Oxygen Transport and Asphyxia AnS 536 Spring 2016
advertisement
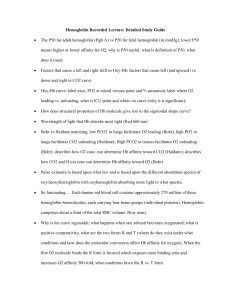
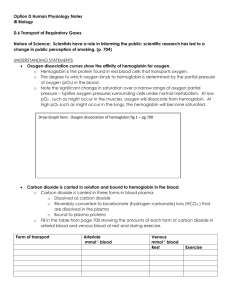
Oxygen Transport and Asphyxia AnS 536 Spring 2016 Goals To transport oxygen from maternal blood across the placenta to fetal blood, and after birth from the lungs to the blood stream To move oxygen from blood to tissues to allow aerobic metabolism (efficient production of ATP) To move carbon dioxide in the reverse direction Erythrocytes After maturation from stem cells in bone marrow, erythrocytes have a circulating life of ~120d Highly specialized cells: Cytoplasm contains ~35% solution of hemoglobin, but is devoid of subcellular organelles Cannot synthesize nucleic acids or proteins, limited lipid metabolism Carbohydrate metabolism devoted to maintaining functional pumps on cell membrane Erythrocytes After cell death, hemoglobin degraded and iron recycled to bone marrow As they pass through capillaries, cells deform into ellipsoidal, hemispheric, or teardrop shapes Cell fragility increased during newborn period Increased risk and incidence of hemolytic diseases Transport of Gases in Blood PO2 not only determines the dissolved oxygen content of blood, but also affects the amount of oxygen in reversible chemical combination with hemoglobin Chemical and physiological actions of gases depend on the partial pressures they exert in the gas phase and in solution in various body fluids Hemoglobin The binding of one molecule of O2 to Fe2+ increases the affinity of the other sites for oxygen binding (4 total) Carbon dioxide binds to the globulin portions of the molecule rather than to the iron molecules Accounts for about 10% of CO2 transport The sigmoidal shape of the oxygen dissociation curve is physiologically important Permits blood to deliver much more oxygen to tissues than a hyperbolic curve Hemoglobin Video Break OXYGEN BINDING VIDEO: http://www.dnatube.com/video/274/Hemoglobin-Oxygen-Binding OXYGEN TRANSPORT VIDEO: http://www.youtube.com/watch?feature=player_detailpage&v=WXOBJE XxNEo O2-Hb Dissociation Curve Illustrates a relationship between the partial pressure of oxygen (PO2) and percent saturated hemoglobin (Hb) Hemoglobin Increasing pH in RBC will increase the affinity of Hb for oxygen (in the lungs) When Hb binds to oxygen, it undergoes a conformational change that releases H ions from globin chains, decreasing pH in the cell In capillaries H+ generated by carbonic anhydrase activity in RBC decreases pH and facilitates oxygen delivery to tissues as well (high CO2 concentrations) Oxygen Loading and Unloading Bohr and Haldane Effects Bohr Effect Describes the influence of CO2 and pH on the release of O2 ↓ in pH (↑ in acidity) due to CO2 and hydrogen ions can combine reversibly with Hb at the sites other than the O2 binding sites (allosteric binding) Results in a structural change of Hb, reducing its affinity for O2 Haldane Effect Displacement of O2 from Hb increases affinity for CO2 and hydrogen ions Bohr and Haldane Effects Work together facilitating O2 liberation and the uptake of CO2 and hydrogen ions at the tissue level A Bohr or Haldane shift reduces Hb affinity for O2 Important in placental O2 transport pH is highest in veins where O2 is picked up (umbilical and placental arterioles) pH is lowest at arteries after CO2 and hydrogen ions have been picked up Changes in pH and CO2 on both maternal and fetal side of placenta regulate the rate of O2 transfer to a great extent Bohr and Haldane Effects Fetal pH is lower (more acidic) than maternal pH Fetal acidosis is metabolic and not related to the high PCO2 Primarily due to placentally produced lactate and pyruvate The effect of low pH on O2 delivery to tissues is often overlooked, but may be important in maintaining O2 delivery to tissues at an appropriate rate 2,3-Bisphosphoglycerate (2,3-BPG) Binds with greater affinity to Maternal deoxyhemoglobin Once it binds to first binding site, it allosterically affects other sites in hemoglobin to effectively increase the rate of release of oxygen at tissue level Right-shift of curve Fetal Hemoglobin (HbF) HbF has a higher affinity for O2 than HbA Two alpha-gamma dimers rather than two alpha-beta dimers Creates a LEFT shift in the dissociation curve much like the effect of ↑ pH, ↓ temperature, or ↓ 2,3 BPG ↑ affinity for O2 by Hb in the fetal blood enhances O2 transport across the placenta After birth HbF declines as neonates begin to manufacture new erythrocytes and HbA HbF binds 2,3-BPG poorly Hemoglobin Transitions Fetal Hemoglobin Fetal Hemoglobin Cytochrome P450 O2 is MUCH more soluble in lipids (like membranes) than in water (as in plasma or cytoplasm) Cytochrome P450 enhances transport processes due to its high affinity for O2 and accumulates along the endoplasmic reticulum (ER) of placental cells Many different varieties Most involve drug metabolism All incorporate oxygen into metabolic processes Tissues can up- or down-regulate the levels of this molecule to enhance O2 transport into cell Cytochrome P450 ER forms channels from the cell membrane to the mitochondria allowing O2 to move more freely throughout or across the cell Alignment of P450 along the ER channels creates a high affinity, O2 soluble freeway for O2 to travel P450 enhances transplacental O2 transport Studies have shown blocking P450 will decrease transplacental O2 flux by over 75% Fetal Gas Exchange CO2 diffuses across placenta primarily in molecular form - not as bicarbonate ion Fetal PCO2 is higher than maternal Fetal oxygen consumption is equivalent to adult values Placenta is designed to protect the fetus from inadequate or excessive oxygen availability Fetal Gas Exchange Cont… Fetal mechanisms for protection against oxygen radicals are poorly developed prior to birth Increased oxygen in fetal blood may have more adverse effects than beneficial effects Induction of superoxide dismutase is due to increased exposure to oxygen postnatally Questions?