distress syndrome. The risk reduction is approximately 40–60%. Hydrocortisone has been evaluated in only a few small trials, without sufficient power to demonstrate a statistically significant effect. Maximum benefit is achieved for babies delivered more than 24 hours and less than 7 days after commencement of the medication. The reductions in the incidence of respiratory distress seen for babies born outside of this optimum period do not achieve statistical significance in the trials conducted, although the trend suggests a benefit. No beneficial treatment effect has been demonstrated from the trials for babies born more than 7 days after the first course of prenatal steroids. Because of this, it has become widespread practice to administer prenatal corticosteroids at weekly intervals to women who remain undelivered and at risk of preterm birth. Whether or not prenatal steroids should be repeated if the woman remains undelivered and at risk of preterm birth 7 days or more after an initial course, is still unknown and is currently being evaluated by randomized trials (see also Section 3.2). Corticosteroid administration to infants born at less than 28 weeks’ gestation, produced similar reductions in the risk of respiratory distress to that observed for preterm babies as a whole, although the numbers available for analysis were not sufficient to demonstrate statistical significance. Respiratory distress is uncommon among babies born after 34 weeks’ gestation, so the beneficial effects will be less in absolute terms, but the relative reduction of risk is similar to that found at earlier gestational ages. Gender of the baby does not modify the effects of prenatal corticosteroid administration. 2.2 Other neonatal morbidity and mortality An important secondary benefit of corticosteroids has been a reduction in the duration and cost of neonatal hospital stay. The need for use of surfactant is reduced. Corticosteroids reduce the risk, not only of respiratory morbidity, but also of other serious forms of neonatal 1 2 3 4 5 6 7 8 9 10 1 2 3 4 5 6 7 8 9 20 1 2 3 4 5 6 7 8 9 30 1 2 3 4 5 6 7 8 9 40 41 morbidity. The risk of periventricular hemorrhage is less than half that seen without the use of corticosteroids. This effect is probably related to the reduced risk of respiratory distress, although it might also reflect an effect of corticosteroids on the periventricular vasculature. No statistically significant effects have been observed on the risk of necrotizing enterocolitis or of chronic lung disease. The marked reductions in risk of respiratory distress syndrome and periventricular hemorrhage are reflected in a substantial reduction in the risk of early neonatal mortality. As there is no concomitant increase in the risk of fetal death with corticosteroid use, this represents a decrease in overall perinatal mortality. 3 Potential risks of prenatal corticosteroid administration 3.1 Risks to the mother Instances of pulmonary edema have been reported in pregnant women receiving a combination of corticosteroids and labor-inhibiting drugs. It is difficult to estimate the magnitude of this risk, or to differentiate the separate effects of corticosteroids and the labor-inhibiting drugs. Infection is another potential risk of prenatal corticosteroid administration. Maternal infection is not increased overall, although infection is increased in women with rupture of the membranes for more than 24 hours prior to birth. Other pharmacological effects of corticosteroid administration in adults relate to long-term treatment, and they provide few grounds for concern when a single course of prenatal corticosteroids is used for a period of 24–48 hours to promote fetal maturation. 3.2 Risks to the baby The immunosuppressive effects of corticosteroid therapy could, in theory, result in an increased susceptibility to infection or to a delay in its recognition. This concern has received a great deal of attention, especially in pregnancies complicated by prelabor rupture of the membranes. Data from the trials show no evidence that corticosteroid therapy increases the risk of fetal or neonatal infection overall or in cases of preterm prelabor rupture of the membranes. A fetus may be exposed to corticosteroids throughout pregnancy if the mother is receiving long-term steroid therapy for ulcerative colitis, 1 2 3 4 5 6 7 8 9 10 1 2 3 4 5 6 7 8 9 20 1 2 3 4 5 6 7 8 9 30 1 2 3 4 5 6 7 8 9 40 41 asthma, rheumatoid arthritis, or other conditions. A review of the literature shows no striking excess over expectation for any adverse outcomes. The most reliable evidence about the long-term effects of a single course of prenatal corticosteroid therapy comes from follow-up of children whose mothers had been treated in the randomized trials. None of the studies indicate that prenatal corticosteroid therapy affects physical growth, lung growth, or development. Because of the reduced neonatal mortality rate in corticosteroid-treated babies, survivors from the corticosteroid groups had a lower mean gestational age at birth than survivors from the control group. Despite this, the available evidence suggests that prenatal corticosteroids may protect against the long-term neurological sequelae of hemiparesis, diplegia, and quadriplegia. This is plausible in the light of the complications that sometimes accompany both respiratory distress and its treatment. No controlled data are available on the risk of a repeat course of prenatal corticosteroids on the baby, although poorly controlled data suggest a reduction in birthweight. Animal studies have suggested other concerns, such as an effect on the fetal adrenals, and prompt caution against repeated use of prenatal corticosteroids until the results of trials are available. 4 Prenatal corticosteroid administration in special situations Elective preterm delivery differs from spontaneous preterm birth in at least four main ways. First, the timing of elective preterm delivery can be controlled, thus securing the delay required to gain maximum benefit from corticosteroid administration. Second, cesarean section, which predisposes to respiratory distress, is a common route of delivery in this group of babies. Third, elective preterm birth usually takes place somewhat later in gestation than spontaneous preterm birth, so that the absolute risk of respiratory distress is usually lower. Finally, elective preterm birth is often undertaken for conditions such as diabetes, in which corticosteroid administration may have unwanted effects. 4.1 Hypertensive disease Hypertensive disorders in pregnancy constitute one of the major indications for elective preterm birth. The initial concern about the use of steroids in women with pre-eclampsia was based on the statistically 1 2 3 4 5 6 7 8 9 10 1 2 3 4 5 6 7 8 9 20 1 2 3 4 5 6 7 8 9 30 1 2 3 4 5 6 7 8 9 40 41 significantly increased risk of fetal death associated with corticosteroid use in the 90 women with pre-eclampsia studied in the first reported trial. This early finding was not based on a plausible hypothesis, and came from a subgroup analysis. All 12 deaths occurred in women with proteinuria of more than 2 g per day for more than 14 days, a severity of disease that was not found in any of the placebo-treated women. There were no fetal deaths of babies of a similar number of hypertensive women in the three other trials from which data are available to address this issue. A consistent adverse effect of corticosteroids would have resulted in an increased incidence of stillbirth overall, but this did not occur. Thus, there is no good reason to deny women with preeclampsia the benefits of steroid therapy. Even in the absence of any adverse effect of corticosteroids in women with pre-eclampsia, the clinician may be faced with the possible risks of postponing delivery for the few hours required to achieve a useful effect of corticosteroid administration. In some cases this delay may constitute an unacceptably high risk of complications, such as eclampsia or cerebral hemorrhage in the mother. Delivery should not be delayed at the expense of maternal health, but even an incomplete course of steroids may help the baby. 4.2 Intra-uterine growth restriction Intra-uterine growth restriction, like hypertensive disease in pregnancy, is a common indication for elective preterm birth. Moreover, the two conditions often co-exist. The lungs of fetuses with growth restriction in the absence of maternal hypertension may have accelerated maturation, but there might still be benefit from corticosteroid administration. A potential disadvantage of prenatal corticosteroid therapy with intra-uterine growth restriction is the risk of neonatal hypoglycemia, which is an important complication in growth restricted infants. Although one trial reported more cases of neonatal hypoglycemia among corticosteroid-treated babies compared with controls, without information from other trials it is difficult to know whether this is anything more than a chance difference. 4.3 Diabetes mellitus Maternal diabetes mellitus may predispose to the development of respiratory distress syndrome. The results of the randomized trials do not clarify whether or not the use of corticosteroids is of benefit for diabetic women who deliver preterm, as only 35 such women were included in 1 2 3 4 5 6 7 8 9 10 1 2 3 4 5 6 7 8 9 20 1 2 3 4 5 6 7 8 9 30 1 2 3 4 5 6 7 8 9 40 41 the trials. Insufficient data are available to allow an evidence based recommendation. While the efficacy of prenatal corticosteroids to women with pregnancies complicated by diabetes mellitus is unknown, the potential side-effects should be a source of concern. Fetal hyperinsulinism may or may not cause cortisol resistance in the fetal lung. Administration of corticosteroids causes insulin resistance in the diabetic. Loss of diabetic control is to be expected with the doses of corticosteroids administered to promote fetal pulmonary maturation. Therefore, prenatal corticosteroid therapy in the diabetic woman would require exceptionally close supervision, possibly with continuous intravenous insulin and frequent blood glucose estimation. Failure to maintain control of the mother’s diabetes may result either in ketoacidosis, which carries a high perinatal mortality rate, or in a state of fetal hyperinsulinism, which may increase the likelihood of failure to respond to corticosteroid therapy. Corticosteroid administration, if used at all in diabetic women, should be used with great caution, as it is not certain that it will do more good than harm. 4.4 Rhesus iso-immunization Elective preterm delivery plays an important role in the management of rhesus iso-immunization. Unlike other conditions associated with chronic intra-uterine stress, rhesus disease is not thought to provoke an acceleration of pulmonary maturation. While there is a trend towards a reduction in perinatal mortality and in the incidence of respiratory distress syndrome in steroid-treated infants compared with controls, the numbers reported in the trials are too small to provide any secure estimates of the likely effects. However, there are no specific contra-indications to the administration of corticosteroids in women with rhesus iso-immunization. 5 Other agents to promote pulmonary maturity 5.1 Ambroxol Treatment with prenatal ambroxol compared with placebo shows a tendency towards reducing the risk of respiratory distress syndrome, but the results are not statistically significant. Direct comparisons of ambroxol with corticosteroids show no clear differential effect, although there were methodological weaknesses in the trials that examined this. The main disadvantage with ambroxol is the 5-day period 1 2 3 4 5 6 7 8 9 10 1 2 3 4 5 6 7 8 9 20 1 2 3 4 5 6 7 8 9 30 1 2 3 4 5 6 7 8 9 40 41 required to complete therapy. Because the evidence in favor of prenatal corticosteroids in anticipated preterm birth is so strong, they remain the prophylactic strategy of choice. 5.2 Thyrotropin-releasing hormone Prenatal administration of thyrotropin-releasing hormone (TRH) in addition to corticosteroids, prior to very preterm birth, does not reduce the risks of respiratory distress syndrome or of chronic lung disease, and is associated with an increased risk of maternal side-effects of nausea, vomiting, light headedness, and elevation of pulse and blood pressure. Systematic review of the randomized trials available shows not only no benefit but an increase in the risk of respiratory distress syndrome, need for ventilation, and death or need for oxygen by day 28 after birth, in babies exposed to prenatal TRH who deliver 10 or more days later. In view of this, prenatal TRH cannot be recommended. 6 Conclusions Prenatal treatment with 24 mg betamethasone, or 24 mg dexamethasone, for lung maturation, is associated with a significant reduction in the risk of respiratory distress syndrome in preterm infants. This reduction is independent of gender, and applies to babies born at all gestational ages at which respiratory distress syndrome may occur. It is accompanied by reductions in the risk of periventricular hemorrhage, lower neonatal mortality rate, and in a reduced cost and duration of neonatal care. These benefits are achieved without any detectable increase in the risk of maternal, fetal, or neonatal infection. Although maternal infection is increased in women with rupture of membranes for more than 24 hours prior to birth, prenatal corticosteroid administration does not increase the risk of stillbirth. Every effort should be made to treat women with corticosteroids prior to preterm birth, either as a result of preterm labor or planned elective preterm birth. The only possible exception is for women with diabetes. Treatment should commence at presentation in women with any symptoms or signs that suggest the onset of preterm labor or indicate a potential need for elective preterm birth in the near future. Treatment should not be withheld because birth appears imminent. There are no controlled data to recommend or refute the widespread 1 2 3 4 5 6 7 8 9 10 1 2 3 4 5 6 7 8 9 20 1 2 3 4 5 6 7 8 9 30 1 2 3 4 5 6 7 8 9 40 41 use of repeat doses of prenatal corticosteroids for women who remain at risk of preterm birth but undelivered after an initial course. Until the results from the trials currently in progress are available, multiple doses of prenatal corticosteroids should be avoided. TRH should not be used for the promotion of pulmonary maturation. Sources Effective care in pregnancy and childbirth Crowley, P., Promoting pulmonary maturity. Cochrane Library Crowley, P., Prophylactic corticosteroids for preterm delivery. Crowther, C.A., Alfirevic, Z. and Haslam, R. Prenatal thyrotropinreleasing hormone (TRH) for preterm birth. Pre-Cochrane reviews Crowley, P. Ambroxol vs placebo prior to preterm delivery. Review no. 03276. Ambroxol vs betamethasone prior to preterm delivery. Review no. 03852. Ambroxol vs intralipid prior to preterm delivery. Review no. 03853. Corticosteroids + induction of labour after PROM preterm. Review no. 06871. Corticosteroids prior to preterm delivery. Review no. 02955.