Placenta (2005), Vol. 26, Supplement A, Trophoblast Research, Vol. 19 doi:10.1016/j.placenta.2005.01.003
advertisement

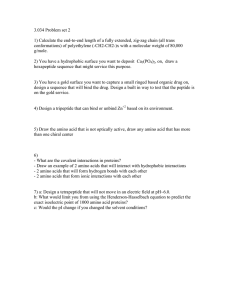
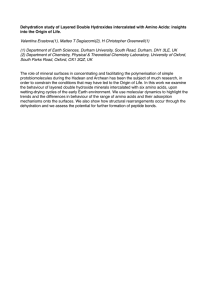
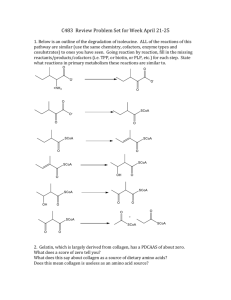
Placenta (2005), Vol. 26, Supplement A, Trophoblast Research, Vol. 19 doi:10.1016/j.placenta.2005.01.003 Fetoplacental Transport and Utilization of Amino Acids in IUGR — A Review T. R. H. Regnault*, J. E. Friedman, R. B. Wilkening, R. V. Anthony and W. W. Hay Jr. Perinatal Research Center, Department of Pediatrics, Division of Perinatal Medicine, University of Colorado Health Sciences Center, F441, Aurora, CO 80045, USA Paper accepted 6 January 2005 Amino acids have multiple functions in fetoplacental development. The supply of amino acids to the fetus involves active transport across and metabolism within the trophoblast. Transport occurs through various amino acid transport systems located on both the maternal and fetal facing membranes, many of which have now been documented to be present in rat, sheep and human placentas. The capacity of the placenta to supply amino acids to the fetus develops during pregnancy through alterations in such factors as surface area and specific time-dependent transport system expression. In intrauterine growth restriction (IUGR), placental surface area and amino acid uptakes are decreased in human and experimental animal models. In an ovine model of IUGR, produced by hyperthermia-induced placental insufficiency (PI-IUGR), umbilical oxygen and essential amino acid uptake rates are significantly reduced in the most severe cases in concert with decreased fetal growth. These changes indicate that severe IUGR is likely associated with a shift in amino acid transport capacity and metabolic pathways within the fetoplacental unit. After transport across the trophoblast in normal conditions, amino acids are actively incorporated into tissue proteins or oxidized. In the sheep IUGR fetus, however, which is hypoxic, hypoglycemic and hypoinsulinemic, there appear to be net effluxes of amino acids from the liver and skeletal muscle, suggesting changes in amino acid metabolism. Potential changes may be occurring in the insulin/IGF-I signaling pathway that includes decreased production and/or activation of specific signaling proteins leading to a reduced protein synthesis in fetal tissues. Such observations in the placental insufficiency model of IUGR indicate that the combination of decreased fetoplacental amino acid uptake and disrupted insulin/IGF signaling in liver and muscle account for decreased fetal growth in IUGR. Placenta (2005), Vol. 26, Supplement A, Trophoblast Research, Vol. 19 Ó 2005 Published by IFPA and Elsevier Ltd. Keywords: Amino acid; Placenta; Fetus; IUGR; Oxygen; Insulin; mTOR INTRODUCTION Amino acids and glucose constitute the carbon and nitrogen requirements for the placenta and fetus. Recently, a greater understanding of the fetal supply and metabolism of amino acids by the placenta during pregnancy has led to the concept that amino acids act as regulators of placental and fetal development. In addition to being a source of protein building blocks and oxidative fuel sources, amino acids influence metabolic cycling pathways between the placenta and fetus. They also act directly to regulate protein synthesis in various fetal and placental tissues through interactions with the insulin and IGF growth-promoting axis via regulation of the amount and/or activity of a key signal transduction protein, mammalian * Corresponding author. Perinatal Research Center, Department of Pediatrics, Division of Perinatal Medicine, University of Colorado Health Sciences Center, PO Box 6508, F441, Aurora, CO 80045, USA. Tel.: C1 303 724 1603; fax: C1 303 724 0898. E-mail address: tim.regnault@uchsc.edu (T.R.H. Regnault). 0143e4004/$esee front matter target of rapamycin (mTOR). This review deals with aspects of human and animal placental amino acid transport, fetal utilization of amino acids, and aspects of the fetal sheep insulin/IGF-I signaling pathway during normal pregnancy. Additionally, we discuss changes in these aspects as they occur in a sheep model of fetal growth restriction, and where possible compare them with human as well as other animal models of IUGR. AMINO ACID TRANSPORT ACROSS THE PLACENTA In recent years, both in vivo and in vitro studies have highlighted the complex characteristics of placental amino acid transport and metabolism (see reviews, [1e4]). Unlike an organ such as the liver, the placenta must carry out its own metabolic functions while also operating as an organ of transport, delivering amino acids from the maternal circulation into the fetal circulation. The concentrations of most amino Ó 2005 Published by IFPA and Elsevier Ltd. Regnault et al.: Fetoplacental Amino Acid Metabolism S53 acids, particularly some of the essential amino acids, are higher in fetal than maternal plasma (noted in rat, sheep and human pregnancies [5e9]), consistent with active transport of amino acids across the placenta. An increased fetal-to-maternal ratio of plasma amino acid concentrations has been documented for many species, and although the fetal/maternal concentration ratio is greater than 1.0 for most amino acids measured, there are quantitative differences among species, as reviewed [4]. The active in vivo transport of amino acids across the trophoblast involves three fundamental steps: (1) uptake from the maternal circulation across the microvillous membrane; (2) transport through the trophoblast cytoplasm; and (3) transport out of the trophoblast across the basal membrane into the umbilical circulation. This transport is regulated through transporter protein systems on both membranes of the trophoblast. Several mammalian amino acid transport systems have been characterized over the years by such general properties as ion-dependence, transport kinetics, substrate specificity, light chain and heavy chain interactions (monomeric or heterodimeric systems), and regulation of activity, which has allowed the description of multiple transport systems for neutral, anionic, and cationic amino acids [3,10e13]. Specific studies in the human and rat trophoblast have yielded more specific information concerning the location, direction of flux, and functioning of amino acid systems in the placenta (see reviews, [2,4]). Figure 1 represents a summary of selected trophoblast amino acid transport system activity location, for these two species, together with information detailing the related cDNA. In addition to the wide number of systems found to exist on the placental membranes, it is interesting to note that while each system is distinct in its operational requirements, many systems exhibit overlapping substrate specificity. Several of these systems are under investigation in the sheep placenta (GenBank Accession number: LAT-1, AY162432; LAT-2, AY162433; EAAT-1, AY157709; EAAT-2, AY157710; EAAT-3, AY157711) including examination of changes in their expression and transport capacity in IUGR and normal control conditions. Heavy (4F2hc or rBAT) and light chain associations System substrates Neutral AA ALA, SER, PRO, GLN MeAIB, AIB A ATA-1, -2 and –3 (SNAT-1, -2 and –4) [21, 116-122] ALA, SER, CYS, Anionic AA ASC ASCT-1 [56, 118, 119, 123-125] NEUTRAL AA, BCH Bo ASCT-2 [126-129] NEUTRAL AA, LYS, ARG, LEU bo,+ rBAT/bo,+ [23, 130-132] LEU, ILE, VAL, TRYP, PHE, MET, TYR, GLN, BCH L 4F2hc/LAT-1 and 4F2hc/LAT-2 [133-137] Cationic AA y +L 4F2hc/ y+LAT-1 and 4F2hc/ y+LAT -2 [23, 55, 131, 138-142] Cationic AA y+ CAT-1, -2B and -4 [22, 23, 138, 139, 143, 144, 145] Anionic AA GLU, ASP XAG- EAAT-1, -2 and -3 [146-150] TAU β TAUT [122, 151-153] Apical membrane Basal membrane Figure 1. Schematic representation of selected sodium-dependent (C) and sodium-independent (B) amino acid transport system activity location for both the apical (maternal) and basal (fetal) facing membranes. Amino acid substrates and the heavy and light chain proteins interactions for each of these placental-specific systems are listed. References for each system’s trophoblast activity location and heavy and light chain interactions are also provided. Notes: substrates in bold represent essential amino acids; MeAIB, methylaminoisobutyric acid; AIB, a-aminoisobutyric acid; BCH, 2-aminobicyclo-(2,2,1)-heptane-2-carboxylic acid. S54 PLACENTAL AMINO ACID TRANSPORT CAPACITY An important aspect of placental transport capacity relates to the total placental surface area across which transport can occur. As pregnancy advances, the increasing nutrient demands of the developing conceptus must be met through an appropriate increase in placental nutrient transport capacity. This enhanced performance is facilitated through alterations in placental perfusion and changes in membrane exchange surface area size and function. Fetal weight increases approximately 20-fold between weeks 16 and 40 (term) of gestation in the human, whereas the peripheral villous surface area increases only ninefold [14e17]. Thus, the increased microvillous density on trophoblast cells alone cannot explain the exponential fetal growth occurring over this time period, indicating that fetal growth is supported not only by changes in villous surface area, but rather by the overall change in total exchange capacity. The makeup of this capacity includes the concentration and affinity characteristics of specific amino acid carrier proteins on the cell membrane surface and circulating amino acid concentrations. Accompanying the maturational changes in trophoblast surface area, the capacities of the amino acid transport systems change with differing expression and transport parameters throughout gestation [18e23]. For example, in the human firsttrimester microvillous membrane has increased transport activity compared to term placental vesicles [20], and the protein concentration of the heavy chain, 4F2hc (CD98), which is associated with heterodimeric transport systems, differ between early/mid pregnancy and term placenta [19,23]. Also of interest is that in early gestation, the Km of the microvillous high affinity System yCL is significantly less than in term preparations [23]. It is also observed that the same amino acid may be transported through different systems, depending upon which membrane is being crossed. In term placenta, L-arginine transport in microvillous membrane preparations is believed to occur through both yC and yCL systems, while in the fetal facing basal membrane, transport may be restricted to the yCL system [23]. Such studies highlight the complex interactions that occur between developing microvillous membrane and basal membrane, within the trophoblast and between the two circulations, to facilitate an increase in nutrient delivery to the growing fetus as gestation advances. Circulating maternal amino acid concentrations also play a major role in influencing placental amino acid transport capacity and ultimately determining fetal supply of amino acids. In sheep studies, the simultaneous flux from maternal to fetal circulations has been studied for the essential amino acids [24e26]. These recent studies demonstrate striking differences for rates of placental clearance of the essential amino acids where clearance is most rapid for valine, leucine, isoleucine, phenylalanine, and methionine, with differences in their transplacental flux directly attributable to the differences in their concentrations in maternal plasma [25]. This observation among several amino acids studied Placenta (2005), Vol. 26, Supplement A, Trophoblast Research, Vol. 19 simultaneously is supported by experiments in which the concentration of individual amino acids is increased in the maternal circulation by infusion, showing that net umbilical uptake of the amino acid increases directly with its maternal plasma concentration. This has been shown for alanine, leucine, lysine, threonine, and glycine [27e31]. However, because of competitive inhibition among multiple amino acids for common transporters, when a large number of amino acids are given to the mother simultaneously, the umbilical uptake of some amino acids increases, but not that of all amino acids [25,26,32]. These observations have direct clinical relevance, as trials of infusions of mixed amino acid solutions into pregnant women to improve amino acid supply to the fetus might produce an imbalance in the actual uptake of amino acids by the fetus, not necessarily a potentially good therapeutic result. Such studies also have shown that placental transport of a given amino acid is a function of its concentration in the maternal plasma and the concentration of inhibitory amino acids, and such relationships are different for each amino acid. Studies in human normal and IUGR pregnancies show similar relationships among maternal plasma concentrations of amino acids and net placental transport to the fetus [33,34]. AMINO ACID TRANSPORT IN ANIMAL MODELS OF PLACENTAL INSUFFICENCY – IUGR AND HUMAN IUGR Human placental insufficiency is difficult to study, for ethical and practical reasons, and is frequently limited to studies at term. Thus, the mechanisms responsible for placental insufficiency and IUGR can be best investigated in animal models. Several laboratories have used the pregnant sheep to study early placental growth and development [35,36], and placentalefetal physiological interactions [37e42]. Growth restriction in fetal sheep can be induced by nutritional restriction, placental infarction with microspheres, reduction of placental implantation sites, uterine or umbilical artery clamping or ligation, and exposure of the pregnant ewe to elevated ambient temperatures (hyperthermia model; [35,41,43e45]). The maternal hyperthermia model involves prolonged increases in maternal core body temperature (w0.6e0.8(C increase; [46]). It is a naturally occurring condition common to sheep that live in warm climates that have a ‘‘spring’’ estrus and carry the pregnancy through the hotter summer months. This model produces placental insufficiency (PI) resulting in IUGR that shares many of the commonly measured characteristics of human IUGR that results from placental insufficiency [47,48], in contrast to mechanical models of placental growth inhibition that usually are imposed late in gestation and involve either surgical reductions in placental size or relatively severe reductions in uterine and/or umbilical blood flow, none of which are characteristic of the common form of human placental growth restriction and nutrient transport insufficiency. Since the early 1980s, our efforts have focused on validating the maternal Regnault et al.: Fetoplacental Amino Acid Metabolism S55 Transplacental PO2 gradient (mm Hg) hyperthermia form of fetal growth restriction as a natural experimental model of IUGR, and to compare it to similar studies of human IUGR [27,29,35,37,41,42,46,49]. In the hyperthermia-induced IUGR model (PI-IUGR), reduction in fetal oxygenation ranges from mild to severe, with similar variable reductions in placental and fetal weights. In the more severe cases, net umbilical oxygen uptake rate (UO2U, mmol/min/kg fetus) and the ratio between oxygen uptake and the transplacental arterial PaO2 gradient (UO2U/ DPO2, mmol/min/100 g placenta/mmHg) are both significantly reduced (Regnault et al., Unpublished data). The reduced UO2U/DPO2 ratio specifically defines a decreased placental oxygen diffusion capacity. More recent studies examining severe IUGR fetuses have defined a significant relationship between placental weight and the increasing transplacental PaO2 gradient (Figure 2). In these IUGR fetus the UO2U/DPO2 ratio is reduced by almost 35%. Such observations indicate that the IUGR trophoblast, in this model, has developed reductions in possibly two of the primary factors associated with diffusing capacity, permeability and surface area, and therefore a reduced placental functional capacity. Furthermore, another experimental model of IUGR supports this observation. In transgenic mice with a deletion of the placental-specific transcript (P0) of the Igf2 gene, placental surface area is reduced and placental thickness increased, significantly reducing the theoretical diffusing capacity of these placentae [50,51]. It is interesting to note that in studies specifically concerned with abnormal placental development near term in human IUGR, there is a reduction in inter-microvillous space and absolute value for microvillous and total trophoblastic surface area [52e54], supportive also of a reduced placental functional capacity. Actual absolute placental amino acid transport is reduced in cases of placental and fetal growth restriction. Reduced uptake of leucine and lysine in vesicles prepared from human IUGR placentae has been described and indicates decreased transporter concentrations and/or activity for neutral and cationic amino acids [55]. Also, in the maternal dietary protein deprivation model of IUGR in the rat, there appears to be a down regulation of placental amino acid transport in systems 60 50 40 R2 = 0.79 30 20 10 0 0 100 200 300 400 500 600 Placental weight (g) Figure 2. Relationship between transplacental oxygen gradient (uterine venous PO2 less umbilical venous PO2, mmHg) and placental weight (g) in control (C) and IUGR (B) animals near term at 135 days gestational age. Xÿ AG A, y and [56,57]. In the PI-IUGR model there is a reduction of maternal leucine flux into the placenta and into the fetus. In contrast to these changes in placental leucine flux, the uteroplacental oxygen and glucose consumption rates are similar to control animals on a per gram basis, indicating that the decrease in leucine metabolism is not a result of reduced placental metabolic rate [29]. The reduction of leucine flux into the placenta is believed to be the result of a deficiency in the number and/or activity of amino acid transporters in the IUGR placenta. Both fetal leucine concentration and the flux of leucine from the fetus back to the placenta are reduced, and fetal oxidation of leucine is decreased [29]. These findings are similar to those reported to occur in human IUGR [58,59]. Specifically, the fetal/maternal ratio of leucine has been correlated with the severity of growth restriction, and as in sheep IUGR studies, demonstrates a decreased transplacental leucine flux and/or increased protein breakdown within the IUGR fetoplacental compartments [58]. More recent studies in the PI-IUGR sheep model have highlighted other specific defects in the placental neutral and anionic amino acid transport systems [49,60]. Current research in the sheep PI-IUGR model is attempting to determine the exact nature of these changes through examination of System L and Xÿ AG transport isoform expression and surface area calculations. These human and animal studies clearly demonstrate that a number of important amino acid transport systems on both membranes of the trophoblast are impaired in experimental models and natural conditions of placental and fetal growth restriction. Earlier studies in humans showed reduced concentrations of essential amino acids such as leucine and lysine in growthrestricted fetuses [61e63], indicating possible alterations in placental amino acid transporter systems. Recently, however, in situations of well-defined IUGR, but with significantly lower than normal umbilical venous oxygen saturation, oxygen content, and pH, umbilical venous concentrations of leucine and phenylalanine were not significantly different from the AGA pregnancies [59]. Interestingly in the sheep model of placental insufficiency induced IUGR, we also observe that while there are significant reductions in the placental flux of the essential amino acids leucine and threonine [27,29], amino acid concentrations are not necessarily different from normal concentrations. For example in the earlier leucine flux studies, fetal arterial leucine concentration was significantly reduced (w30%) [29], while in later studies, concentrations of threonine were not significantly different between the two study groups [27], yet in both studies, significant reductions in specific amino acid flux per unit placenta were observed. Furthermore, in past and current studies of severely hypoxic and hypoglycemic sheep fetuses in which umbilical uptake of the essential amino acids is significantly reduced, fetal essential amino acid concentrations are unaltered compared to control animals [64e67], similar to observations in humans and guinea pigs [68e70]. It is possible that in the presence of relatively more hypoxic and hypoglycemic conditions, a hypometabolic state within the IUGR fetus contributes to the maintenance of essential amino acid concentrations, despite reduced umbilical uptakes. Despite C S56 these observations of highly variable differences in fetal amino acid concentrations among conditions and models, both human and animal studies emphasize that placental amino acid transport is reduced in cases of placental growth restriction. This reduction is likely a combination of many factors including changes in trophoblast exchange capacity as well as uteroplacental oxygenation and fetoplacental metabolism. FETAL HEPATIC AND SKELETAL MUSCLE UTILIZATION OF AMINO ACIDS During normal fetal development there is no appreciable rate of fetal hepatic gluconeogenesis. Fetal hepatic glucose production would be counterproductive since an increased glucose concentration would reduce the transplacental glucose gradient, leading to decreased umbilical glucose uptake from the mother [71,72]. Although gluconeogensis in the adult liver consumes amino acids, there is no measurable fetal gluconeogenesis, despite the higher concentration of amino acids in the fetal rather than the maternal circulations. However, there is in fact a high rate of hepatic uptake of all of the essential and most of the nonessential amino acids by both lobes of the fetal liver [7,73], including all of the gluconeogenic amino acids. In fetal life, the carbon from these amino acids is released primarily as glutamate and pyruvate with a smaller contribution coming from the hepatic release of serine, ornithine, and aspartate [7,74e76], in contrast to postnatal life, where the carbon from these amino acids is released from the liver solely as glucose. Studies concerned with hepatic function in the model of PI-IUGR are currently being conducted. However, it is interesting to note that in the situation of experimentally elevated fetal dexamethasone levels, analogous to elevated cortisol concentrations as in other models of IUGR, hepatic glutamine and alanine uptakes and hepatic glutamate output are reduced [77]. This might suggest that in the hypoxic, hypoglycemic IUGR fetus, hepatic glutamine and alanine uptakes may also be reduced. Under normal physiologic conditions, the hind limb of a growing ovine fetus shows net uptake of both essential and nonessential amino acids from the fetal circulation, presumably contributing to the relatively high nitrogen accretion rate of the fetus [78]. The fetal hind limb also has no net release of alanine [73], in contrast to the adult hind limb that displays a large output of alanine and glutamine [79]. The normal ovine fetal hind limb also consumes the two amino acids that are not supplied by the placenta: glutamate and serine, which are produced from the fetal liver in amounts that could account for the combined uptake of glutamate by both placenta and hind limb [75,76,78,80]. With reduced placental supply of glucose to the growth-restricted fetus, there is likely an increased efflux of the gluconeogenic amino acids, glutamine and alanine, and the Branched Chain Amino Acids (BCAA) from the fetal hind limb, possibly from increased rates of protein breakdown, as has been demonstrated to occur in fetal hypoglycemic studies [65,66,81]. Placenta (2005), Vol. 26, Supplement A, Trophoblast Research, Vol. 19 CHANGES IN INSULIN, IGF-I AND AMINO ACID REGULATION OF THE INSULIN/IGF-I SIGNALING PATHWAY IN IUGR In the hyperthermia-induced ovine model of placental insufficiency, the fetuses are hypoxic, hypoglycemic [41,42], and hypoinsulinemic and have reduced circulating IGF-I concentrations (Regnault et al., unpublished data). Importantly, with respect to the growth-restricted fetus, insulin and, to a lesser extent, the IGFs activate protein synthesis via the PI 3-kinase/ Akt/mTOR/p70S6k/4E-BP-1/eIF4E signaling pathway, as illustrated schematically in Figure 3. Recent, studies have established the initiation phase of mRNA translation as a pivotal site of regulation for global rates of protein synthesis, as well as a site through which the synthesis of specific proteins is controlled [82]. Activation of the insulin and IGF-1 receptor triggers docking of the insulin receptor substrate-1 (muscle), INSULIN IGF-I α S S β α β p p IRS-1,2 p p85 p p110 PI 3 Kinase p Akt-1,2 Hypoxia p mTOR Amino Acids GSK-3b p Glycogen p p P70 S6K 4E-BP1 p Ribosomal protein GS S6 eIF4E Complex Translation initiation GDP eIF2B GTP Protein Synthesis Figure 3. A schematic representation of control of mRNA translation initiation by growth factors insulin and IGF-1. The signaling pathway from tyrosine kinase receptors activates insulin receptor substrates (IRS)-1,2, p85 phosphatidylinositol-3-kinase, Akt, and mTOR. Glycogen Synthase Kinase-3b (GSK-3b) is a major negative regulator of Glycogen Synthase (GS) enzyme. Insulin-mediated phosphorylation of GSK-3 via Akt relieves this inhibition. Insulin and amino acids stimulate, while hypoxia inhibits the phosphorylation of mTOR to control downstream signaling of protein synthesis. Activation of mTOR increases phosphorylation of the suppressor 4E-BP-1, thereby reducing its affinity for eIF4E. Release of eIF4E enables formation of eIF4E complex, allowing eIF2B to bind GTP and interact with Met-tRNA and the 40S ribosomal subunit of mRNA, thereby promoting protein synthesis. The p70S6 kinase is directly phosphorylated by mTOR and triggers phosphorylation of ribosomal protein S6 at multiple sites. S6 kinases are required for promoting the translation of mRNAs. Regnault et al.: Fetoplacental Amino Acid Metabolism -2 (liver), and the catalytic activation of phosphatidylinositol3-kinase (PI 3-kinase) mediated by binding and phosphorylation of the 85 kDa PI 3-kinase regulatory subunit. PI 3-kinase activation triggers phosphorylation of the serine/threonine kinases Akt-1, -2, -3 [83]. Akt phosphorylates and thereby activates the protein kinase mammalian target of rapamycin (mTOR) [84,85]. Mammalian target of rapamycin appears to be a key regulator of cell growth by sensing upstream nutrient and hormonal signals to coordinate gene activation, protein synthesis, and cell growth [85,86]. Mammalian target of rapamycin is a serine/threonine kinase that phosphorylates and thereby coordinates the function of the translational suppressor-eukaryotic translation initiation factor 4E binding protein 1 (4E-BP1) and the 70 kDa small ribosomal subunit kinase (p70S6k) [87]. Under conditions of substrate sufficiency (amino acids and glucose) and hormonal stimulation, mTOR phosphorylates the 4E-BP1 repressor on several sites, triggering its dissociation from the inactive 4E-BP-1eIF4E complex [88,89], thus making eIF4E available for binding to eIF4G. The eIF4E binds to the mRNA cap structure present at the 5#-end of all nuclear transcribed mRNAs to form an eIF4Emethionyl-tRNAi complex. The eIF4EmRNA complex binds to eIF4G and eIF4A, forming the active eIF4F complex, thereby allowing translation to proceed. Similar to human IUGR, the ovine model of IUGR also displays decreased fetal insulin and IGF-I circulating concentrations (Regnault et al., unpublished data). In association with this, in the ovine IUGR, there appears to be up regulation of the proximal signals for insulin action involved in control of glucose metabolism (Regnault et al., unpublished data). This up regulation includes an increase of the insulin receptor and a suppression of glycogen synthase kinase-3-b, which normally suppresses glycogen synthesis. Insulin normally inactivates GSK-3b, which thereby dephosphorylates glycogen synthase (GS), leading to the activation of GS [90,91]. Low levels of GSK-3b would therefore tend to favor GS activity and consequently an elevation in glycogen formation. In preliminary studies in our laboratory, fetal hepatic glycogen concentrations in IUGR are indeed elevated, which is similar to what has been previously observed in hyperthermic exposed fetuses [92]. This elevation could be due to a higher GS activity, and/or possibly less glycogen phosphorylase. Interestingly, while there is an up regulation at the proximal end of the insulin signaling pathway, we have observed a concomitant decrease in protein expression more distally in the insulin signaling cascade leading to protein translation. Initiation factor eIF4E is significantly reduced by 63% in IUGR livers, while the translational repressor 4E-BP1 is significantly increased, 2.5-fold (Regnault et al., unpublished data). The significant increase in the downstream translational repressor 4E-BP1, combined with a decrease in the limited amount of eIF4E may be a key mechanism limiting protein translation in IUGR livers. There also appears to be an increase in proximal insulin signaling in muscle despite reduced insulin/IGF-I S57 concentrations in growth-restricted ovine fetuses. Insulin receptor protein in skeletal muscle is increased 77%, while there is a 36% decrease in the amount of the p85a subunit of PI 3-kinase in skeletal muscle from the IUGR fetuses (Regnault et al., unpublished data). It has recently been demonstrated that reduced expression of the murine p85a subunit of PI 3-kinase in heterozygous knockout mice actually improves insulin signaling and ameliorates diabetes, indicating that p85a expression is negatively correlated with insulin sensitivity [93,94]. The mechanism for this effect involves enhanced coupling between the p85a and p110 subunits and increased PI 3-kinase production in mice in vivo. These changes in insulin receptor and p85a may therefore be compensatory responses to low insulin concentrations and/or simultaneous hypoglycemia, and could favor increased responsiveness to insulin to facilitate increased glucose uptake. In contrast to the liver, the levels of 4E-BP1 and eIF4E examined in fetal skeletal muscle from IUGR animals are unchanged, indicating that fetal growth restriction may have tissue-specific effects on mechanisms for reduced organ growth. However, mTOR was reduced significantly by 38% in hind limb skeletal muscle from IUGR fetuses (Regnault et al., unpublished data). A decrease in mTOR expression potentially has multiple downstream consequences that could lead to a decrease in fetal growth. The mTOR-dependent p70S6K and 4E-BP1/eIF4E pathways are activated independently during muscle growth in vivo [84,95] and these pathways cooperate with each other to promote cell growth and increased cell size. mTOR also coordinates the cellular responses to extracellular nutrient concentrations by modulating nutrient transporter gene expression [85,89,96,97]. The reasons for the reduced mTOR in muscle cells from growthrestricted fetuses are not known. Amino acids, particularly the BCAA, leucine, stimulate mTOR in a number of tissues in the adult [88,98e100], and reduced levels of mTOR may be associated with reduced intracellular amino acid concentrations. As previously mentioned, under hypoxic conditions amino acids leave the cell, including the BCAAs from the fetal muscle [70], which is the only site of BCAA utilization besides the placenta [101,102], and this associated change in mTOR may potentially represent a direct site of protein synthesis control in the growth-restricted fetus. Other factors that impact mTOR signaling include reduced cellular energy (ATP/AMPK levels) [103e105], and DNA damage through changes in the transcription factor p53 [106,107]. The transcription factor p53 is an important regulator of cell cycle progression and apoptosis and has been associated with apoptosis in IUGR fetuses [108e111]. It negatively regulates the expression of Bcl-2 and up regulates Bax expression [112,113], and these two cell transcription factors play major roles in activating the caspase-3 pathway which is necessary for the chromatin condensation and DNA fragmentation that characterize apoptosis [114]. mTOR is also directly regulated by decreased oxygen partial pressure [115]. The reversible inhibition of protein synthesis by hypoxia is thought to be an important aspect of energy S58 conservation in an oxygen deficient environment. Arterial PO2 in growth-restricted fetuses may be as low as 12 mmHg (w2% oxygen), which is similar to the oxygen partial pressures in cell culture conditions in which reduced oxygen levels have been suggested to initiate cellular energy conservation strategies, including the hypophosphorylation of mTOR, independent of other commonly associated hypoxia changes, such as ATP levels, HIF-1 and Akt/protein kinase B and AMP-activated protein kinase phosphorylation [115]. CONCLUSIONS In severe cases of placental and fetal growth restriction, particularly as shown in a well established ovine model of Placenta (2005), Vol. 26, Supplement A, Trophoblast Research, Vol. 19 IUGR with placental insufficiency, the increased transplacental gradients for oxygen is not large enough to overcome the reduced diffusion capacities of the growth-restricted placenta. Both limited oxygen and nutrient substrate supplies, therefore, limit the capacity for fetal protein accretion and may augment mechanisms leading to protein breakdown. Furthermore, hypoxia, reduced nutrient supplies and intracellular concentrations of nutrient substrates may initiate differential cellular energy conservation strategies, some of which may not be fully reversible. The complete mechanisms by which oxygen, nutrient substrates, and related anabolic hormones and growth factors regulate placental amino acid uptake, fetal utilization and metabolism, and cellular growth remain to be a field of active investigation. ACKNOWLEDGMENTS The authors wish to sincerely thank our colleagues, past and present, and all the staff of the Perinatal Research Center who over the many years, have helped contribute to improving our understanding of the placental transport and the fetoplacental metabolism of amino acids. We are grateful to the National Institute of Child Health and Human Development for the funding that has supported this work. REFERENCES [1] Cetin I. Amino acid interconversions in the fetaleplacental unit: the animal model and human studies in vivo. Pediatric Research 2001;49(2): 148e54. [2] Jansson T. Amino acid transporters in the human placenta. Pediatric Research 2001;49(2):141e7. [3] Kudo Y, Boyd CA. Human placental amino acid transporter genes: expression and function. Reproduction 2002;124:593e600. [4] Regnault TRH, de Vrijer B, Battaglia FC. Transport and metabolism of amino acids in placenta. Endocrine 2003;19(1):23e41. [5] Beckman DA, Pugarelli JE, Jensen M, Koszalka TR, Brent RL, Lloyd JB. Sources of amino acids for protein synthesis during early organogenesis in the rat. I. Relative contributions of free amino acids and of proteins. Placenta 1990;11(2):109e21. [6] Lemons JA, Adcock EW, Jones MDJ, Naughton MA, Meschia G, Battaglia FC. Umbilical uptake of amino acids in the unstressed fetal lamb. The Journal of Clinical Investigation 1976;58(6):1428e34. [7] Marconi AM, Battaglia FC, Meschia G, Sparks JW. A comparison of amino acid arteriovenous differences across the liver and placenta of the fetal lamb. American Journal of Physiology 1989;257(6 Pt 1): E909e15. [8] Philipps AF, Holzman IR, Teng C, Battaglia FC. Tissue concentrations of free amino acids in term human placentas. American Journal of Obstetrics and Gynecology 1978;131(8):881e7. [9] Montgomery D, Young M. The uptake of naturally occurring amino acids by the plasma membrane of the human placenta. Placenta 1982; 3(1):13e20. [10] Christensen HN. Methods for distinguishing amino acid transport systems of a given cell or tissue. Federation Proceedings 1966;25(3): 850e3. [11] Christensen HN. Amino acid nutrition across the placenta. Nutrition Reviews 1992;50(1):13e5. [12] Kilberg MS, Stevens BR, Novak DA. Recent advances in mammalian amino acid transport. Annual Review of Nutrition 1993;13:137e65. [13] Yudilevich DL, Sweiry JH. Transport of amino acids in the placenta. Biochimica et Biophysica Acta 1985;822(2):169e201. [14] Baur R. Morphometry of the placental exchange area. Advances in Anatomy, Embryology, and Cell Biology 1977;53(1):3e65. [15] Teasdale F. Gestational changes in the functional structure of the human placenta in relation to fetal growth: a morphometric study. American Journal of Obstetrics and Gynecology 1980;137(5):560e8. [16] Teasdale F. Morphometric evaluation. Contributions to Gynecology and Obstetrics 1982;9:17e28. [17] Teasdale F, Jean-Jacques G. Morphometric evaluation of the microvillous surface enlargement factor in the human placenta from midgestation to term. Placenta 1985;6(5):375e81. [18] Mahendran D, Donnai P, Glazier JD, D’Souza SW, Boyd RD, Sibley CP. Amino acid (system A) transporter activity in microvillous membrane vesicles from the placentas of appropriate and small for gestational age babies. Pediatric Research 1993;34(5):661e5. [19] Okamoto Y, Sakata M, Ogura K, Yamamoto T, Yamaguchi M, Tasaka K, et al. Expression and regulation of 4F2hc and hLAT1 in human trophoblasts. American Journal of Physiology - Cell Physiology 2002;282(1):C196e204. [20] Mahendran D, Byrne S, Donnai P, D’Souza SW, Glazier JD, Jones CJ, et al. Na+ transport, H+ concentration gradient dissipation, and system A amino acid transporter activity in purified microvillous plasma membrane isolated from first-trimester human placenta: comparison with the term microvillous membrane. American Journal of Obstetrics & Gynecology 1994;171(6):1534e40. [21] Novak DA, Beveridge MJ, Malandro M, Seo J. Ontogeny of amino acid transport system A in rat placenta. Placenta 1996;17(8):643e51. [22] Malandro MS, Beveridge MJ, Kilberg MS, Novak DA. Ontogeny of cationic amino acid transport systems in rat placenta. American Journal of Physiology 1994;267(3 Pt 1):C804e11. [23] Ayuk PT, Sibley C, Donnai P, D’Souza S, Glazier J. Development and polarization of cationic amino acid transporters and regulators in the human placenta. American Journal of Physiology 2000;278(6):c1162e71. [24] Jozwik M, Teng C, Wilkening RB, Meschia G, Tooze J, Chung M, et al. Effects of branched-chain amino acids on placental amino acid transfer and insulin and glucagons release in the ovine fetus. American Journal of Obstetrics & Gynecology 2001;185(2):487e95. [25] Paolini CL, Meschia G, Fennessey PV, Pike AW, Teng C, Battaglia FC, et al. An in vivo study of ovine placental transport of essential amino acids. American Journal of Physiology e Endocrinology & Metabolism 2001;280(1):E31e9. [26] Jozwik M, Teng C, Wilkening RB, Meschia G, Battaglia FC. Reciprocal inhibition of umbilical uptake within groups of amino acids. American Journal of Physiology. Endocrinology and Metabolism 2004;286(3): E376e83. [27] Anderson AH, Fennessey PV, Meschia G, Wilkening RB, Battaglia FC. Placental transport of threonine and its utilization in the normal and growth-restricted fetus. American Journal of Physiology 1997;272 (5 Pt 1):E892e900. [28] Geddie G, Moores R, Meschia G, Fennessey P, Wilkening R, Battaglia FC. Comparison of leucine, serine and glycine transport across the ovine placenta. Placenta 1996;17(8):619e27. Regnault et al.: Fetoplacental Amino Acid Metabolism [29] Ross JC, Fennessey PV, Wilkening RB, Battaglia FC, Meschia G. Placental transport and fetal utilization of leucine in a model of fetal growth retardation. American Journal of Physiology 1996;270(3 Pt 1): E491e503. [30] Timmerman M, Chung M, Wilkening RB, Fennessey PV, Battaglia FC, Meschia G. Relationship of fetal alanine uptake and placental alanine metabolism to maternal plasma alanine concentration. American Journal of Physiology 1998;275(6 Pt 1):E942e50. [31] Wilkes PT, Meschia G, Teng C, Zhu Y, Wilkening RB, Battaglia FC. The effect of an elevated maternal lysine concentration on placental lysine transport in pregnant sheep. American Journal of Obstetrics and Gynecology 2003;189(5):1494e500. [32] Jozwik M, Teng C, Battaglia FC, Meschia G. Fetal supply of amino acids and amino nitrogen after maternal infusion of amino acids in pregnant sheep. American Journal of Obstetrics and Gynecology 1999; 180(2 Pt 1):447e53. [33] Ronzoni S, Marconi AM, Cetin I, Paolini CL, Teng C, Pardi G, et al. Umbilical amino acid uptake at increasing maternal amino acid concentrations: effect of a maternal amino acid infusate. American Journal of Obstetrics & Gynecology 1999;181(2):477e83. [34] Ronzoni S, Marconi AM, Paolini CL, Teng C, Pardi G, Battaglia FC. The effect of a maternal infusion of amino acids on umbilical uptake in pregnancies complicated by intrauterine growth restriction. American Journal of Obstetrics and Gynecology 2002;187(3):741e6. [35] Bell AW, Wilkening RB, Meschia G. Some aspects of placental function in chronically heat-stressed ewes. Journal of Developmental Physiology 1987;9:17e29. [36] Ehrhardt RA, Bell AW. Growth and metabolism of the ovine placenta during mid-gestation. Placenta 1995;16(8):727e41. [37] Bell AW, McBride BW, Slepetis R, Early RJ, Currie WB. Chronic heat stress and prenatal development in sheep: I. Conceptus growth and maternal plasma hormones and metabolites. Journal of Animal Science 1989;67(12):3289e99. [38] Green LR, Kawagoe Y, Hill DJ, Richardson BS, Han VK. The effect of intermittent umbilical cord occlusion on insulin-like growth factors and their binding proteins in preterm and near-term ovine fetuses. Journal of Endocrinology 2000;166(3):565e77. [39] Jensen EC, Harding JE, Bauer MK, Gluckman PD. Metabolic effects of IGF-I in the growth retarded fetal sheep. Journal of Endocrinology 1999;161(3):485e94. [40] Owens JA, Falconer J, Robinson JS. Effect of restriction of placental growth on oxygen delivery to and consumption by the pregnant uterus and fetus. Journal of Developmental Physiology 1987;9(2):137e50. [41] Thureen PJ, Trembler KA, Meschia G, Makowski EL, Wilkening RB. Placental glucose transport in heat-induced fetal growth retardation. American Journal of Physiology 1992;263:R578e85. [42] Regnault TRH, de Vrijer B, Galan HL, Davidsen ML, Trembler KA, Battaglia FC, et al. The relationship between transplacental O2 diffusion and placental expression of P1GF, VEGF and their receptors in a placental insufficiency model of fetal growth restriction. Journal of Physiology 2003;550:641e56. [43] Alexander G, Williams D. Heat stress and development of the conceptus in domestic sheep. Journal of Agricultural Science 1971;76: 53e72. [44] Yeates NTM. Foetal dwarfism in sheep e an effect of high atmospheric temperature during gestation. Journal of Agricultural Science 1958;51: 84e9. [45] Shelton M, Huston JE. Effects of high temperature stress during gestation on certain aspects of reproduction in the ewe. Journal of Animal Science 1968;27(1):153e8. [46] Regnault TRH, Orbus RJ, Battaglia FC, Wilkening RB, Anthony RV. Altered arterial concentrations of placental hormones during maximal placental growth in a model of placental insufficiency. Journal of Endocrinology 1999;162(3):433e42. [47] Regnault TRH, Galan HL, Parker TA, Anthony RV. Placental development in normal and compromised pregnancies e a review. Placenta 2002;23(Suppl A, Trophoblast Research 16):S119e29. [48] Anthony RV, Scheaffer AN, Wright CD, Regnault TRH. Ruminant models of prenatal growth restriction. Reproduction 2003;61(Suppl.): 183e94. [49] de Vrijer B, Regnault TR, Wilkening RB, Meschia G, Battaglia FC. Placental uptake and transport of ACP, a neutral nonmetabolizable S59 [50] [51] [52] [53] [54] [55] [56] [57] [58] [59] [60] [61] [62] [63] [64] [65] [66] [67] [68] [69] amino acid, in an ovine model of fetal growth restriction. American Journal of Physiology. Endocrinology and Metabolism 2004;287: E1114e24. Constancia M, Hemberger M, Hughes J, Dean W, Ferguson-Smith A, Fundele R, et al. Placental-specific IGF-II is a major modulator of placental and fetal growth. Nature 2002;417(6892):945e8. Sibley CP, Coan PM, Ferguson-Smith AC, Dean W, Hughes J, Smith P, et al. Placental-specific insulin-like growth factor 2 (Igf2) regulates the diffusional exchange characteristics of the mouse placenta. Proceedings of the National Academy of Science USA 2004;101(21):8204e8. Mayhew TM, Ohadike C, Baker PN, Crocker IP, Mitchell C, Ong SS. Stereological investigation of placental morphology in pregnancies complicated by pre-eclampsia with and without intrauterine growth restriction. Placenta 2003;24(2e3):219e26. Teasdale F, Jean-Jacques G. Intrauterine growth retardation: morphometry of the microvillous membrane of the human placenta. Placenta 1988;9(1):47e55. Woods DL, Rip MR. Placental villous surface area of light-for-dates infants at term. Early Human Development 1987;15(2):113e7. Jansson T, Scholtbach V, Powell TL. Placental transport of leucine and lysine is reduced in intrauterine growth restriction. Pediatric Research 1998;44(4):532e7. Malandro MS, Beveridge MJ, Kilberg MS, Novak DA. Effect of lowprotein diet-induced intrauterine growth retardation on rat placental amino acid transport. American Journal of Physiology 1996;271(1 Pt 1): C295e303. Rosso P. Maternalefetal exchange during protein malnutrition in the rat. Placental transfer of glucose and a nonmetabolizable glucose analog. The Journal of Nutrition 1977;107(11):20006e10. Marconi AM, Paolini CL, Stramare L, Cetin I, Fennessey PV, Pardi G. Steady state maternalefetal leucine enrichments in normal and intrauterine growth-restricted pregnancies. Pediatric Research 1999; 46(1):114e9. Paolini CL, Marconi AM, Ronzoni S, Di Noio M, Fennessey PV, Pardi G, et al. Placental transport of leucine, phenylalanine, glycine, and praline in intrauterine growth-restricted pregnancies. Journal of Clinical Endocrinology & Metabolism 2001;86(11):5427e32. Brusati V, Regnault TRH, Battaglia FC, Meschia G. Placental uptake of glutamate in FGR ovine pregnancies. Journal of the Society for Gynecologic Investigation 2003;10(2):A277. Cetin I, Marconi AM, Bozzetti P, Sereni LP, Corbetta C, Pardi G, et al. Umbilical amino acid concentrations in appropriate and small for gestational age infants: a biochemical difference present in utero. American Journal of Obstetrics & Gynecology 1988;158(1):120e6. Cetin I, Corbetta C, Sereni LP, Marconi AM, Bozzetti P, Pardi G, et al. Umbilical amino acid concentrations in normal and growth- retarded fetuses sampled in utero by cordocentesis. American Journal of Obstetrics & Gynecology 1990;162(1):253e61. Economides DL, Nicolaides KH, Gahl WA, Bernardini I, Evans MI. Plasma amino acids in appropriate- and small-for-gestational-age fetuses. American Journal of Obstetrics and Gynecology 1989;161(5):1219e27. Anderson AH, Guyton TS, Meschia G, Battaglia FC, Wilkening RB. Fetal plasma amino acid changes during severe, prolonged fetal hypoxia in pregnant sheep [Abstract]. Second World Congress of Perinatal Medicine; 1993. Philipps AF, Dubin JW, Raye JR. Effect of endogenous insulin release on fetal alanine concentration and uptake. American Journal of Obstetrics and Gynecology 1981;139(1):22e6. Philipps AF, Rosenkrantz TS, Lemons JA, Knox I, Porte PJ, Raye JR. Insulin-induced alterations in amino acid metabolism in the fetal lamb. Journal of Developmental Physiology 1990;13(5):251e9. Regnault TRH, de Vrijer B, Battaglia FC, Meschia G, Wilkening RB. Relationship of transplacental oxygen gradient, fetal lactate concentration and amino acid uptake in fetal growth restriction. Journal of the Society for Gynecologic Investigation 2004;11(2):A823. Bondoli A, Magalini SI, Camaioni D, Gagliardi A, Barbi S. Amino acid distribution in guinea pig plasma, cerebrospinal fluid and brain tissue in acute experimental hypoxia. Resuscitation 1980;8(2):85e93. Schultz K, Soltesz G, Mestyan J. Metabolic responses to severe perinatal asphyxia in term newborn infants with particular reference to the changes in plasma free amino acids. Biology of the Neonate 1981; 39(3e4):185e90. S60 [70] Walker V, Gentry AJ, Green LR, Hanson MA, Bennet L. Effects of hypoxia on plasma amino acids of fetal sheep. Amino Acids 2000;18(2): 147e56. [71] Hay WWJ, Sparks JW, Wilkening RB, Battaglia FC, Meschia G. Fetal glucose uptake and utilisation as functions of maternal glucose concentration. American Journal of Physiology 1984;246(3 Pt 1): E237e42. [72] Hay WWJ, Meznarich HK. Effect of maternal glucose concentration on uteroplacental glucose concentration and transfer in pregnant sheep. Proceedings of the Society for Experimental Biology and Medicine 1989;190:63e9. [73] Teng C, Battaglia FC, Meschia G, Narkewicz MR, Wilkening RB. Fetal hepatic and umbilical uptakes of glucogenic substrates during a glucagonesomatostatin infusion. American Journal of Physiology. Endocrinology and Metabolism 2002;282(3):E542e50. [74] Cetin I, Fennessey PV, Quick Jr AN, Marconi AM, Meschia G, Battaglia FC, et al. Glycine turnover and oxidation and hepatic serine synthesis from glycine in fetal lambs. American Journal of Physiology 1991;260(3 Pt 1):E371e8. [75] Cetin I, Fennessey PV, Sparks JW, Meschia G, Battaglia FC. Fetal serine fluxes across fetal liver, hindlimb, and placenta in late gestation. American Journal of Physiology 1992;263(4 Pt 1):E786e93. [76] Moores RRJ, Vaughn PR, Battaglia FC, Fennessey PV, Wilkening RB, Meschia G. Glutamate metabolism in fetus and placenta of lategestation sheep. American Journal of Physiology 1994;267(1 Pt 2): R89e96. [77] Timmerman M, Teng C, Wilkening RB, Fennessey P, Battaglia FC, Meschia G. Effect of dexamethasone on fetal hepatic glutamineeglutamate exchange. American Journal of Physiology. Endocrinology and Metabolism 2000;278(5):E839e45. [78] Wilkening RB, Boyle DW, Teng C, Meschia G, Battaglia FC. Amino acid uptake by the fetal ovine hindlimb under normal and euglycemic hyperinsulinemic states. American Journal of Physiology 1994;266 (1 Pt 1):E72e8. [79] Ballard FJ, Filsell OH, Jarrett IG. Amino acid uptake and output by the sheep hind limb. Metabolism: Clinical and Experimental 1976;25(4): 415e8. [80] Moores RRJ, Rietberg CC, Battaglia FC, Fennessey PV, Meschia G. Metabolism and transport of maternal serine by the ovine placenta: glycine production and absence of serine transport into the fetus. Pediatric Research 1993;33(6):590e4. [81] Carver TD, Quick AA, Teng CC, Pike AW, Fennessey PV, Hay Jr WW. Leucine metabolism in chronically hypoglycemic hypoinsulinemic growth-restricted fetal sheep. American Journal of Physiology 1997; 272(1 Pt 1):E107e17. [82] Jefferson LS, Kimball SR. Amino acids as regulators of gene expression at the level of mRNA translation. The Journal of Nutrition 2003;133 (6 Suppl 1):2046Se51S. [83] Lawlor MA, Alessi DR. PKB/Akt: a key mediator of cell proliferation, survival and insulin responses? Journal of Cell Science 2001;114(Pt 16): 2903e10. [84] Bodine SC, Stitt TN, Gonzalez M, Kline WO, Stover GL, Bauerlein R, et al. Akt/mTOR pathway is a crucial regulator of skeletal muscle hypertrophy and can prevent muscle atrophy in vivo. Nature. Cell Biology 2001;3(11):1014e9. [85] Kim DH, Sarbassov DD, Ali SM, King JE, Latek RR, ErdjumentBromage H, et al. mTOR interacts with raptor to form a nutrientsensitive complex that signals to the cell growth machinery. Cell 2002; 110(2):163e75. [86] Rohde J, Heitman J, Cardenas ME. The TOR kinases link nutrient sensing to cell growth. Journal of Biological Chemistry 2001;276(13): 9583e6. [87] Shah OJ, Anthony JC, Kimball SR, Jefferson LS. 4E-BP1 and S6K1: translational integration sites for nutritional and hormonal information in muscle. American Journal of Physiology. Endocrinology Metabolism 2000;279(4):E715e29. [88] Lynch CJ, Patson BJ, Anthony J, Vaval A, Jefferson LS, Vary TC. Leucine is a direct-acting nutrient signal that regulates protein synthesis in adipose tissue. American Journal of Physiology. Endocrinology Metabolism 2002;283(3):E503e13. [89] Proud CG. Regulation of mammalian translation factors by nutrients. European Journal of Biochemistry 2002;269(22):5338e49. Placenta (2005), Vol. 26, Supplement A, Trophoblast Research, Vol. 19 [90] Cross DA, Alessi DR, Cohen P, Andjelkovich M, Hemmings BA. Inhibition of glycogen synthase kinase-3 by insulin mediated by protein kinase B. Nature 1995;378(6559):785e9. [91] Peyrollier K, Hajduch E, Blair AS, Hyde R, Hundal HS. L-Leucine availability regulates phosphatidylinositol 3-kinase, p70 S6 kinase and glycogen synthase kinase-3 activity in L6 muscle cells: evidence for the involvement of the mammalian target of rapamycin (mTOR) pathway in the L-leucine-induced up-regulation of system A amino acid transport. The Biochemical Journal 2000;350(Pt 2):361e8. [92] Dreiling CE, Carman FS, Brown DE. Maternal endocrine and fetal metabolic responses to heat stress. Journal of Dairy Science 1991;74: 312e27. [93] Terauchi Y, Tsuji Y, Satoh S, Minoura H, Murakami K, Okuno A, et al. Increased insulin sensitivity and hypoglycaemia in mice lacking the p85 alpha subunit of phosphoinositide 3-kinase. Nature Genetics 1999;21(2): 230e5. [94] Mauvais-Jarvis F, Ueki K, Fruman DA, Hirshman MF, Sakamoto K, Goodyear LJ, et al. Reduced expression of the murine p85alpha subunit of phosphoinositide 3-kinase improves insulin signaling and ameliorates diabetes. Journal of Clinical Investigation 2002;109(1):141e9. [95] Fingar DC, Salama S, Tsou C, Harlow E, Blenis J. Mammalian cell size is controlled by mTOR and its downstream targets S6K1 and 4EBP1/ eIF4E. Genes & Development 2002;16(12):1472e87. [96] Beck T, Hall MN. The TOR signalling pathway controls nuclear localization of nutrient-regulated transcription factors. Nature 1999; 402(6762):689e92. [97] Schmidt EV. The role of c-myc in cellular growth control. Oncogene 1999;18(19):2988e96. [98] Anthony JC, Yoshizawa F, Anthony TG, Vary TC, Jefferson LS, Kimball SR. Leucine stimulates translation initiation in skeletal muscle of postabsorptive rats via a rapamycin-sensitive pathway. The Journal of Nutrition 2000;130(10):2413e9. [99] Xu G, Kwon G, Cruz WS, Marshall CA, McDaniel ML. Metabolic regulation by leucine of translation initiation through the mTORsignaling pathway by pancreatic beta-cells. Diabetes 2001;50(2): 353e60. [100] Kimball SR, Jefferson LS. Regulation of global and specific mRNA translation by oral administration of branched-chain amino acids. Biochemical and Biophysical Research Communications 2004;313(2): 423e7. [101] Jozwik M, Teng C, Meschia G, Battaglia FC. Contribution of branchedchain amino acids to uteroplacental ammonia production in sheep. Biology of Reproduction 1999;61(3):792e6. [102] Loy GL, Quick ANJ, Hay WWJ, Meschia G, Battaglia FC, Fennessey PV. Fetoplacental deamination and decarboxylation of leucine. American Journal of Physiology 1990;259(4 Pt 1):E492e7. [103] Bolster DR, Crozier SJ, Kimball SR, Jefferson LS. AMP-activated protein kinase suppresses protein synthesis in rat skeletal muscle through down-regulated mammalian target of rapamycin (mTOR) signaling. Journal of Biological Chemistry 2002;277(27):23977e80. [104] Proud CG. The multifaceted role of mTOR in cellular stress responses. DNA Repair (Amst) 2004;3(8e9):927e34. [105] Tokunaga C, Yoshino K, Yonezawa K. mTOR integrates amino acidand energy-sensing pathways. Biochemical and Biophysical Research Communications 2004;313(2):443e6. [106] Horton LE, Bushell M, Barth-Baus D, Tilleray VJ, Clemens MJ, Hensold JO. p53 Activation results in rapid dephosphorylation of the eIF4E-binding protein 4E-BP1, inhibition of ribosomal protein S6 kinase and inhibition of translation initiation. Oncogene 2002;21(34):5325e34. [107] Cairns CA, White RJ. p53 is a general repressor of RNA polymerase III transcription. The EMBO Journal 1998;17(11):3112e23. [108] Pham TD, Maclennan NK, Chiu CT, Laksana GS, Hsu JL, Lane RH. Uteroplacental insufficiency increases apoptosis and alters p53 gene methylation in the full-term IUGR rat kidney. American Journal of Physiology. Regulatory Integrative and Comparative Physiology 2003; 285(5):R962e70. [109] Yamauchi H, Katayama K, Ueno M, Uetsuka K, Nakayama H, Doi K. Involvement of p53 in 1-beta-D-arabinofuranosylcytosine-induced trophoblastic cell apoptosis and impaired proliferation in rat placenta. Biology of Reproduction 2004;70(6):1762e7. [110] Levy R, Smith SD, Yusuf K, Huettner PC, Kraus FT, Sadovsky Y, et al. Trophoblast apoptosis from pregnancies complicated by fetal growth Regnault et al.: Fetoplacental Amino Acid Metabolism [111] [112] [113] [114] [115] [116] [117] [118] [119] [120] [121] [122] [123] [124] [125] [126] [127] [128] [129] [130] restriction in associated with enhanced p53 expression. American Journal of Obstetrics & Gynecology 2002;186(5):1056e61. Maclennan NK, James SJ, Melnyk S, Piroozi A, Jernigan S, Hsu JL, et al. Uteroplacental insufficiency alters DNA methylation, one-carbon metabolism, and histone acetylation in IUGR rats. Physiological Genomics 2004;18(1):43e50. Shihab FS, Andoh TF, Tanner AM, Yi H, Bennett WM. Expression of apoptosis regulatory genes in chronic cyclosporine nephrotoxicity favors apoptosis. Kidney International 1999;56(6):2147e59. Wu Y, Mehew JW, Heckman CA, Arcinas M, Boxer LM. Negative regulation of bcl-2 expression by p53 in hematopoietic cells. Oncogene 2001;20(2):240e51. Porter AG, Janicke RU. Emerging roles of caspase-3 in apoptosis. Cell Death and Differentiation 1999;6(2):99e104. Arsham AM, Howell JJ, Simon MC. A novel hypoxia-inducible factorindependent hypoxic response regulating mammalian target of rapamycin and its targets. Journal of Biological Chemistry 2003;278(32): 29655e60. Hatanaka T, Huang W, Wang H, Sugawara M, Prasad PD, Leibach FH, et al. Primary structure, functional characteristics and tissue expression pattern of human ATA2, a subtype of amino acid transport system A. Biochimica et Biophysica Acta 2000;1467(1):1e6. Hoeltzli SD, Smith CH. Alanine transport systems in isolated basal plasma membrane of human placenta. American Journal of Physiology 1989;256(3 Pt 1):C630e7. Johnson LW, Smith CH. Neutral amino acid transport systems of microvillous membrane of human placenta. American Journal of Physiology 1988;254(6 Pt 1):C773e80. Kudo Y, Yamada K, Fujiwara A, Kawasaki T. Characterization of amino acid transport systems in human placental brush-border membrane vesicles. Biochimica et Biophysica Acta 1987;904(2):309e18. Wang H, Huang W, Sugawara M, Devoe LD, Leibach FH, Prasad PD, et al. Cloning and functional expression of ATA1, a subtype of amino acid transporter A, from human placenta. Biochemical & Biophysical Research Communications 2000;273(3):1175e9. Nelson DM, Smith SD, Furesz TC, Sadovsky Y, Ganapathy V, Parvin CA, et al. Hypoxia reduces expression and function of system A amino acid transporters in cultured term human trophoblasts. American Journal of Physiology - Cell Physiology 2003;284(2):C310e5. Champion EE, Mann SJ, Glazier JD, Jones CJ, Rawlings JM, Sibley CP, et al. System B and System A Amino Acid Transporters in the Feline Endotheliochorial Placenta. American Journal of Physiology; Regulatory, Integrative and Comparative Physiology 2004; 287:R1369e79. Matthews JC, Beveridge MJ, Malandro MS, Kilberg MS, Novak DA. Response of placental amino acid transport to gestational age and intrauterine growth retardation. The Proceedings of the Nutrition Society 1998;57(2):257e63. Shafqat S, Tamarappoo BK, Kilberg MS, Puranam RS, McNamara JO, Guadano-Ferraz A, et al. Cloning and expression of a novel Na(+)dependent neutral amino acid transporter structurally related to mammalian Na+/glutamate contransporters. Journal of Biological Chemistry 1993;268(21):15351e5. Arriza JL, Kavanaugh MP, Fairman WA, Wu YN, Murdoch GH, North RA, et al. Cloning and expression of a human neutral amino acid transporter with structural similarity to the glutamate transporter gene family. Journal of Biological Chemistry 1993;268(21):15329e32. Carbo N, Lopez-Soriano FJ, Argiles JM. Neutral amino acid transport in placental plasma membrane vesicles in the late pregnant rat. Evidence for a B0-like transport system. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1997;71(1):85e90. Kekuda R, Prasad PD, Fei YJ, Torres-Zamorano V, Sinha S, YangFeng TL, et al. Cloning of the sodium-dependent, broad-scope, neutral amino acid transporter Bo from a human placental choriocarcinoma cell line. Journal of Biological Chemistry 1996;271(31):18657e61. Kudo Y, Boyd CA. Characterization of amino acid transport systems in human placental basal membrane vesicles. Biochimica et Biophysica Acta 1990;1021(2):169e74. Novak DA, Beveridge MJ. Glutamine transport in human and rat placenta. Placenta 1997;18(5e6):379e86. Feliubadalo L, Font M, Purroy J, Rousaud F, Estivill X, Nunes V, et al. Non-type I cystinuria caused by mutations in SLC7A9, encoding S61 [131] [132] [133] [134] [135] [136] [137] [138] [139] [140] [141] [142] [143] [144] [145] [146] [147] [148] [149] a subunit (bo, +AT) of rBAT. International Cystinuria Consortium. Nature Genetics 1999;23(1):52e7. Furesz TC, Smith CH. Identification of two leucine-sensitive lysine transport activities in human placental basal membrane. Placenta 1997; 18(8):649e55. Cariappa R, Heath-Monnig E, Smith CH. Isoforms of amino acid transporters in placental syncytiotrophoblast: plasma membrane localization and potential role in maternal/fetal transport. Placenta 2003; 24(7):713e26. Ganapathy ME, Leibach FH, Mahesh VB, Howard JC, Devoe LD, Ganapathy V, et al. Characterization of tryptophan transport in human placental brush-border membrane vesicles. The Biochemical Journal 1986;238(1):201e8. Kanai Y, Segawa H, Miyamoto K, Uchino H, Takeda E, Endou H. Expression cloning and characterization of a transporter for large neutral amino acids activated by the heavy chain of 4F2 antigen (CD98). Journal of Biological Chemistry 1998;273(37):23629e32. Kudo Y, Boyd CA. Characterisation of L-tryptophan transporters in human placenta: a comparison of brush border and basal membrane vesicles. Journal of Physiology 2001;531(Pt 2):405e16. Pineda M, Fernandez E, Torrents D, Estevez R, Lopez C, Camps M, et al. Identification of a membrane protein, LAT-2, that Co-expresses with 4F2 heavy chain, an L-type amino acid transport activity with broad specificity for small and large zwitterionic amino acids. Journal of Biological Chemistry 1999;274(28):19738e44. Ritchie JW, Taylor PM. Role of the System L permease LAT1 in amino acid and iodothyronine transport in placenta. The Biochemical Journal 2001;356(Pt 3):719e25. Eleno N, Deves R, Boyd CA. Membrane potential dependence of the kinetics of cationic amino acid transport systems in human placenta. Journal of Physiology 1994;479(Pt 2):291e300. Furesz TC, Moe AJ, Smith CH. Lysine uptake by human placental microvillous membrane: comparison of system yC with basal membrane. American Journal of Physiology 1995;268(3 Pt 1):C755e61. Kudo Y, Boyd CA. Heterodimeric amino acid transporters: expression of heavy but not light chains of CD98 correlates with induction of amino acid transport systems in human placental trophoblast. Journal of Physiology 2000;523(Pt 1):13e8. Pfeiffer R, Rossier G, Spindler B, Meier C, Kuhn L, Verrey F. Amino acid transport of yCL-type by heterodimers of 4F2hc/CD98 and members of the glycoprotein-associated amino acid transporter family. The EMBO Journal 1999;18(1):49e57. Torrents D, Estevez R, Pineda M, Fernandez E, Lloberas J, Shi YB, et al. Identification and characterization of a membrane protein (y+L amino acid transporter-1) that associates with 4F2hc to encode the amino acid transport activity y+L. A candidate gene for lysinuric protein intolerance. Journal of Biological Chemistry 1998;273(49): 32437e45. Furesz TC, Moe AJ, Smith CH. Two cationic amino acid transport systems in human placental basal plasma membranes. American Journal of Physiology 1991;261(2 Pt 1):C246e52. Kamath SG, Furesz TC, Way BA, Smith CH. Identification of three cationic amino acid transporters in placental trophoblast: cloning, expression, and characterization of hCAT-1. The Journal of Membrane Biology 1999;171(1):55e62. Furesz TC, Heath-Monnig E, Kamath SG, Smith CH. Lysine uptake by cloned hCAT-2B: comparison with hCAT-1 and with trophoblast surface membranes. The Journal of Membrane Biology 2002;189(1):27e33. Hoeltzli SD, Kelley LK, Moe AJ, Smith CH. Anionic amino acid transport systems in isolated basal plasma membrane of human placenta. American Journal of Physiology 1990;259(1 Pt 1):C47e55. Matthews JC, Beveridge MJ, Malandro MS, Rothstein JD, CampbellThompson M, Verlander JW, et al. Activity and protein localization of multiple glutamate transporters in gestation day 14 vs. day 20 rat placenta. American Journal of Physiology 1998;274(3 Pt 1):C603e14. Matthews JC, Beveridge MJ, Dialynas E, Bartke A, Kilberg MS, Novak DA. Placental anionic and cationic amino acid transporter expression in growth hormone overexpressing and null IGF-II or null IGF-I receptor mice. Placenta 1999;20(8):639e50. Moe AJ, Smith CH. Anionic amino acid uptake by microvillous membrane vesicles from human placenta. American Journal of Physiology 1989;257(5 Pt 1):C1005e11. S62 [150] Malandro MS, Beveridge MJ, Novak DA, Kilberg MS. Rat placental amino acid transport after protein-deprivation-induced intrauterine growth retardation. Biochemical Society Transactions 1996;24(3): 839e43. [151] Karl PI, Fisher SE. Taurine transport by microvillous membrane vesicles and the perfused cotyledon of the human placenta. American Journal of Physiology 1990;258(3 Pt 1):C443e51. Placenta (2005), Vol. 26, Supplement A, Trophoblast Research, Vol. 19 [152] Norberg S, Powell TL, Jansson T. Intrauterine growth restriction is associated with a reduced activity of placental taurine transporters. Pediatric Research 1998;44(2):233e8. [153] Ramamoorthy S, Leibach FH, Mahesh VB, Han H, Yang F, Blakely RD, et al. Functional characterization and chromosomal localization of a cloned taurine transporter from human placenta. Biochemical Journal 1994;300(Pt 3):893e900.