Increased Peripheral Chemoreceptor Activity
may be Critical in Destabilizing Breathing
in Neonates
Abdulrahman Al-Matary, Ibrahim Kutbi, Mansour Qurashi,
Mohammed Khalil, Ruben Alvaro, Kim Kwiatkowski, Don Cates,
and Henrique Rigatto
Periodic breathing and apnea are common in neonates, yet the physiological mechanisms involved are
not clear. A low arterial PO2 might magnify peripheral chemoreceptor contribution to breathing, with
its baseline variability inducing major changes in ventilation, leading to instability of the respiratory
control system. We hypothesized that neonates: (1) would depend much more on the peripheral
chemoreceptor contribution to breathing than adult subjects and (2) their baseline arterial PO2 would
sit on the steep portion of the ventilation/arterial PO2 relationship on the adult nomogram, making
breathing prone to oscillate. We analyzed data from previous polygraphic recordings in four groups
of subjects: small preterm infants [SPI; postconceptional age (PCA) 33 ⴞ 2 weeks; n ⴝ 40], large
preterm infants (LPI; PCA 36 ⴞ 2 weeks; n ⴝ 34), term infants (TI; PCA 42 ⴞ 1 week; n ⴝ 24), and
adult subjects (AS; weight 63 ⴞ 2 kg; age 29 ⴞ 3 years, n ⴝ 16). Peripheral chemoreceptor activity was
measured by: (1) the immediate decrease in ventilation and (2) apnea time during brief inhalation of
100% O2 (about 1 minute). We found that: (1) the immediate decrease in ventilation with 100% O2
was more pronounced in infants than in adult subjects (38 ⴞ 2 versus 6 ⴞ 5%), and in infants
breathing periodically versus those breathing continuously; (2) the apnea time during 100% O2 was
also significantly longer in periodic breathing infants; and (3) the TcPO2 was much lower in infants
than in adult subjects (65 ⴞ 1 versus 93 ⴞ 1 Torr), and also lower in periodic versus continuously
breathing infants. It was located significantly to the left of values for the adult subject, on the
ventilation/arterial PO2 diagram. The data suggest that: (1) a substantial portion of baseline breathing activity early in life is maintained by increased peripheral chemoreceptor activity; and (2)
neonates breathe irregularly with apneas due to the position of their arterial PO2 values on the
ventilation/arterial PO2 diagram, in which a change in PO2 produces a more significant change in
ventilation than that observed later in life.
© 2004 Elsevier Inc. All rights reserved.
eriodic breathing and apnea are common
in neonates, particularly in preterm infants,
but they are rare or absent in older children and
adult subjects.1-15 Despite many efforts in the
past to understand the physiologic mechanisms
responsible for this respiratory pattern, we still
P
From the Department of Pediatrics, Physiology, and Reproductive
Medicine University of Manitoba, Winnipeg, MB Canada.
Supported in part by the Canadian Institutes of Health Research, the
Winnipeg Rh Institute Foundation, Inc., and the Children’s Hospital of Manitoba.
Address reprint requests to Henrique Rigatto, MD, WR-125, Women’s Hospital, 735 Notre Dame Avenue, Winnipeg, MB, R3E 0L8,
Canada e-mail: hrigatto@cc.umanitoba.ca
© 2004 Elsevier Inc. All rights reserved.
0146-0005/04/2804-0000$30.00/0
doi:10.1053/j.semperi.2004.08.003
264
do not know why some neonates breathe more
periodically than others.10-12,16 In previous studies, we observed that infants breathing periodically hypoventilated, were hypoxic, and had increased peripheral chemoreceptor activity when
compared with infants breathing continuously.
We were not able at the time to adjust for the
impact of gestational and postnatal age, nor
were we able to integrate these data into a mechanistic hypothesis.11,12
Since these previous publications, new developments have occurred in the field of respiratory control, particularly regarding the importance of central versus peripheral chemoreceptor activity to maintain baseline breathing,
and the crucial role of the PCO2 apneic threshold in inducing apnea.9,15,17,18 We hypothesized
Seminars in Perinatology, Vol 28, No 4 (August), 2004: pp 264-272
Increased Peripheral Chemoreceptor Activity
that the degree to which maintenance of breathing was dependent on peripheral chemoreceptor activity might be a major destabilizing factor
leading to apnea in term and preterm infants. If
this were true, we should observe greater peripheral chemoreceptor activity early versus late in
life, and in periodic breathers versus continuous
breathers. Moreover, if peripheral chemoreceptor dependence was related to arterial hypoxemia, we should observe a leftward shift of the
minute ventilation/transcutaneous PO2 (V̇E/
TcPO2) relationship in infants versus adult subjects, and in periodic versus continuous breathers.19,20
We designed this study to examine respiratory
pattern and ventilation in neonates of distinct
gestational and postconceptional ages and in
adult subjects, in parallel with measurements of
transcutaneous gases and peripheral chemoreceptor activity. In addition, these measurements
were also made in neonates with and without
periodic breathing.
Materials and Methods
Subjects
We analyzed data from previous polygraphic recordings in 114 subjects: 98 neonates and 16
adults. We excluded tracings lacking recording
of key variables or showing poor quality signals
on the polygraphic recording. The subjects were
growing preterm infants, normal term infants,
and healthy adult subjects. The original studies
were approved by the Faculty Committee for the
Use of Human Subjects in Research. Informed
consent was obtained from at least one of the
parents of the neonates and from each adult
subject. Neonates were further classified into
three groups: small preterm infants [SPI, birth
weight (BW) ⬍ 1500 g], large preterm infants
(LPI, BW ⱖ 1500), and term infants (TI). In
each of these subgroups, half of the infants
breathed predominantly periodic (⬎68% of
sleep time) and half breathed predominantly
continuous (⬎95%). Within each age/birth
weight stratum, periodic breathers were
matched 1:1 with continuous breathers. The
subjects were not on any medication at the time
of the study and were breathing room air.
265
Methods
Our system to measure breathing pattern and
ventilation has been described.3,7,21-23 Briefly,
breathing was measured using a nosepiece and a
flow-through system. The screen flowmeter was
linear up to 6 L 䡠 min⫺1. The resistance of the
system was low (0.1 cm H2O 䡠 L⫺1 䡠 min⫺1). The
frequency response of the system was linear, varying less than 5% from 18 to 120 cycles 䡠 min⫺1
with volumes of 5 to 30 mL. The infants
breathed through nostril adaptors and added
(expiration) or subtracted (inspiration) flow
from the background flow. The flow signal was
electronically integrated to give volume. Breathto-breath alveolar PCO2 (PACO2) and PO2
(PAO2) were measured using Beckman analyzers
(LB-2 and OM11; Beckman Instruments Co.,
Fullerton, CA). The 95% rise time of the analyzers was 0.16 and 0.18 seconds for CO2 and O2,
respectively. Alveolar gases are usually part of
our polygraphic monitoring, and in this study,
they were used primarily to monitor changes in
inhaled O2 during 100% O2. Oxygen saturation
(HbO2) was monitored with a Nellcor Pulse
Oximeter (model N-100C; Nellcor, Hayward,
CA) and used as an index of infant well being.
Transcutaneous O2 (TcPO2) and transcutaneous CO2 (TcPCO2) were measured with a model
TCM 3 model (Radiometer, Copenhagen, Denmark). The electroencephalogram (EEG) was
recorded with electrodes placed in the C4/A1
positions. The electrooculogram (EOG) was recorded from the upper outer canthus of the left
eye and the lower outer canthus of the right eye
and referred to the right ear lobe. Respiratory
efforts were determined using chest and abdominal displacements, which were measured using
mercury strain gauges.21 These strain gauges
were placed at the level of the 4th intercostal
space and just above the umbilicus. Heart rate
was measured using conventional leads. All signals were recorded on a Nihon Kohden 21-channel recorder (Model 4221; Nihon, Kohden, Tokyo, Japan) and were also stored in a computer
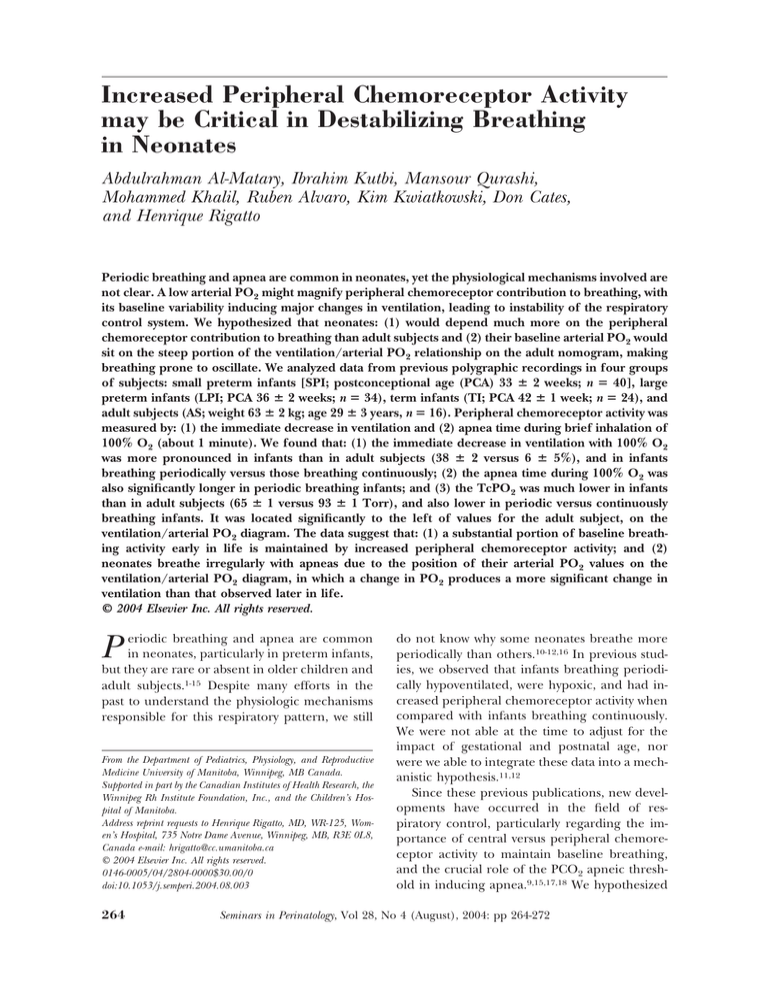
for further analysis. A representative tracing of
pertinent variables in infants is shown in Fig 1.
Sleep states were classified as quiet, REM,
transitional, and indeterminate. Quiet sleep was
defined by the absence of rapid eye movement
coupled with, in preterm infants, discontinuous
EEG, or, in term infants, with “trace alter-
266
Al-Matary et al
logic stage comparable to quiet sleep in preterm
infants.26
Experimental Procedures
Figure 1. Representative tracing of pertinent variables in a preterm infant breathing periodically and
in a preterm infant breathing continuously. Note the
significant prolongation of apnea in response to
100% O2 in the infant breathing periodically, whereas
the infant breathing continuously showed only a brief
decrease in frequency and in tidal volume.
nant.”3,6,22,24,25 REM sleep was defined by the
presence of rapid eye movements on the EOG
and continuous, irregular, low-voltage on the
EEG. Transitional states were short epochs lasting 1 to 3 minutes, which were usually observed
during the transition from quiet to REM or vice
versa. Indeterminate sleep was defined as that
which could not be described by other definitions. All ventilatory measurements were made
during quiet sleep, including the response to
100% O2.
Apneas were classified as central or obstructive. Central apneas were those in which airflow
and respiratory efforts (chest and abdominal displacement) were absent. Obstructive apneas
were those in which absent airflow was associated with some respiratory efforts. This obstructive group therefore includes apneas traditionally classified as purely obstructive and mixed.7,23
Adults were studied in a fully equipped sleep
laboratory. The method used was similar to that
of infants, consisting of a face mask connected to
a flow transducer. The flow signal was electrically integrated to give volume. EEG (C4-A1 and
C3-A2) and EOG were recorded from surface
electrodes. Breath-to-breath PAO2 and PACO2
were measured at the nose with a CO2 analyzer
(Dole 223; Puritan-Bennett Corp, Wilmington,
MA). All variables were continuously recorded at
10 mm/s using a 15-channel polygraph (Model
78; Grass Instruments Co, Quincy, MA). All measurements were made in stage 2 sleep, a physio-
Infants were studied on the Ohio Neonatal Intensive Care Unit (Ohio Medical Instrument,
Madison, WI) in a neutral thermal environment
with skin abdominal temperature at 36.5 ⫾
0.03°C. After appropriate placement of the various electrodes and nosepiece, we waited for the
infant to fall asleep. When the infant did not
settle, a feeding was offered. If infants woke
during the study, they were fed and the study was
continued. Once in quiet sleep and breathing
21% O2, the infants were exposed to 100% O2
for about 1 minute. Recording was long enough
to allow for a good representation of breathing
pattern. At least one epoch of quiet and REM
sleep were always observed. Adults slept overnight in the sleep laboratory and polygraphic
tracings were obtained. Administration of 100%
O2 was given when the subjects were breathing
quietly in stage 2 sleep.
Data Collection and Analysis
Respiratory minute ventilation (V̇E), frequency
(f), tidal volume (VT), PAO2, PACO2, TcPO2,
TcPCO2, HbO2 saturation (HbO2), heart rate
(HR), EEG, EOG, chest and abdominal displacements, length and type of apneas were measured
in all subjects. Apneas were defined as pauses
equal to or greater than 3 seconds in infants,
and equal or greater than 5 seconds in adults, as
to avoid calling a prolonged expiration apnea.
Peripheral chemoreceptor activity was assessed
by the decrease in ventilation and by the apnea
time during the brief inhalation of 100% O2.
The data were measured by hand from the
polygraphic tracings and transferred to a computer for analysis. To test the significance of
differences between continuous variables, we
used two-tailed one-way analysis of variance.
Tukey’s Honest Significant Difference test was
used for post hoc tests. Values are expressed as
mean ⫾ SEM. A probability value ⱕ0.05 was
considered significant.
Increased Peripheral Chemoreceptor Activity
267
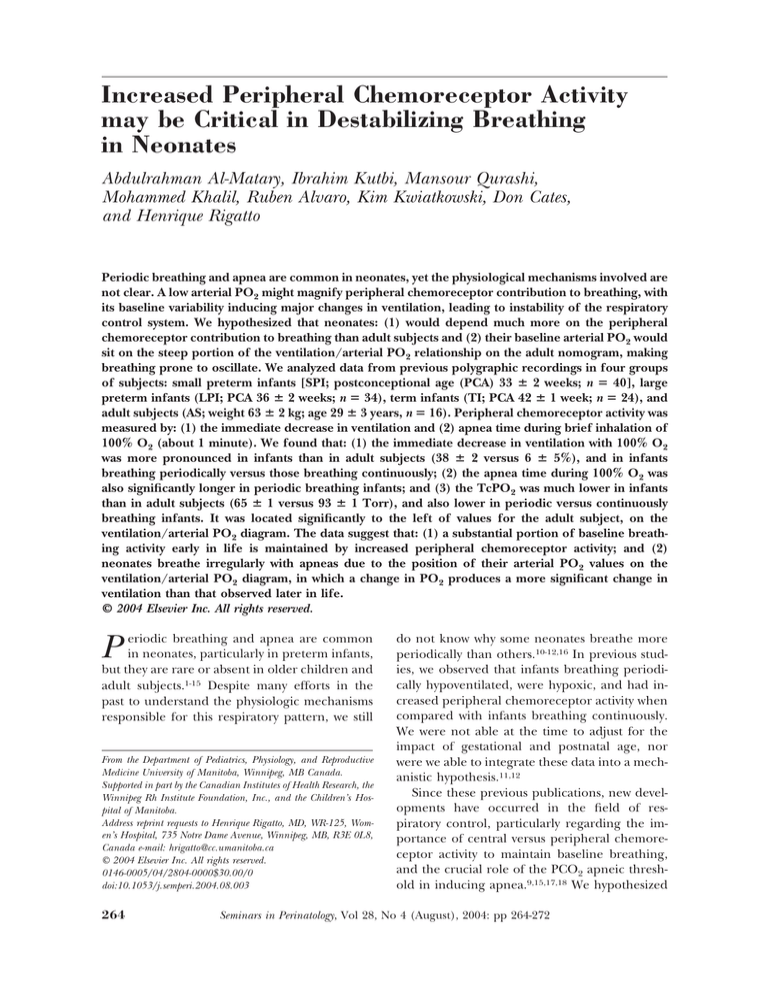
Figure 2. Minute ventilation and its components, frequency and tidal volume in
the various groups. Note that
minute ventilation per unit
body weight gradually decreased from the small preterm infant to the adult
subject; this was related primarily to a decrease in frequency, tidal volume increasing with postnatal age. There
was a trend for minute ventilation values for periodic
breathing infants to be lower
than those for continuously
breathing infants, also due to
a decrease in frequency. Values are expressed as mean ⫾
SEM. *, P ⱕ 0.05 in relation
to adult subjects.
Results
General Observations
We were able to examine the polygraphic recordings of four groups of subjects: (1) small
preterm infants [SPI, BW 1.2 ⫾ 0.04 kg (mean ⫾
SEM); gestational age (GA) 29 ⫾ 0.3 week; postnatal age (PNA) 28 ⫾ 3 days; postconceptional
age (PCA) 33 ⫾ 2 weeks; n ⫽ 40]; (2) large
preterm infants [LPI, BW 2.0 ⫾ 0.06 kg; GA
33 ⫾ 0.3 week; PNA 23 ⫾ 3 days; PCA 36 ⫾ 2
weeks, n ⫽ 34]; (3) term infants [TI, BW 3.4 ⫾
0.1 kg, GA 39 ⫾ 0.2 week, PNA 20 ⫾ 4 days; PCA
42 ⫾ 1 week, n ⫽ 24]; and (4) adult subjects [AS,
weight 63 ⫾ 3 kg, 29 ⫾ 3 years, n ⫽ 16]. The
percentage of periodic breathing was 68% in
infants breathing periodically and 5% in infants
breathing continuously. The average duration of
the study was 2.2 ⫾ 0.2 hour (range 1.5 to 3.2
hours) in neonates and 4.2 ⫾ 0.5 hour in adult
subjects.
Ventilatory Measurements
Minute ventilation per unit body weight decreased significantly from early life to adulthood
(Fig 2). This decrease was mediated primarily by
a decrease in f, since VT actually increased to
adulthood. In newborn infants VE was lower in
the periodic group than in the continuously
breathing group, although significance was
present only for small preterm infants. This
change in ventilation related primarily to a
greater decrease in f in infants breathing periodically.
Transcutaneous PO2 and PCO2
TcPO2 and TcPCO2 increased significantly from
small preterm to term infants, and increased
further to adult subjects (Fig 3). The TcPO2 was
much lower in infants than in adult subjects
(65 ⫾ 1 versus 93 ⫾ 1 Torr), and also lower in
periodic breathing infants than those breathing
continuously (54 ⫾ 2 versus 70 ⫾ 2 Torr in SPI;
57 ⫾ 1 versus 73 ⫾ 3 Torr in LPI; and 63 ⫾ 2
versus 74 ⫾ 2 Torr in TI, P ⬍ 0.001). Values for
TcPCO2 were lower in the continuously breathing than in the periodic breathing groups. When
the TcPO2 was plotted on the V̇E/TcPO2 regression curve, values for neonates were located to
the left of those for adult subjects, and the periodic breathing group was uniformly located to
the left of the continuous breathing group, in-
268
Al-Matary et al
Figure 3. Transcutaneous
gases according to various
postnatal ages. Note that
both TcPO2 and TcPCO2 increased from small preterm
infants to adult subjects. Note
also that periodic breathing
infants had a baseline TcPCO2
higher than infants breathing continuously, suggesting
that they are hypoventilating
as a group. Values are expressed as mean ⫾ SEM. *,
P ⱕ 0.05 in relation to adult
subjects. †, P ⱕ 0.05 in relation to continuous breathing
infants.
dicating an increase contribution of hypoxia to
ventilatory drive in the periodic group (Fig 4).
Peripheral Chemoreceptor Activity
Corresponding to the significantly lower TcPO2
early in life, there was a pronounced increase in
Figure 4. TcPO2 for periodic
and continuously breathing
infants plotted on the traditional ventilation/TcPO2 diagram for adult subjects. Note
that values for infants are significantly to the left of those
for adult subjects. Similarly,
values for periodic breathing
infants are to the left of those
for infants breathing continuously, suggesting a much
greater change in ventilation
per unit change in TcPO2.
This likely makes the respiratory control system prone to
oscillation. Values are expressed as mean ⫾ SEM. *,
P ⱕ 0.05 compared with adult
subjects; †, P ⱕ 0.05 in relation
to continuously breathing infants.
peripheral chemoreceptor activity at this age, as
reflected by a greater percent decrease in ventilation with inhalation of 100% O2 in neonates
compared with adult subjects (38 ⫾ 2 versus 6 ⫾
5%; Fig 5). The decrease in the various groups
was 45 ⫾ 3% (SPI), 35 ⫾ 3% (LPI), 30 ⫾ 5%
(TI), and 6 ⫾ 4% (AS), being more pronounced
Increased Peripheral Chemoreceptor Activity
269
Figure 5. Peripheral chemoreceptor activity, measured as
a percent decrease in ventilation, at various postnatal ages.
Note that the percent decrease in ventilation with
100% O2 gradually diminishes toward adulthood.
Note also that infants breathing periodically have a more
pronounced decrease in ventilation than those breathing
continuously. Values are expressed as mean ⫾ SEM. *,
P ⱕ 0.05 compared with
adult subjects; †, P ⱕ 0.05
compared with continuously
breathing infants.
in periodic than in continuously breathing infants(53 ⫾ 5 versus 38 ⫾ 5% in SPI; 41 ⫾ 5
versus 31 ⫾ 5% in LPI; and 45 ⫾ 5 versus 17 ⫾
6% in TI, P ⬍ 0.002). An additional index of this
more pronounced peripheral chemoreceptor
activity was reflected by the more prolonged
apnea time with O2 inhalation in all three
groups of neonates compared with adult subjects (Fig 6). These apneas were all central in
term neonates and were 24% mixed in preterm
infants. Only two adults had a brief apnea (⬍10
seconds). The periodic group showed a longer
apnea with inhalation of 100% O2 than the continuously breathing group at all ages.
Discussion
We measured peripheral chemoreceptor activity
in four groups of subjects, from small preterm
infants to adulthood, to improve our knowledge
Figure 6. Apnea time during
O2 administration in the various groups. Note that the apnea time decreases gradually
with increasing postnatal ages,
being short and rare in adult
subjects. Infants breathing periodically had significantly
longer apnea time than infants breathing continuously
during 100% O2, suggesting
more active peripheral chemoreceptors. Values are expressed as mean ⫾ SEM. *,
P ⱕ 0.05 in relation to adult
subjects; †, P ⱕ 0.05 in relation
to infants breathing continuously.
270
Al-Matary et al
of the mechanisms responsible for the unstable
breathing of newborn infants. We found that (1)
peripheral chemoreceptor activity was significantly increased in early life versus adulthood
and in infants breathing periodically versus
those breathing continuously; (2) the TcPO2
values of neonates were significantly lower than
and located to the left of those in adult subjects
on the V̇E/TcPO2 nomogram; similarly, values
for infants breathing periodically were to the left
of those breathing continuously; and (3) apneas
were more prolonged and more frequent in neonates than in adult subjects. The findings are
supportive of the hypothesis that the drive to
breathe early in life is dependent on increased
peripheral chemoreceptor activity, and that this
heightened peripheral chemoreceptor activity
may play a role in disturbing the respiratory
control system, leading to periodic breathing
and apnea.
Although we previously found that preterm
infants breathing periodically had lower arterial
PO2 than those breathing continuously, we did
not explore the possible role of low PO2 in
destabilizing breathing.10,11 The present study of
newborn infants and adult subjects provides
some interesting clues to potential mechanisms.
Today, it is well accepted that respiratory periodicity generated by low arterial O2 relates to a
decrease in arterial PCO2 below the apneic
threshold (ie, the PCO2 level below which
breathing ceases).9,15,17,18,27,28 This scenario was
clearly present in the present study, in which
infants breathing periodically manifested lower
TcPO2 values. We previously showed that neonates have a baseline PACO2 which is only 1.3
Torr above the apneic threshold,9 and this difference may become even smaller with a decrease in metabolism associated with low PO2.29
In contrast, adults have a difference of about 4
Torr between baseline and threshold Pco2, making it more difficult for PCO2 to dive below
threshold and destabilize breathing.15,18 Thus,
small decreases in PCO2, such as changes in
sleep state or stretching, can easily result in apnea.10,30 The low TcPO2 levels early in life also
lead to increased peripheral chemoreceptor activity and more instability of breathing, since
minor changes in arterial PO2 would greatly alter baseline ventilation. Therefore, this low arterial PO2 early in life represents a major handicap
for preterm infants.
There are a few new findings in the present
study worth emphasizing. First, methodical and
comprehensive studies of changes in ventilation
at different gestational and postconceptional
ages, including adult subjects, are limited.31 Second, an analysis of the differences in peripheral
chemoreceptor activity, particularly at different
postconceptional ages, has not been done, although reports on the overall responsiveness of
neonates and adults to high O2 has been documented previously.2,8,10-12,16,30,32 Finally, the pronounced shift to the left of the TcPO2 values of
infants breathing periodically versus infants
breathing continuously, on the V̇E/TcPO2 plot,
is novel and supports the idea that low O2 and its
effect on the peripheral chemoreceptor control
of breathing may be crucial to destabilize respiration in these tiny infants. Such instability generated by low O2 is also seen in adult subjects
climbing to altitudes, in whom low O2 induces
periodic breathing and apnea. The fact that an
increase in inspired O2, even a very small one,
will reduce or eliminate apneas in these infants
is further evidence that low O2 is central to this
disturbance of the control of breathing.12
Our study focused on physiologic measurements likely to disturb breathing in infants
breathing periodically as opposed to those
breathing continuously. Adult subjects very
rarely breathe periodically.15 In the infants studied, there was a gradual increase in TcPO2 and
TcPCO2 from the small to the large preterm
group. This occurred both in the subgroups
breathing periodically and continuously, although TcPO2 values for the periodic group
were uniformly lower than those for the continuous breathing group. Why is the arterial PO2
low in these infants as a group, and why is it even
lower in the subgroup breathing periodically?
The reason is likely the presence of intrapulmonary shunt. The more immature the infant, the
greater the shunt and the lower the arterialized
PO2. Infants breathing periodically would supposedly have more lung immaturity and more
shunt than those breathing continuously. Intrapulmonary shunt is also likely to be involved
in some term infants, although in this group
some degree of pulmonary hypertension may be
present. Lower TcPO2 values may also result
from a greater decrease in functional residual
capacity (FRC) in infants breathing periodically
which is in general associated with the stiffer
Increased Peripheral Chemoreceptor Activity
lungs.14 In previous studies, we demonstrated
that term infants with excessive periodic breathing (ⱖ50% of the sleeping time) were more
likely to develop Apparent Life Threatening
Events (ALTE).8
The present data suggest that infants breathing periodically are more hypoxemic than those
breathing continuously, at any age. Their baseline TcPO2 levels being low indicates that, during prolonged apneic pauses (ⱖ20 seconds),
their saturation may decrease to low levels. Indeed, previously we found that infants ⱕ1500 g
had a significant decrease in V̇E, accompanied
by a decrease in HbO2 from 92 to 80% during
the apneic period.33 Although speculative, this
decrease in saturation may represent a more
damaging insult than we have so far appreciated.
Unfortunately, studies trying to unravel the role
of these hypoxic events on late outcome have
used developmental markers such as the Bayley
test, which does not have the necessary discriminating power.34 These conventional markers
are affected by so many other variables that they
are unable to accurately assess the effect of one
single event. New strategies are needed to assess
the effects of these events on the ultimate outcome, but prevention of apnea by adjusting inspired O2 or distending the chest seems a reasonable thing to do.12
In conclusion, we have measured ventilatory
variables, transcutaneous gases, and peripheral
chemoreceptor activity at distinct ages in neonates and adult subjects. We found that ventilation per unit body weight decreases with age,
that the increased values early in life correspond
to lower TcPO2 and greater peripheral chemoreceptor activity. The lower TcPO2 in infants sits
on the steep portion of the ventilation/arterial
PO2 regression line, suggesting major changes
in ventilation with minor alterations in arterial
PO2. In addition, we found that neonates
breathing periodically have lower PO2 values
than those breathing regularly and therefore
may be subject to greater oscillations in
breathing. We suggest that this dependency of
respiratory pattern on peripheral chemoreceptor activity early in life is likely to offer
greater instability to the respiratory control
system, making it prone to oscillate and induce apnea.
271
Acknowledgments
We thank Marie Meunier Jackson for helping in the
preparation of this manuscript.
References
1. Barrington KJ, Finer NN: Periodic breathing and apnea
in preterm infants. Pediatr Res 27:118-121, 1990
2. Brady JP, Cotton EC, Tooley WH: Chemoreflexes in the
newborn infant: Effects of 100% O2 on heart rate and
ventilation. J Physiol 172:332-340, 1966
3. Davi M, Sankaran K, Simons K: Physiologic changes
induced by theophylline in the treatment of apnea in
preterm infants. J Pediatr 92:91-95, 1978
4. Fenner A, Schalk U, Hoenicke H, et al: Periodic breathing in premature and neonatal babies: Incidence,
breathing pattern, respiratory gas tensions, response to
changes in the composition of ambient air. Pediatr Res
7:174-183, 1973
5. Finer NN, Barrington KJ: Prolonged periodic breathing:
Significance in sleep studies. Pediatrics 89:450-453, 1992
6. Gabriel M, Albani M, Schulte FJ: Apneic spells and sleep
states in preterm infants. Pediatrics 57:142-147, 1976
7. Lee DS, Caces R, Kwiatkowski K, et al: A developmental
study on types and frequency distribution of short apneas (3 to 5 secs) in term and preterm infants. Pediatr
Res 22:344-349, 1987
8. Qurashi M, Kutbi I, Alvaro R, et al: Increased peripheral
chemoreceptor activity is critical in destabilizing breathing in term infants with excessive periodic breathing and
hypoxemia. Pediatr Res 51:326(abstr), 2002
9. Khan A, Qurashi M, Kwiatkowski K, et al: The vulnerability of the “CO2 Apneic Threshold” in neonates. Pediatr Res 49:380(abstr), 2001
10. Rigatto H, Brady JP: Periodic breathing and apnea in
preterm infants. I. Evidence for hypoventilation possibly
due to central respiratory depression. Pediatrics 50:202218, 1972
11. Rigatto H, Brady JP: Periodic breathing and apnea in
preterm infants. II. Hypoxia as a primary event. Pediatrics 50:219-228, 1972
12. Rigatto H: Periodic breathing, in Mathew O, Lenfant C
(eds): Lung Biology in Health and Disease. New York,
Marcel Dekker, Inc., 2003.
13. Shannon DC, Carley DW, Kelly DH: Periodic breathing:
Quantitative analysis and clinical description. Pediatr
Pulmonol 4:98-102, 1988
14. Thibeault DW, Wong MM, Auld PAM: Thoracic gas
volume changes in premature infants. Pediatrics 40:403411, 1967
15. Younes M: The physiologic basis of central apnea and
periodic breathing. Curr Pulmonol 10:265-365, 1989
16. Cross KW, Oppé TE: The effect of inhalation of high
and low concentrations of oxygen on the respiration of
the premature infant. J Physiol 117:38-55, 1952
17. Cherniack NS, Longobardo GS, Levine OR: Periodic
breathing in dogs. J Appl Physiol 21:1847-1854, 1966
18. Dempsey JA, Skatrud JB: A sleep-induced apneic threshold and its consequences. Am Rev Respir Dis 133:11631170, 1986
272
Al-Matary et al
19. Comroe JH: Physiology of Respiration (ed 2), Chicago,
Year Book Medical Publishers Inc., 1934, p 50
20. Comroe JH: Physiology of Respiration (ed 2), Chicago,
Year Book Medical Publishers Inc., 1934, p 64
21. Luz J, Winter A, Cates D, et al: Effect of chest and
abdomen uncoupling on ventilation and work of breathing in the newborn infant during sleep. Pediatr Res
16:297(abstr), 1982
22. Moriette G, Van Reempts P, Moore M, et al: The effect
of rebreathing CO2 on ventilation and diaphragmatic
electromyography in newborn infants. Respir Physiol
62:387-397, 1985
23. Fajardo C, Alvarez J, Wong A, et al: The incidence of
obstructive apneas in preterm infants with and without
bronchopulmonary dysplasia. Early Hum Dev 32:197206, 1993
24. Dreyfus-Brisac C: Ontogenesis of brain bioelectrical activity and sleep organization in neonates and infants, in
Falkner F, Tanner JM (eds): Human Growth. Vol. 3
Plenum, London, 1979, p. 157
25. Dreyfus-Brisac C: Ontogenesis of sleep in human prematures after 32 weeks of conceptional age. Dev Psychobiol
3:91-121, 1970
26. Rechtshaffen A, Kales A: A Manual of Standardized Terminology and Scoring System for Sleep Stages in Human
Subjects. Washington DC, US Gov. Printing Office, NIH
Pub. 204.
27. Kolobow T, Gattinoni L, Tomlinson TA, et al: Control of
28.
29.
30.
31.
32.
33.
34.
breathing using an extracorporeal membrane lung. Anesthesiology 46:138-141, 1977
Phillipson EA, Bowes G: Control of breathing during
sleep, Fishman AP, Cherniack NS, Widdicombe JG et al
(ed): Handbook of Physiology, Vol II, pt 2. Bethesda,
MD, Am Physiol Soc, 1986, pp 649 – 689
Rehan V, Haider AZ, Alvaro RE, et al: The biphasic
ventilatory response to hypoxia in preterm infants is not
due to a decrease in metabolism. Pediatr Pulmonol 22:
287-294, 1996
Sankaran K, Wiebe H, Seshia MMK, et al: Immediate and
late ventilatory response to high and low O2 in preterm
infants and adult subjects. Pediatr Res 13:875-878, 1979
Al-Hathlol K, Idiong N, Hussain A, et al: A study of
breathing pattern and ventilation in newborn infants
and adult subjects. Acta Paediatr 89:1420-1425, 2000
Lambertsen CJ, Kough RH, Cooper DY, et al: Oxygen
toxicity. Effects in man of oxygen inhalation at 1 and 3.5
atmospheres upon blood gas transport, cerebral circulation and cerebral metabolism. J Appl Physiol 5:471-486,
1953
Alvaro RE, Hussain A, Idiong N, et al: Periodic breathing
(PB) in small infants (ⱕ1500g): Ventilatory correlates
and significance. Pediatr Res 41:244(abstr), 1997
Kahn A, Rebuffat E, Franco P, et al: Apparent life-threatening events and apnea of infancy, in Beckerman RC,
Brouillette RT, Hunt CE (eds): Respiratory Control Disorders in Infants and Children Baltimore, MD, Williams
& Wilkins, 1992, pp 178 –189