Document 14366848
advertisement
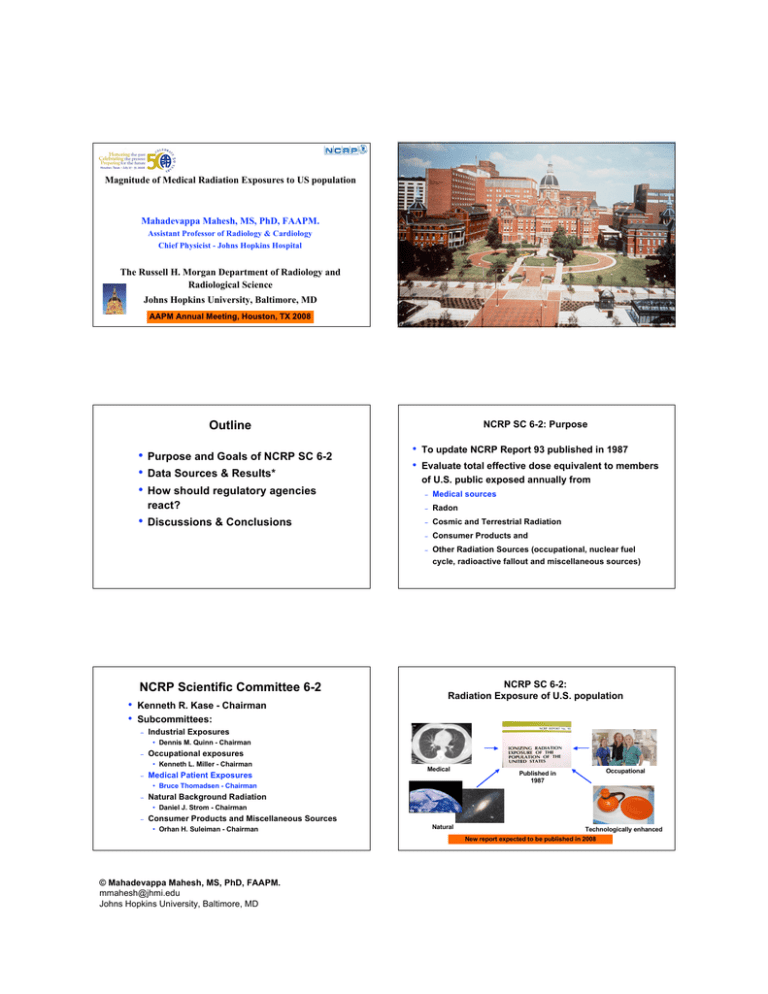
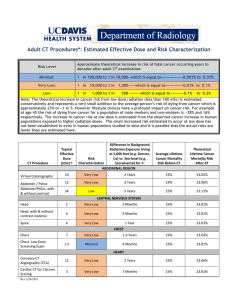
Magnitude of Medical Radiation Exposures to US population Mahadevappa Mahesh, MS, PhD, FAAPM. Assistant Professor of Radiology & Cardiology Chief Physicist - Johns Hopkins Hospital The Russell H. Morgan Department of Radiology and Radiological Science Johns Hopkins University, Baltimore, MD AAPM Annual Meeting, Houston, TX 2008 Outline • • • • Purpose and Goals of NCRP SC 6-2 Data Sources & Results* How should regulatory agencies react? Discussions & Conclusions NCRP Scientific Committee 6-2 • • Kenneth R. Kase - Chairman Subcommittees: − Industrial Exposures − Occupational exposures − Medical Patient Exposures NCRP SC 6-2: Purpose • • To update NCRP Report 93 published in 1987 Evaluate total effective dose equivalent to members of U.S. public exposed annually from − Medical sources − Radon − Cosmic and Terrestrial Radiation − Consumer Products and − Other Radiation Sources (occupational, nuclear fuel cycle, radioactive fallout and miscellaneous sources) NCRP SC 6-2: Radiation Exposure of U.S. population • Dennis M. Quinn - Chairman • Kenneth L. Miller - Chairman Medical • Bruce Thomadsen - Chairman − Natural Background Radiation − Consumer Products and Miscellaneous Sources Occupational Published in 1987 • Daniel J. Strom - Chairman • Orhan H. Suleiman - Chairman Natural Technologically enhanced New report expected to be published in 2008 © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD NCRP Report 93*: Annual effective dose equivalent to US population circa 1980-82 • Natural Sources − Radon 2.0 mSv − Other 1.0 mSv • Man-made Sources 1987 Natural 82% Man-made 18% 3.0 mSv • Medical − • Last major medical data used in NCRP Report No. 93 are from 1982 or earlier • 0.53 mSv • X-rays To update NCRP Report 93 published in 1987 and NCRP report 100 published in 1989 0.6 mSv Occupational, Consumer products, nuclear fuel cycle and other miscellaneous products 0.07 mSv − 1989 Purpose Evaluate the current total effective dose to members of U.S. public exposed annually from 0.39 mSv • Nuclear Medicine 0.14 mSv Medical Radiation Exposures * Published in 1987 NCRP SC 6-2: Medical Subgroup Members Chairperson: B. Thomadsen,University of Wisconsin • • • • • • • • • • Goals • Estimate current radiation exposure to US population M. Bhargavan American College of Radiology − Number and types of medical procedures D. Gilley State of Florida − Effective radiation dose per procedure J. Gray DIQUAD, LLC J. Lipoti State of New Jersey M. Mahesh Johns Hopkins University J. McCrohan US FDA − Radiography, Fluoroscopy, Mammography, Dental F. Mettler Univ of New Mexico VA − Interventional T. Yoshizumi Duke University − CT M. Rosenstein Scientific NCRP Consultant − Nuclear Medicine K. Kase Stanford SC 6-2 Chair − Radiation Therapy • • Examine past and future trends of medical exposures Modalities Assumptions Methods • Collective doses estimated independently for each modality • Modality groups: − • • report • CT, Nuclear medicine, Radiography & Fluoroscopy, Mammography, Interventional, Dental, Chiropractic Radiology, Bone Densitometry, and Radiation Therapy Procedures within each modality categorized by body part or organ system Benefit exceeds risk: Issue not examined in this Data sources: − Multiple data sets − Incomplete data sets required assumptions and cross checking between data sets • Weighting Factors: Used ICRP 60 (1990). Past reports used older ICRP 26 (1977) and new factors are suggested © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Modalities & procedures considered in the report • • • • • • • • Major and minor data sources Computed Tomography (CT) Nuclear Medicine Procedures Radiography and Fluoroscopy Interventional Radiography Mammography Dental and Chiropractic Bone Densitometry Radiation Therapy IMV Benchmark Reports • Based on responses from hospitals and estimated to identified universe of US hospitals (~7000) • • Surveys had high response rates (~60%) • • Reports used: CT, nuclear medicine, cardiac catheterization, radiography-fluoroscopy, angiography, mammography, PET and radiation therapy Reports between 2003-2006 • • • • • Procedure counts available for 1991-2006 Grouped by HCPCS-CPT, patient age and gender Summarized data for 2003-2006 used for comparisons 4 to 7 million enrollees, mostly male Women and children under-represented © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Commercial (IMV Benchmark) Medicare payment data (2003-2005) • • • • • • • • VA Health Care System Claims data from large national employer plan US FDA CRCPD State radiation programs Large hospitals American College of Radiology Literature Medicare Payment Data • • Claims data for Medicare fee-for-service enrollees Summarized procedure counts for each modality and sorted by Common Procedure Coding System (HCPCS) Common Procedural Terminology (CPT) code • • • • 100% medical claims from 1997-2004 Accounts for nearly 40 million enrollees Mainly covers persons >65 years old and disabled Represents one-third of all utilization and one-seventh of US population Data includes all ages Veterans Administration (VA) • • Large National Employer Program (LNEP) • • • • • Claims data available for 2003 Data summarized by modality and body part 4 millions nationally distributed All ages and gender included Data used for spot-check distributions of procedures for certain modalities Data: Reconciliations and Limitations • • Results Procedure counts and distribution from IMV reports Distribution of procedure counts across body part or organ system was matched with data from other data sources • Limited data available on volumes of chiropractic and dental imaging Computed Tomography (CT) • Annual growth over 1993-2006: − Computed Tomography Number of CT procedures in US IMV Benchmark Report on CT, 2006 © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD • • • CT Procedures > 10% vs US population < 1% Nearly 67 million CT procedures in US in 2006 Data correlated to nearly 7649 hospitals in US Pediatric CT ~ 8-10% of total procedures Categories of CT procedures (62.0 million in 2006) HCAP: ~80% of all CT procedures IMV 2006 Distribution Pattern of CT Scanners in US* CT scans of Abdomen and Pelvis Exam distribution vs US Population* ~ 20% of population >55 years, receives >55% of CT scans IMV 2006 * LNEP 2003 CT: Procedures vs Collective Dose Preliminary Results for CT (2006) Number (millions) % Collective dose Person Sv % Head 19.0 28 38,000 8.7 Chest 10.6 16 74,000 17.0 Abd/Pelvis 25.4 38 254,000 58.0 Extremity 3.5 5 500 0.1 CT Angiogram 4.3 6 56,000 12.8 Miscellaneous 4.2 6 15,000 3.4 TOTAL 67 84% 438,000 Preliminary results not yet reviewed and approved by NCRP Council Collective dose Effective dose per person from CT ~438,000 person Sv ~1.46 mSv Preliminary results not yet reviewed and approved by NCRP Council Radiation dose from CT: Then (1980) and Now (2006) • According to NCRP report 100 • According to current estimations − Collective dose for CT 3,700 person Sv − Collective dose for CT 440,000 person Sv − Effective dose per capita ~1.5 mSv and some radiation exposure © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Nuclear Medicine • Annual growth over 1993-2005: • Nearly 17 million nuclear medicine procedures in US − Nuclear Medicine in 2005 • • Data correlated to nearly 7200 hospitals in US Largest increases in cardiac procedures − Number of nuclear medicine procedures in US Nuclear Medicine Procedures > 5% vs US population < 1% 1% in 1973 to 57% in 2005 Type of Nuclear Medicine Procedures IMV 2005 IMV Benchmark Report on NM, 2005 Nuclear Medicine: Procedures vs Collective Dose Procedures by categories (%) Collective dose Effective dose per person Preliminary Results for Nuclear Medicine (2005) Collective dose by categories (%) ~231,000 person Sv ~0.80 mSv Preliminary results not yet reviewed and approved by NCRP Council © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Number millions % Collective dose Person Sv % Brain <0.1 <2 260 0.1 Thyroid < 0.1 <2 400 0.2 Lung 0.74 4 2,000 0.9 Cardiac 9.80 57 188,000 85.2 GI 1.21 7 3,500 1.6 Renal 0.47 3 650 0.3 Bone 3.45 20 20,500 9.3 Infection 0.38 2 1,300 0.6 Tumor 0.34 2 3,900 1.8 Total 17.2 220,500 Radiation doses from Nuclear Medicine: Then (1980) and Now (2006) • According to NCRP report 100 − • Collective dose for Nuclear Medicine 32,000 person Sv Radiography & Fluoroscopy According to current estimations − Collective dose for Nuclear Medicine − Effective dose per capita ~0.80 mSv 231,000 person Sv Radiography & Fluoroscopy Radiography: Procedures vs Collective Dose Procedures by categories (%) • Collective dose by categories (%) Data includes mammography, dental, chiropractic radiographic procedures, bone densitometry & certain fluoroscopy procedures • Limited data available for dental and chiropractic procedures Collective dose Effective dose per person from Radiography ~98,000 person Sv ~0.30 mSv Preliminary results not yet reviewed and approved by NCRP Council Radiation dose from conventional radiography and fluoroscopy: Then (1980) and Now (2006) • According to NCRP report 100 − • Collective dose 71,000 person Sv According to current estimations − Collective dose − Effective dose per capita 98,000 person Sv ~0.32 mSv © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Interventional Interventional Fluoroscopy • Preliminary Results for Interventional Procedures considered − − − • Procedures Number (millions) % Collective dose Person Sv % 10 12,900 10 Non-coronary angiography diagnostic and therapeutic procedures Non-coronary diagnostic 1.7 Cardiac catheterization procedures Non-coronary therapeutic 1.4 9 21,930 17 Cardiac catheterization 4.6 28 63,210 49 Other interventional fluoroscopy 9.0 53 30,960 24 TOTAL 16.7 Other interventional fluoroscopy procedures such as ERCP, Urinary studies, … Effective dose estimations varies by order of magnitude 129,000 Preliminary results not yet reviewed and approved by NCRP Council Interventional: Procedures vs Collective Dose Procedures by categories (%) Collective dose by categories (%) Radiation Therapy Collective dose Effective dose per person ~129,000 person Sv ~0.4 mSv Preliminary results not yet reviewed and approved by NCRP Council Radiation Therapy • Different source of exposure to population than other medical exposures • Form of risks are different from diagnostic applications • • − Concern for failure of function of target organ due to high dose − Likelihood of secondary cancer Even though data on number of radiation therapy procedures are available, the dose delivered varies widely and often unknown Uncertainty in estimating an average dose is very high, therefore not included in final estimation of radiation exposure to US population Preliminary Results* Number Procedures % Collective dose (Person-Sv) % Per capita (mSv) CT 67 million 16 440,000 49 1.50 Nuclear Medicine 18 million 4 231,000 26 0.80 Radiography & Fluoroscopy 324 million 76 99,000 11 0.30 Interventional 17 million 4 129,000 14 0.40 Modalities Total ~426 million 899,000 ~3.0 *NCRP SC 6-2 © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Procedures vs Effective dose contributions Radiation dose from Medical Exposure: Then (1980) and Now (2006) • • Percent Procedures Effective Dose Contributions Effective dose per capita from medical radiation exposure is ~ 3.0 mSv * Includes mammography & dental procedures According to NCRP report 93 − Collective dose 123,000 person Sv − Effective dose 0.54 mSv per capita According to current estimations − Collective dose 899,000 person Sv − Effective dose 3.0 mSv per capita Results not yet reviewed and approved by NCRP Council NCRP SC 6-2 Preliminary Results*: Medical Radiation Exposure to US population Per capita radiation dose has increased ~ 500% Radiation exposure to US population from all sources The new pie chart! US 1982 (NCRP 93) x 5.5 = 3.0mSv 3.2 mSv 0.54 mSv 1980 CT contribution ~1.5 mSv Medical 0.54 mSv per capita Total 3.6 mSv per capita 2006 * These results have not been reviewed and approved by Council Not to be disseminated or referenced Discussions • Results are snapshots, however, provides insight regarding current and future trends • Doses for procedures are averages and individual doses may vary by a factor of 3-20 • US 2006 Final report expected in 2008 © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Medical 3.0 mSv per capita Total 6.25 mSv per capita These results have not been reviewed and approved by NCRP Council Not to be disseminated or referenced Probable causes for increase in medical exposures • • • Advances in medical technology • Easy to use - • Accessibility • Economics in medical imaging Demand of improved patient care Challenges in early diagnosis − − − Demand for improved temporal and spatial resolution Out of the box solution, for ex: CT Emergency Rooms - Outpatient - Doctor’s offices - … Benefits from Medical Imaging • • Benefits outweighs the risks! Early diagnosis have led to − Increase in life expectancy − Decrease in deaths due to cancers, cardiovascular and other What should we do? • Aware of risks of radiation when ordering x-ray based examinations • Essential to use most accurate information when making risk benefit decisions • Often risks are either underestimated or massively overestimated • Well-informed investigative decisions are key! diseases • Decreases in childhood mortality - not only in US but globally - due to early diagnosis Are more regulations required – Yes & No • Yes, Appropriate regulations are required to hinder/stop misuse of medical x-ray technology • Yes, appropriate regulations are required to ensure x-ray technology is operated at optimal settings with proper QA in place and only qualified individuals operates/uses the technology • No, should not curb the development of new technology or protocols or stop clinicians from finding new ways to better care for their patients What can we do? • Examine radiation doses for different procedures • Identify and optimize factors contributing towards radiation doses • Image quality should not be jeopardized when reducing dose • Management of radiation dose is key! Effective doses in CT procedures* Computed Tomography * Mettler, Huda, Yoshizumi and Mahesh, Radiology, July 2008 © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Many patients have more than one CT examination Sinus CT in Post Bone Marrow Transplant Pediatric Patients 2002 Table 1: Number of CT scans performed for various age groups along with the average and range of effective dose estimation. 2003 No. of CT scans Age group 2004 2004 2005 Radiation Dose Report for a CTA Procedure 18.4 9.8 39.2 2 to 5 19 3.8 2 13 16.9 8.8 57.2 6 to 10 10 3.4 2 6 11.2 6.6 19.8 11 to 15 15 3.1 2 7 7.8 5 17.5 16 and above 16 3 2 6 6.6 4.4 13.2 Optimize CT settings − − • 1.0 mSv • • 18.3 mSv 21.7 mSv General Implications − For example, digital vs screen-film mammography, 64 vs 4 MDCT − As scan time becomes shorter, and more information can be gathered per visit, tendency is to add more exams per visit − A chest x-ray may be followed by a chest CT scan and chest CT scan may further include with and without contrast scans − Similarly, CT Angiography may be followed by CT Perfusion • ‘How many of the medical exams are appropriate?’ © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Maximum 8 Recommendations to reduce radiation risk from CT 2.4 mSv • However, number of exams performed per patient visit seems to increase • For example: Average Minimum 2 − exam can decrease Effective dose (mSv) Maximum 3.8 • • Advances in technology leads to increase in protocols • With technological advances and optimization, often radiation exposure per Average Minimum 4 Effective dose (mSv) Total effective dose (mSv) No of patients 0 to 1 Reduce tube current (mA) Use dose modulation techniques Increase pitch Reduce number of multiple scans with contrast material Eliminate inappropriate referrals for CT Adopt Image Gently Campaign for lowering dose What can we do? • Is educating public regarding radiation exposures better? YES • • ‘Web’ - can be a useful tool or a distracting tool • Often when patients ask about their medical exposures, clinic pays special attention regarding their protocol settings Delicate balance necessary - educating versus scaring population about radiation exposures Conclusions • Advances in medical technology, clinical applications, proliferation of imaging systems and easiness to use and many other factors have contributed to the overall increase in medical radiation exposure • Justify appropriateness of x-ray imaging procedure • Understanding associated radiation dose and risks are essential to obtain optimal benefit Conclusions • Overall, medical radiation exposure to US population has increased significantly from last report • Advances in medical technology, clinical applications, proliferation of imaging systems and easiness to use and many other factors have contributed to the overall increase in medical radiation exposure to US population © Mahadevappa Mahesh, MS, PhD, FAAPM. mmahesh@jhmi.edu Johns Hopkins University, Baltimore, MD Conclusions • Results are snap-shot of radiation exposure to US population from various medical procedures • Doses for procedures are averages and individual doses may vary by a factor of 3-20 • Benefit exceeds risk - however, this issue is not examined in this report • Final report is expected in 2008 Slice Wars! Dose Wars! Past – Present - Future