Preconditioning and the Developing Brain Carina Mallard, PhD,
advertisement

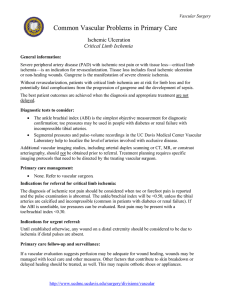
Preconditioning and the Developing Brain Henrik Hagberg, MD, PhD,* Olaf Dammann, MD, MSc,† Carina Mallard, PhD,‡ and Alan Leviton, MD, PhD§ Preconditioning occurs when a subinjurious exposure renders the brain less vulnerable to a subsequent damaging exposure. In this essay, various models of preconditioning in the immature brain are discussed. Adenosine, excitatory amino acids, nitric oxide, hypoxia-inducible factor, ATP-sensitive Kⴙ channels, caspases, heat shock proteins, inflammatory mediators and gene expression all seem to be involved in sensing, transducing and executing preconditioning resistance. Also reviewed in this essay is evidence that some subinjurious exposures render the brain more vulnerable to a subsequent damaging exposure. We believe that unraveling the mechanisms of how the developing brain becomes inherently resilient or vulnerable will offer important insights into the pathogenesis of injury. Preconditioning of the brain or induction of tolerance of the immune system might be utilized in the future to decrease CNS vulnerability and the occurrence of perinatal brain injury. Semin Perinatol 28:389-395 © 2004 Elsevier Inc. All rights reserved. I n light of recent advances in the field of preconditioning (PC), we consider it appropriate to review this area of research. Elucidating the endogenous mechanisms involved in PC might provide information that can guide us to a better understanding of the critical events leading to brain injury. This, in turn, would help us design prophylactic and therapeutic interventions. Because our major goal is to find ways to protect the developing brain, we have emphasized PC effects in the immature central nervous system. Background and Definition In a seminal paper published in 1986, Murray and his colleagues reported that the extent of myocardial infarction resulting from a sustained coronary occlusion was diminished if the heart had been subjected previously to brief periods of sublethal ischemia.1 This modulation of a response to an otherwise lethal exposure by a preceding *Department of Obstetrics and Gynecology, Institute of Women’s and Children’s Health, Göteborg University, Göteborg. †Perinatal Infectious Disease Epidemiology Unit, Department of Obstetrics, Prenatal Medicine, and General Gynecology, Department of Pediatric Pneumology and Neonatology, Hannover Medical School, Hannover. ‡Department of Physiology and Pharmacology, Göteborg University, Göteborg. §Neuroepidemiology Unit, Children’s Hospital, Boston, MA. Address reprint requests to: Professor Henrik Hagberg, Perinatal Center, Department of Obstetrics and Gynecology, Sahlgrenska University Hospital, Göteborg University, Göteborg, Sweden 416 85. E-mail: henrik.hagberg@obgyn.gu.se 0146-0005/04/$-see front matter © 2004 Elsevier Inc. All rights reserved. doi:10.1053/j.semperi.2004.10.006 sublethal exposure defines PC. Similar PC effects on the heart have been observed in humans.2,3 One report suggests that transient ischemic attacks (TIA) induce ischemic PC in the brain.4 PC, also sometimes known as tolerance, occurs in a number of organs, can be induced by different sublethal insults, and can occur at remote sites. For example, ischemia in one cerebral hemisphere can induce tolerance in both hemispheres to subsequent forebrain ischemia.5 Moreover, this concept of “remote PC” can be extended to include PC of one organ protecting another organ.6 This suggests that a circulating substance is involved in communicating the PC message to other organs. Although early studies used the same PC exposure as the potentially toxic exposure, subsequent studies documented that PC to a toxic exposure could be achieved with exposure to subtoxic levels of a different exposure, so called cross-tolerance.7,8 Usually PC means that a prior sublethal exposure renders the tissue less sensitive to the severe insult. In this sense, PC protects the organ. Some recent studies, however, have demonstrated that a sublethal exposure (eg, to lipopolysaccharide or “in vitro ischemia”) increases vulnerability to further insults.9 In this sense, PC, or perhaps more appropriately, “negative PC,” is a sensitizing factor (Fig. 1). Here we limit the expression PC to illustrate the reduction in the brain’s vulnerability made possible by a previous subthreshold exposure (chemicals, toxins, hypoxia, epilepsy, cytokines or any other exposure). We use the term sensitization to describe a situation where the brain is rendered more vulnerable by a previous subthreshold exposure. 389 390 H. Hagberg et al. the vulnerability of the cell or tissue. Single factors can sometimes act both as a sensor and part of the cellular signal transduction/effector system (eg, HIF-1, caspases and nitric oxide). Adenosine PC stimuli (eg, hypoxia or ischemia) disturb the energy balance resulting in an accumulation of adenosine. The subsequent activation of adenosine A1 receptors seems to be a critical early step in tolerance. A1 receptor antagonists inhibit PC protection in a number of tissues, including the adult CNS.19,20 The role of adenosine A1 receptors has not been explored in PC models of immature animals and may actually be less critical as A1 receptors do not appear to function during the neonatal period.21 Figure 1 The interaction between a sub-threshold insult and a severe insult may result in decreased brain injury, so called preconditioning. In contrast, the term sensitization describes a situation where the brain is rendered more vulnerable by a previous sub-threshold exposure. (Color version of figure is available online.) Cellular Biology of Preconditioning in the Brain Models of PC in Immature Animals A number of different insults can induce PC in adult animals, including hypoxia, ischemia, inflammatory cytokines, endotoxin, spreading depression, seizures, excitotoxins, hyperthermia and mitochondrial toxins. Usually, a certain time period (typically 12-72 hours) between PC and the severe insult is required to achieve tolerance. For example, induction of hyperthermia (41.5-42°C for 15 minutes) 6 to 24 hours before hypoxia–ischemia conferred a considerable reduction of brain injury in postnatal day 7 rats.10,11 Longer lasting protection is suggested by the observation that transient (30 minute) intrauterine ischemia 12 days before an hypoxic–ischemic insult on postnatal day 7 still increased neuronal survival from 44% to 74%.12 On the other hand, the salutary effects of PC are partly lost when the interval between the threshold exposure and evaluation is prolonged (eg, weeks), especially in young animals.13,14 Although no study has demonstrated that the benefits of PC are permanent, they do seem to last for weeks, if not months. In immature rats, 3 hours of exposure to 8% oxygen, 24 hours before a prolonged hypoxic–ischemic insult, reduces brain injury by 70 to 90%,15,16 which persists up to 3 weeks.17 Indeed, we recently found that the structural damage and the functional deficits following the severe insult were still markedly (by 72%) reduced after 8 weeks of recovery in the PC compared with the sham control group.18 Mechanisms of PC Acquisition of tolerance appears to depend on stress sensors, signal transduction and effectors of protection (Fig. 2). Stress sensors (or proximal triggers) detect various stressful conditions and convert the information into an intracellular stress response. The signal is thereafter processed through the signal transduction system, activating various effector systems that will reduce Glutamate Glutamate is also released in response to PC insults, leading to activation of both N-methyl-D-aspartate (NMDA) and alphaamino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors. Indeed, PC can be induced by administration of glutamate receptor agonists. NMDA receptor antagonists block tolerance in the adult brain,22,23 but not in the immature brain.17 Preconditioning might also prevent the downregulation of GluR2 AMPA type of receptors, which would decrease intracellular calcium overload.24 In the immature white matter, the situation appears to be quite the opposite, as sublethal exposure to oxygen– glucose deprivation down-regulates GluR2 receptors, increases Ca2⫹ uptake and increases the vulnerability of oligodendroglial precursor cells.9 This is an example of the sensitization (“negative PC”) we refer to above. Nitric Oxide (NO) NO may be involved in hypoxic PC in the immature brain. In one study of 7-day-old rats, the nonspecific NOS inhibitor L-nitroarginine almost completely inhibited PC protection.16 Specific inhibitors of the neuronal and inducible isoforms of NOS, however, had no effect on the PC response, indicating the importance of endothelial NOS (eNOS). Hypoxia Inducible Factor 1 (HIF-1) HIF-1 is a heterodimeric transcription factor composed of HIF-1, which is constitutively expressed, and HIF-1␣, which is tightly regulated by the oxygen concentration.25 Consequently, HIF-1␣, is rapidly induced by hypoxia in the neonatal brain26 and may thereby serve as a stress sensor. HIF-1 may actually also function as an effector to promote cell survival by inducing genes that contain a hypoxia response element that includes binding sites for HIF-1.27 Indeed, hypoxic PC induces the expression of a number of HIF-1 target proteins (or mRNAs) like glucose transporter 1, aldolase, phosphofructokinase, lactate dehydrogenase, erythropoietin and vascular endothelial growth factor28,29 that may make the brain resistant to further insults.30,31 Both desferrioxamine and CoCl2, each known to protect the immature brain (see below), also induce HIF-1␣ expression.26 However, HIF-1 target genes expressed after hypoxia were not induced by CoCl228 and there is currently no direct evidence yet that HIF-1 is responsible for PC protection in the immature brain. Preconditioning and the developing brain 391 Preconditioning insults hypoxia, ischemia, proinflammatory cytokines, endotoxins, spreading depression, seizures, excitotoxins, hyperthermia, mitochondrial toxins Stress sensors ATP-sensitive K-channels; NMDA receptors (?), i.c. Ca2+, NO, adenosine A1 receptors (?), oxygen free radicals; activation of caspase-3; Heat shock proteins; Signal transduction Kinases Transcription factors PKC NFkB Raf-1, P42/p44(Erks), p38, p21ras, MEKs, JNK/SAP ceramide Jak-2 HIF-1a CREB Effectors of protection Altered synthesis of proteins or posttranslational modification hypoxia-inducible factor ATP sensitive K channels (mitochondria) HIF-1a target genes preservation of mitochondrial function heat shock protein 72 & 27 Erythropoietin Bcl-2-family of proteins 12-lipoxygenase heme oxygenase-1 eNOS MnSOD metallothionein-1 and-2 MKP-1 block of GluR2 (?) Figure 2 Acquisition of tolerance depends on stress sensors, signal transduction and effectors of protection. Stress sensors detect various stressful conditions and convert the information into an intracellular stress response. The signal is thereafter processed through the signal transduction system, activating various effector systems that will reduce the vulnerability of the cell or tissue. ATP-Sensitive Kⴙ Channels, Caspases and Heat Shock Proteins ATP-sensitive K⫹ channels, which may be important at the signal transduction/effector level, can be activated by adenosine A1 receptors, oxygen free radicals and through a complicated kinase cascade involving both the protein kinase C family and mitogen-activated protein kinases.20 Channel blockers inhibit PC and channel openers can induce tolerance in many systems.19,20 The mechanisms are partly unresolved, but activation of these channels in the plasma membrane leads to hyperpolarization that may prevent or delay deleterious depolarizations. Alternatively, opening of ATP-sensitive K⫹ channels in mitochondria may dissipate the potential across the inner membrane that would prevent wasteful ATP-hydrolysis or increase mitochondrial buffering of cytosolic Ca2⫹.20 Another possibility is that opening of ATP-sensitive K⫹ channels leads to a limited release of mitochondrial cytochrome C and activation of caspase-3, which will turn on compensatory systems like the heat shock proteins (HSPs). HSPs are intracellular molecular chaperones of naive, aberrantly folded or mutated proteins, but they also prevent the assembly of the apoptosome and inactivate caspase-3.32,33 Such a sequence of events may be relevant for the immature brain because administration of an ATP sensitive K⫹ channel opener (diazoxide) protects against hypoxia–ischemia,34 heat shock protein 72 is induced in response to stimuli that promote PC10 and caspases play a key role in immature cell injury.35-37 Preconditioning-induced activation of caspase-3 may also cleave and inactivate poly(ADP-ribose)polymerase-1 (PARP-1), which would add to the tolerant state as activation of PARP-1 enhances brain injury also in the immature brain.38,39 Preconditioning and Gene Expression In most cases a certain time lag (typically 12-72 hours) is required between the PC stimulus and the severe insult to obtain PC protection (at least for the brain). This has led to the inference that protein synthesis is needed for PC. This inference is supported by the observation that the protein synthesis inhibitor cycloheximide inhibits ischemic PC40 and by the evidence that proteins play an important role in PC (including such transcription factors as HIF-1, nuclear factor kappa B (NF-kB), ceramide, activator protein-1, early growth response gene-1 and cAMP response element-binding protein).41,42 392 A number of these genes/proteins, besides HIF-1 target genes and heat shock proteins, are expressed after PC. Based on their specific properties, some of them may be anticipated to act as intermediates between the PC stimulus and the observed protection. For example, metallothionein-1 and -2 are expressed in the immature brain after hypoxic PC29 and even though the functions of these proteins are unknown, they are protective in models of ischemia.43 Furthermore, MAP-kinase phosphate-1 (MKP-1) mRNA, which is induced after hypoxia,29 improves survival by antagonizing c-Jun Nterminal kinase (JNK) activation, a contributor to CNS injury.44 A considerable number of other genes are also induced by the PC process (eg, lipoxgenases, cytokines, chemokines, etc). With the increased availability of micro-arrays, we expect that more will be identified. Vascular Effects: Cerebral Blood Flow Although some PC-related phenomena10,29,45 lead to the inference that improved cerebral blood flow accounts for some of the PC effects, studies in the adult CNS have shown that PC does not affect cerebral blood flow during or after ischemia.40,46,47 In addition, the fact that PC can be induced in vitro provides additional support for the view that factors unrelated to blood flow are at play. No studies have been published on PC and cerebral blood flow in the immature brain. However, in an immature (6-day-old) rat model of 2.5 hours of systemic hypoxia followed 24 hours later by the same systemic hypoxia accompanied by unilateral common carotid artery ligation, the rate of energy failure was significantly delayed in PC rats compared with that seen in rats exposed to hypoxia–ischemia alone.48 These results suggest an effect on cerebral blood flow or a direct effect on energy metabolism. Cytokines Under certain circumstances pro-inflammatory cytokines afford protection against cerebral ischemia.49 Both IL-1 and TNF-␣ are up-regulated following sublethal ischemia in vivo.50,51 Ischemic preconditioning appears to be dependent on TNF-␣ release as inhibition of TNF-␣ convertase (TACE/ ADAM17, which is involved in TNF-␣ release), blocked both the increase in TNF-␣ and the neuroprotective effects of preconditioning.51 Pretreatment of hippocampal cell cultures with TNF-␣ induces protection against subsequent oxidative insults such as FeSO4 or amyloid b-peptide exposure.52 TNF-␣ pretreatment also protects against focal cerebral ischemia in mice, however, only when given intracisternally.53 Furthermore, both TNF-␣ and IL-1 protect neurons in culture against subsequent hypoxic or excitotoxic injury.54,55 In the adult gerbil, repeated administration of IL-1 over several days protects hippocampal neurons from subsequent ischemic injury, an effect that is blocked by coadministering of IL-1 receptor antagonist (IL-1ra).56 In neuron cultures, the protective effects of TNF-␣ appear to reflect activation of NF-kB with subsequent induction of manganese superoxide dismutase (Mn-SOD) and suppression of both peroxynitrite formation and apoptosis.52,57 Nuclear translocation of NF-kB plays a central role following several PC stimuli as inhibition of NF-kB activation abolishes the preconditioning effects of sublethal ischemia, as well as H. Hagberg et al. epileptic and polyunsaturated fatty acid insults.58 In astrocyte cultures, TNF-␣-induced tolerance is associated with the inhibition of the phosphorylation of the NF-kB subunit, p65/ RelA, resulting in suppression of the ICAM-1 gene, while other NF-kB dependent genes such as Mn-SOD are not affected.59 These results therefore suggest that cytokine-induced tolerance is associated with different mechanisms in different cell types. Other possible down-stream beneficial effect of the induction of TNF-␣ and IL-1 is the production of neurotrophins, which are markedly induced by pro-inflammatory cytokines55,60,61 and by PC.62 In support of neurotrophins as PC intermediaries, is the observation that intracerebral administration of BDNF for 7, 10 or 14 days before ischemia reduces infarction volume, without affecting CBF.63 BDNF may exert its PC effects via crosstalk between the TrkB receptor and the NMDA receptor.64 Thus, under certain circumstances and at relatively low levels, pro-inflammatory cytokines appear to participate in a physiologic stress response that contributes to the development of tolerance in adult animals and in vitro. The role of cytokines in PC in the immature brain is complex and still unclear. Cytokines play important roles in the developing brain, are easily induced following ischemia, and might contribute to damage. We await evidence that cytokines and neurotrophins are involved in PC in the immature brain. Lipopolysaccharide (LPS) In the adult, the endotoxin LPS and the endotoxin analog diphoporyl lipid A confer tolerance to cerebral ischemia.65,66 LPS priming that increases tolerance against focal cerebral ischemia could be due to its stimulation of cytokines, such as TNF-␣ expression.67 Furthermore, ceramide, a down stream messenger of TNF-␣ signaling, contributes to LPS-induced tolerance to cerebral ischemia.68 PC induced by LPS is also associated with the induction of TGF-1, which has neuroprotective properties.69 LPS pretreatment does not appear to affect the cerebral blood flow immediately after MCA occlusion, but may diminish the severity of secondary microvascular perfusion deficits.70,71 In support of this concept, endothelial NOS is up-regulated following LPS and administration of the NOS inhibitor L-NAME abolishes the preconditioning effects of LPS.72 Other studies suggest that up-regulation of antioxidants (superoxide dismutase) following low doses of endotoxin may be important in LPS-induced tolerance.73,74 To our knowledge, endotoxin-induced PC has not been studied in the immature brain. We have recently found that LPS sensitizes the immature rat brain.75 Repeated daily doses of LPS, in utero, have been shown to induce cardiovascular tolerance but without cerebral protection in the fetal sheep.76 These observations suggest that effects of LPS priming may be variable depending on the physiological state, the presence of certain risk factors for vascular injury and age. Preconditioning and the developing brain Brain Injury Protection Analogies to PC Chemical Protection Some chemicals that protect the immature brain might do so by means other than those that characterize PC. Thus, we are not yet prepared to consider glucocorticoids, desferrioxamine and cobalt chloride as “chemical” preconditioners. Nevertheless, some of the similarities deserve attention. For example, glucocorticoids do not provide brain protection against hypoxia/ischemia if given immediately prior, during or after the insult in immature77 or adult78,79 animals. However, if dexamethasone, is given 4 to 24 hours before hypoxia–ischemia, brain injury is prevented in 1 to 2 weeks old, but not in 4-week-old pups80,81 demonstrating that not only the interval between the protector and the insult can be critical but also the age of the animals. The relatively long halflife of glucocorticoids would allow their effects to be exerted in the brain for days after administration and their presence might therefore contribute to a direct protective effect.82 Thus, a PC like mechanism needs not to be invoked, although it remains a possibility. As previously mentioned, HSPs are seen as protectors of the cell after exposure to stressful stimuli and may have a role in PC. The primary mediator of the heat shock response is the heat shock transcription factor 1 (HSF1). When HSF1 binds to one of the HSPs, a conformational switch occurs that rapidly activates HSF1 in a manner that mimics the kinetics of glucocorticoid receptor pathways mediated by cochaperones.83,84 Thus, steroid receptor function might be analogous to some phenomena presumed to be similar to some PC processes. Other examples of “chemical” preconditioners in immature animals are desferrioxamine and CoCl2. Giving either of these substances 24 hours before hypoxia–ischemia in 7-dayold rats reduces brain injury by more than 50%.26 Desferrioxamine has a half-life of only 3 hours in the rat.85 Thus, it is unlikely that enough desferrioxamine is available, in the brain, 24 hours later when the rat is exposed to the insult. The inference is that desferrioxamine has changed something that might be an approximation of what occurs with PC. Until the mechanisms of action are known, it is difficult to separate a PC effect of these agents from alternative explanations for brain protection. Immunization Immunization is defined as the induction of an immune response that is beneficial to the host in halting a pathological process.86 The earliest, and most current, immunizations promote the organisms’ ability to respond vigorously to an infectious organism (eg, H influenza). When an inflammatory response is damaging, however, the goal should be to turn down the ability to respond vigorously to a stimulus. Progress has been made recently in efforts to induce tolerance to CNS components, thereby promoting the development of regulatory/suppressor cells that modulate subsequent potentially damaging inflammatory phenomena. Antigen(s) can be injected, although risk of adversities may 393 be heightened.86 An alternative approach exposes the animal or person to the antigen(s) via the nose or mouth.87 Nasaland gut-associated lymphoid tissues are thought to have evolved to prevent the host from reacting to inhaled or ingested proteins that are nonpathogenic.88 T cells in the nose and bowel can be made tolerant with a low-dose regimen of a CNS antigen. For multiple sclerosis, the preferred antigens have been synthetic polypeptides whose components are present in myelin basic protein.89 For Alzheimer disease, the antigen has been amyloid-beta (A) protein.90 In animals studies intended to reduce infarct size, the antigens have been myelin basic protein,91 ovalbumin,91 and selectin.88 These tolerized cells become a form of regulatory T cell called Tr3 cells, which secrete cytokines such as IL-10 and transforming growth factor-1 on antigen restimulation. These Tr3 cells thereby modulate the brain-damaging inflammatory response by “active cellular regulation” or “bystander suppression.”92 PC-induced tolerance differs considerably from immunization-induced tolerance. Nevertheless, they can be viewed as analogous, at least in that both are prophylactic procedures intended to diminish the effects of insults that would otherwise lead to brain cell death. We offer this detail about immunizationinduced tolerance because it is a possible alternative to PC or a supplemental therapeutic approach. This alternative/supplement might be especially attractive if circulating inflammatory cells are shown to adversely affect the immature brain.93 Concluding Remarks Although PC does occur in the immature brain, very few investigators have addressed this topic. The complexity of PC needs to be much better understood before PC is considered a viable prophylactic approach to prevent brain damage in the newborn. For example, the possibility exists that a PC stimulus intended to protect the brain might instead sensitize the brain to an insult. On the other hand, the potential for PC to reduce the occurrence/severity of brain damage in the most vulnerable humans is sufficient reason to explore this topic in greater detail. Perhaps chemical preconditioners can be found that do not have this sensitizing capability. Other possibilities to protect the brain may be to induce tolerance in circulating inflammatory cells as activation of these are known to adversely affect the immature brain. Might such immuno-modulating interventions help to minimize perinatal brain damage in the future? Acknowledgments This work was supported by the Swedish Medical Research Council (09455 and K2004-33X-14185-03A), the Åhlén Foundation, the Sven Jerring Foundation, the Magnus Bergvall Foundation, the Wilhelm and Martina Lundgren Foundation, the Linnéa and Josef Carlsson Foundation, the Frimurare Barnhus Foundation, Göteborg Medical Society, Åke Wibergs Foundation, Wilhelm-Hirte Stiftung, Hannover Medical School, a cooperative agreement with the National Institutes of Health of the United States (NS40069) and by grants to researchers in the public health service from the Swedish government. H. Hagberg et al. 394 References 1. Murray CE, Jennings RB, Reimer KA: Preconditioning with ischemia: A delay of lethal cell injury in ischemic myocardium. Circulation 74: 1124-1136, 1986 2. Tomai F, Crea F, Chiariello L, et al: Preinfarction angina and myocardial preconditioning. Cardiologia 44:963-967, 1999 3. Yellon DM, Dana A: The preconditioning phenomenon: A tool for the scientist or a clinical reality? Circ Res 87:543-550, 2000 4. Wegener S, Gottschalk B, Jovanovic V, et al: Transient ischemic attacks before ischemic stroke: Preconditioning the human brain? A multicenter magnetic resonance imaging study. Stroke 35:616-621, 2004 5. Belayev L, Ginsberg MD, Alonso OF, et al: Bilateral ischemic tolerance of rat hippocampus induced by prior unilateral transient focal ischemia: Relationship to c-fos mRNA expression. Neuroreport 8:55-59, 1996 6. Takaoka A, Nakae I, Mitsunami K, et al: Renal ischemia/reperfusion remotely improves myocardial energy metabolism during myocardial ischemia via adenosine receptors in rabbits: Effects of “remote preconditioning.” J Am Coll Cardiol 33:556-564, 1999 7. Plamondon H, Blondeau N, Heurteaux C, et al: Mutually protective actions of kainic acid epileptic preconditioning and sublethal global ischemia on hippocampal neuronal death: Involvement of adenosine A1 receptors and K(ATP) channels. J Cereb Blood Flow Metab 19: 1296-1308, 1999 8. Meng X, Brown JM, Ao L, et al: Myocardial gene reprogramming associated with a cardiac cross-resistant state induced by LPS preconditioning. Am J Physiol 275:C475-C483, 1998 9. Deng W, Rosenberg PA, Volpe JJ, et al: Calcium-permeable AMPA/ kainate receptors mediate toxicity and preconditioning by oxygen-glucose deprivation in oligodendrocyte precursors. Proc Natl Acad Sci U S A 100:6801-6806, 2003 10. Ikeda T, Ikenoue T, Xia XY, et al: Important role of 72-kd heat shock protein expression in the endothelial cell in acquisition of hypoxic– ischemic tolerance in the immature rat. Am J Obstet Gynecol 182:380386, 2000 11. Wada T, Kondoh T, Tamaki N: Ischemic “cross” tolerance in hypoxic ischemia of immature rat brain. Brain Res 847:299-307, 1999 12. Cai Z, Fratkin JD, Rhodes PG: Prenatal ischemia reduces neuronal injury caused by neonatal hypoxia–ischemia in rats. Neuroreport 8:1393-1398, 1997 13. Corbett D, Crooks P: Ischemic preconditioning: A long term survival study using behavioural and histological endpoints. Brain Res 760:129136, 1997 14. Dowden J, Corbett D: Ischemic preconditioning in 18- to 20-monthold gerbils: Long-term survival with functional outcome measures. Stroke 30:1240-1246, 1999 15. Gidday JM, Fitzgibbons JC, Shah AR, et al: Neuroprotection from ischemic brain injury by hypoxic preconditioning in the neonatal rat. Neurosci Lett 168:221-224, 1994 16. Gidday JM, Shah AR, Maceren RG, et al: Nitric oxide mediates cerebral ischemic tolerance in a neonatal rat model of hypoxic preconditioning. J Cereb Blood Flow Metab 19:331-340, 1999 17. Vannucci RC, Towfighi J, Vannucci SJ: Hypoxic preconditioning and hypoxic–ischemic brain damage in the immature rat: Pathologic and metabolic correlates. J Neurochem 71:1215-1220, 1998 18. Gustavsson M, Anderson M, Mallard C, et al: Hypoxic preconditioning confers long-term reduction of brain injury and improvement of neurological ability in immature rats. Pediatr Res 2004 (in press) 19. Heurteaux C, Lauritzen I, Widmann C, et al: Essential role of adenosine, adenosine A1 receptors, and ATP-sensitive K⫹ channels in cerebral ischemic preconditioning. Proc Natl Acad Sci U S A 92:4666-4670, 1995 20. Cohen MV, Baines CP, Downey JM: Ischemic preconditioning: From adenosine receptor of K ATP channel. Annu Rev Physiol 62:79-109, 2000 21. Ådén U, Leverin AL, Hagberg H, et al: Adenosine A1 receptor agonism in the immature rat brain and heart. Eur J Pharmacol 426:185-192, 2000 22. Grabb MC, Choi DW: Ischemic tolerance in murine cortical cell culture: Critical role for NMDA receptors. J Neurosci 19:1657-1662, 1999 23. Aizenman E, Sinor JD, Brimecombe JC, et al: Alterations of N-methyl- 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. D-aspartate receptor properties after chemical ischemia. J Pharmacol Exp Ther 295:572-577, 2000 Tanaka H, Calderone A, Jover T, et al: Ischemic preconditioning acts upstream of GluR2 down-regulation to afford neuroprotection in the hippocampal CA1. Proc Natl Acad Sci U S A 99:2362-2367, 2002 Huang LE, Arany Z, Livingston DM, et al: Activation of hypoxia-inducible transcription factor depends primarily upon redox-sensitive stabilization of its alpha subunit. J Biol Chem 271:32253-32259, 1996 Bergeron M, Gidday JM, Yu AY, et al: Role of hypoxia-inducible factor-1 in hypoxia-induced ischemic tolerance in neonatal rat brain. Ann Neurol 48:285-296, 2000 Gregg L, Semenza GL: Surviving ischemia: Adaptive responses mediated by hypoxia-inducible factor 1. J Clin Invest 106:809-812, 2000 Jones NM, Bergeron M: Hypoxic preconditioning induces changes in HIF-1 target genes in neonatal rat brain. J Cereb Blood Flow Metab 21:1105-1114, 2001 Bernaudin M, Tang Y, Reilly M, et al: Brain genomic response following hypoxia and re-oxygenation in the neonatal rat. Identification of genes that might contribute to hypoxia-induced ischemic tolerance. J Biol Chem 277:39728-39738, 2002 Juul S: Erythropoietin in the central nervous system, and its use to prevent hypoxic–ischemic brain damage. Acta Paediatr Suppl 91:3642, 2002 Sun Y, Jin K, Xie L, et al: VEGF-induced neuroprotection, neurogenesis, and angiogenesis after focal cerebral ischemia. J Clin Invest 111: 1843-1851, 2003 McLaughlin B, Hartnett KA, Erhardt JA, et al: Caspase 3 activation is essential for neuroprotection in preconditioning. Proc Natl Acad Sci U S A 100:715-720, 2003 Parcellier A, Gurbuxani S, Schmitt E, et al: Heat shock proteins, cellular chaperones that modulate mitochondrial cell death pathways. Biochem Biophys Res Commun 304:505-512, 2003 Rajapakse N, Shimizu K, Kis B, et al: Activation of mitochondrial ATPsensitive potassium channels prevents neuronal cell death after ischemia in neonatal rats. Neurosci Lett 327:208-212, 2002 Cheng Y, Deshmukh M, D’Costa A, et al: Caspase inhibitor affords neuroprotection with delayed administration in a rat model of neonatal hypoxic–ischemic brain injury. J Clin Invest 101:1992-1999, 1998 Nakajima W, Ishida A, Lange MS, et al: Apoptosis has a prolonged role in the neurodegeneration after hypoxic ischemia in the newborn rat. J Neurosci 20:7994-8004, 2000 Zhu C, Wang X, Hagberg H, et al: Correlation between caspase-3 activation and three different markers of DNA damage in neonatal cerebral hypoxia–ischemia. J Neurochem 75:819-829, 2000 Ducrocq S, Benjelloun N, Plotkine M, et al: Poly(ADP-ribose) synthase inhibition reduces ischemic injury and inflammation in neonatal rat brain. J Neurochem 74:2504-2511, 2000 Hagberg H, Wilson M-A, Mutsushita H, et al: Hypoxia–ischemia in immature mice: Disruption of the poly(ADP-ribose) and the polymerase (PARP)-1 gene modifies responses to injury. Dev Neurosci 24:446, 2002 Barone FC, White RF, Spera PA, et al: Ischemic preconditioning and brain tolerance: Temporal histological and functional outcomes, protein synthesis requirement, and interleukin-1 receptor antagonist and early gene expression. Stroke 29:1937-1950, 1998 Semenza GL: Regulation of mammalian O2 homeostasis by hypoxiainducible factor 1. Annu Rev Cell Dev Biol 15:551-578, 1999 Baxter GF, Ferdinandy P: Delayed preconditioning of myocardium: Current perspectives. Basic Res Cardiol 96:329-344, 2001 Giralt M, Penkowa M, Lago N, et al: Metallothionein-1⫹2 protect the CNS after a focal brain injury. Exp Neurol 173:114-128, 2002 Kuan CY, Whitmarsh AJ, Yang DD, et al: A critical role of neuralspecific JNK3 for ischemic apoptosis. Proc Natl Acad Sci U S A 100: 15184-15189, 2003 Wick A, Wick W, Waltenberger J, et al: Neuroprotection by hypoxic preconditioning requires sequential activation of vascular endothelial growth factor receptor and Akt. J Neurosci 22:6401-6407, 2002 Matsushima K, Hakim AM: Transient forebrain ischemia protects against subsequent focal cerebral ischemia without changing cerebral perfusion. Stroke 26:1047-1052, 1995 Preconditioning and the developing brain 47. Chen J, Graham SH, Zhu R, et al: Stress proteins and tolerance to focal cerebral ischemia. J Cereb Blood Flow Metab 16:566-577, 1996 48. Vannucci SJ, Brucklacher RM, Vannucci RC: Hypoxic preconditioning increases brain glycogen, delays energy depletion, and prevents secondary energy failure following hypoxia–ischemia in the immature rat. J Cereb Blood Flow Metab 23:440, 2003 49. Bruce AJ, Boling W, Kindy MS, et al: Altered neuronal and microglial responses to excitotoxic and ischemic brain injury in mice lacking TNF receptors. Nat Med 2:788-794, 1996 50. Wang X, Li X, Currie RW, et al: Application of real-time polymerase chain reaction to quantitate induced expression of interleukin-1 mRNA in ischemic brain tolerance. J Neurosci Res 59:238-246, 2000 51. Cardenas A, Moro MA, Leza JC, et al: Upregulation of TACE/ADAM17 after ischemic preconditioning is involved in brain tolerance. J Cereb Blood Flow Metab 22:1297-1302, 2002 52. Mattson MP, Goodman Y, Luo H, et al: Activation of NF-kappaB protects hippocampal neurons against oxidative stress-induced apoptosis: Evidence for induction of manganese superoxide dismutase and suppression of peroxynitrite production and protein tyrosine nitration. J Neurosci Res 49:681-697, 1997 53. Nawashiro H, Tasaki K, Ruetzler CA, et al: TNF-alpha pretreatment induces protective effects against focal cerebral ischemia in mice. J Cereb Blood Flow Metab 17:483-490, 1997 54. Cheng B, Christakos S, Mattson MP: Tumor necrosis factors protect neurons against metabolic– excitotoxic insults and promote maintenance of calcium homeostasis. Neuron 12:139-153, 1994 55. Strijbos PJ, Rothwell NJ: Interleukin-1 beta attenuates excitatory amino acid-induced neurodegeneration in vitro: Involvement of nerve growth factor. J Neurosci 15:3468-3474, 1995 56. Ohtsuki T, Ruetzler CA, Tasaki K, et al: Interleukin-1 mediates induction of tolerance to global ischemia in gerbil hippocampal CA1 neurons. J Cereb Blood Flow Metab 16:1137-1142, 1996 57. Van Antwerp DJ, Martin SJ, Verma IM, et al: Inhibition of TNF-induced apoptosis by NF-kappa B. Trends Cell Biol 8:107-111, 1998 58. Blondeau N, Widmann C, Lazdunski M, et al: Activation of the nuclear factor-kappaB is a key event in brain tolerance. J Neurosci 21:46684677, 2001 59. Ginis I, Jaiswal R, Klimanis D, et al: TNF-alpha-induced tolerance to ischemic injury involves differential control of NF-kappaB transactivation: The role of NF-kappaB association with p300 adaptor. J Cereb Blood Flow Metab 22:142-152, 2002 60. Lindholm D, Heumann R, Meyer M, et al: Interleukin-1 regulates synthesis of nerve growth factor in non-neuronal cells of rat sciatic nerve Nature 330:658-659, 1987 61. Heese K, Hock C, Otten U: Inflammatory signals induce neurotrophin expression in human microglial cells. J Neurochem 70:699-707, 1998 62. Truettner J, Busto R, Zhao W, et al: Effect of ischemic preconditioning on the expression of putative neuroprotective genes in the rat brain. Mol Brain Res 103:106-115, 2002 63. Yanamoto H, Nagata I, Sakata M, et al: Infarct tolerance induced by intra-cerebral infusion of recombinant brain-derived neurotrophic factor. Brain Res 859:240-248, 2000 64. Jiang X, Zhu D, Okagaki P, et al: N-methyl-D-aspartate and TrkB receptor activation in cerebellar granule cells: An in vitro model of preconditioning to stimulate intrinsic survival pathways in neurons. Ann N Y Acad Sci 993:134-145, 2003 65. Ahmed SH, He YY, Nassief A, et al: Effects of lipopolysaccharide priming on acute ischemic brain injury. Stroke 31:193-199, 2000 66. Toyoda T, Kassell NF, Lee KS: Induction of tolerance against ischemia/ reperfusion injury in rat brain by preconditioning with the endotoxin analog diphosphoryl lipid A. J Neurosurg 92:435-441, 2000 67. Tasaki K, Ruetzler CA, Ohtsuki T, et al: Lipopolysaccharide pre-treatment induces resistance against subsequent focal cerebral ischemic damage in spontaneously hypertensive rats. Brain Res 748:267-270, 1997 68. Zimmermann C, Ginis I, Furuya K, et al: Lipopolysaccharide-induced ischemic tolerance is associated with increased levels of ceramide in brain and in plasma. Brain Res 895:59-65, 2001 69. Boche D, Cunningham C, Gauldie J, et al: Transforming growth factor- 395 70. 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. 87. 88. 89. 90. 91. 92. 93. beta 1-mediated neuroprotection against excitotoxic injury in vivo. J Cereb Blood Flow Metab 23:1174-1182, 2003 Dawson DA, Furuya K, Gotoh J, et al: Cerebrovascular hemodynamics and ischemic tolerance: Lipopolysaccharide-induced resistance to focal cerebral ischemia is not due to changes in severity of the initial ischemic insult, but is associated with preservation of microvascular perfusion. J Cereb Blood Flow Metab 19:616-623, 1999 Bastide M, Gele P, Petrault O, et al: Delayed cerebrovascular protective effect of lipopolysaccharide in parallel to brain ischemic tolerance. J Cereb Blood Flow Metab 23:399-405, 2003 Puisieux F, Deplanque D, Pu Q, et al: Differential role of nitric oxide pathway and heat shock protein in preconditioning and lipopolysaccharide-induced brain ischemic tolerance. Eur J Pharmacol 389:71-78, 2000 Kramer BC, Yabut JA, Cheong J, et al: Lipopolysaccharide prevents cell death caused by glutathione depletion: Possible mechanisms of protection. Neuroscience 114:361-372, 2002 Bordet R, Deplanque D, Maboudou P, et al: Increase in endogenous brain superoxide dismutase as a potential mechanism of lipopolysaccharide-induced brain ischemic tolerance. J Cereb Blood Flow Metab 20:1190-1196, 2000 Eklind S, Mallard C, Leverin AL, et al: Bacterial endotoxin sensitizes the immature brain to hypoxic–ischaemic injury. Eur J Neurosci 13:11011106, 2001 Duncan JR, Cock ML, Scheerlinck JP, et al: White matter injury after repeated endotoxin exposure in the preterm ovine fetus. Pediatr Res 52:941-949, 2002 Altman DI, Young RS, Yagel SK: Effects of dexamethasone in hypoxic– ischemic brain injury in the neonatal rat. Biol Neonate 46:149-156, 1984 Sapolsky RM, Pulsinelli WA: Glucocorticoids potentiate ischemic injury to neurons: Therapeutic implications. Science 229:1397-1400, 1985 Koide T, Wieloch TW, Siesjo BK: Chronic dexamethasone pretreatment aggravates ischemic neuronal necrosis. J Cereb Blood Flow Metab 6:395-404, 1986 Barks JD, Post M, Tuor UI: Dexamethasone prevents hypoxic–ischemic brain damage in the neonatal rat. Pediatr Res 29:558-563, 1991 Chumas PD, Del Bigio MR, Drake JM, et al: A comparison of the protective effect of dexamethasone to other potential prophylactic agents in a neonatal rat model of cerebral hypoxia–ischemia. J Neurosurg 79:414-420, 1993 Tuor UI, Chumas PD, Del Bigio MR: Prevention of hypoxic–ischemic damage with dexamethasone is dependent on age and not influenced by fasting. Exp Neurol 132:116-122, 1995 Williams RS, Benjamin IJ: Protective responses in the ischemic myocardium. J Clin Invest 106:813-818, 2000 Beato M, Klug J: Steroid hormone receptors: An update. Hum Reprod Update 6:225-236, 2000 Palmer C, Roberts RL, Bero C: Deferoxamine posttreatment reduces ischemic brain injury in neonatal rats. Stroke 25:1039-1045, 1994 Nicoll JA, Wilkinson D, Holmes C, et al: Neuropathology of human Alzheimer disease after immunization with amyloid- peptide: A case report. Nat Med 9:448-452, 2003 Weiner HL, Selkoe DJ: Inflammation and therapeutic vaccination in CNS diseases. Nature 420:879-884, 2002 Chen Y, Ruetzler C, Pandipati S, et al: Mucosal tolerance to E-selectin provides cell-mediated protection against ischemic brain injury. Proc Natl Acad Sci U S A 100:15107-15112, 2003 Arnon R, Sela M: Immunomodulation by the copolymer glatiramer acetate. J Mol Recognit 16:412-421, 2003 Lemere CA, Maron R, Selkoe DJ, et al: Nasal vaccination with betaamyloid peptide for the treatment of Alzheimer’s disease. DNA Cell Biol 20:705-711, 2001 Becker K, Kindrick D, McCarron R, et al: Adoptive transfer of myelin basic protein-tolerized splenocytes to naïve animals reduces infarct size: A role for lymphocytes in ischemic brain injury? Stroke 34:18091815, 2003 Faria AM, Weiner HL: Oral tolerance: Mechanisms and therapeutic applications. Adv Immunol 73:153-264, 1999 Cavaillon JM: The nonspecific nature of endotoxin tolerance. Trends Microbiol 3:320-324, 1995