Personnel Protection During Fluoroscopic Procedures Medical Physicist’s Role
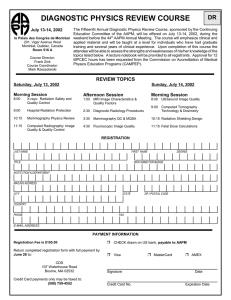
advertisement

CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Medical Physicist’s Role n n Personnel Protection During Fluoroscopic Procedures n n n Beth Schueler Mayo Clinic Rochester, Minnesota n n Procedure room design Movable and personal shielding device selection Fluoroscopic equipment selection Fluoroscopic system optimization Personnel exposure monitoring Personnel exposure investigation Radiation safety training 2 Learning Objectives n n n Stray Radiation Sources What is the nature of stray radiation in fluoroscopic procedures? What can be done to reduce occupational exposure? What regulations must be followed regarding personnel radiation exposure? n n X-ray tube leakage Scatter from patient and objects exposed to the primary beam 3 4 X-Ray Tube Leakage Part 1020.30 (k) Leakage radiation from the diagnostic source assembly: n n n not to exceed 100 mR/hr (0.88 mGy/hr) at 1 m measured at maximum kVp (125-150 kVp) and maximum continuous mA (3-5 mA) n 5 Beth Schueler, AAPM Annual Meeting 2003 Leakage radiation is negligible compared to scatter typical amount of leakage radiation for fluoroscopy of an average adult abdomen: 5 mGy/hr at 1 m 1 0.8 mGy/hr at 1 m n X-Ray Tube Leakage 0.6 0.4 0.2 0 70 80 90 100 110 120 kVp 6 1 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 n Scatter vs Field Size Number of scattered x-rays depends on n the patient entrance skin exposure rate n the patient entrance skin area n the beam energy n n For constant entrance exposure rate and constant kVp, scatter is proportional to the exposure field size Typical scatter value 10 8 Scatter (mGy/hr) Scatter 0.1% of incident exposure at 1 m for a 23-cm FOV n for an entrance skin exposure rate of 20 mGy/min, scatter at 1 m is 20 mGy/min or 1.2 mGy/hr n 6 4 2 0 0 100 200 300 400 2 Field Size (cm ) 7 8 For constant field size and constant kVp, scatter is proportional to the entrance skin exposure rate n 10 Scatter (mGy/hr) n Scatter vs DAP 8 6 For constant kVp, scatter is proportional to the dose-area-product rate (DAP) 4 2 0 0 20 40 60 10 8 Scatter (mGy/hr) Scatter vs Entrance Exposure 6 4 2 0 80 0 Entrance Skin Exposure Rate (mGy/min) 2 10 Scatter vs kVp Scatter: Distribution n 10 8 Scatter (mGy/hr) For constant field size and constant entrance skin exposure rate, scatter increases with kVp 6 Scatter intensity is higher on the entrance side of the exposed volume n 4 2 n 0 60 6 2 9 n 4 DAP Rate (Gy-cm /min) 80 100 120 primary beam most intense on the entrance side forward scatter is heavily attenuated kVp 11 Beth Schueler, AAPM Annual Meeting 2003 12 2 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Stray Radiation: Horizontal Profile Scatter: Distribution n n The entrance skin port should be considered the major radiation source for occupational exposure For actual imaging situations, the scatter distribution is also affected by 0.25 mGy/hr 84 attenuation from unexposed tissue to the side attenuation from the table and pad n shielding by image intensifier, equipment supports, lead shielding devices 2 1 0.5 n n 1m 13 Stray Radiation: Vertical Profile Learning Objectives 180 180 n 0.25 Distance From Floor (cm) 0.5 120 120 34 cm 1.0 mGy/hr 90 90 2.0 4.0 60 60 8.0 30 60 90 150 Patient120 entrance skin Distance dose From = 87 mGy/min Central Ray (cm) 0 30 60 90 120 150 Distance from Central Ray (cm) Distance from Floor (cm) 150 150 n n What is the nature of stray radiation in fluoroscopic procedures? What can be done to reduce occupational exposure? What regulations must be followed regarding personnel radiation exposure? 30 30 180 0 180 15 16 Radiation Safety: Operator Occupational Exposure Reduction n n n What can operators do? What can assisting personnel do? What can medical physicists do? n use short taps of fluoro instead of continuous exposure n use 5-min fluoro-on time warning to maintain awareness of total fluoroscopy time n utilize last-image-hold for image study, discussion and teaching n develop workflow procedures with ancillary personnel so that there is no fluoroscopic exposure when they need to be close to the patient n 17 Beth Schueler, AAPM Annual Meeting 2003 Minimize fluoroscopy beam-on time 18 3 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Radiation Safety: Operator n Radiation Safety: Operator Increase distance from the patient n Remove the grid when possible reduces patient entrance skin exposure and scatter by about a factor of 2 n reduction in image contrast is minimal for n GI: “spoon” palpation device n vertebroplasty: PMMA injection device n other interventional devices: forceps n n n small patients and body parts procedures requiring a large separation between the patient and image intensifier 19 20 Radiation Safety: Operator Lateral Projection: Tube by Operator 90 n Position yourself on the x-ray beam exit side of the patient when possible Scatter at a height of 100 cm 0.25 mGy/hr 60 0.5 30 Scatter intensity is lower on the image intensifier side as compared to the x-ray tube side n For C-arm fluoroscopy, n n n Distance from 0 Table Center (cm) 30 frontal projections: place the x-ray tube under the table lateral and oblique projections: place the x-ray tube on opposite side of the patient 8.0 60 4.0 2.0 90 1.0 mGy/hr 0.5 Distance from Central Ray (cm) 0 21 Scatter at a height of 100 cm n 60 4.0 90 120 150 120 180 22 90 1.0 mGy/hr 2.0 8.0 60 Radiation Safety: Operator Lateral Projection: Tube Opposite Operator 0.5 30 Collimate tightly to the area of interest reduces the entrance skin exposure area improves image contrast n entrance skin exposure may increase n scatter will decrease with collimation as long as there is a decrease in DAP rate n similar result for wedge-shaped beam filters n 30 n Distance from 0 Table Center (cm) 30 60 0.25 mGy/hr 90 Distance from Central Ray (cm) 0 30 60 90 120 150 120 180 23 Beth Schueler, AAPM Annual Meeting 2003 24 4 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Radiation Safety: Operator 10 20 8 18 6 16 4 14 2 12 0 10 0 400 300 200 100 ESER (mGy/min) Scatter (m G y/hr) D AP (G y-cm 2 /m in) Scatter vs Field Size n n DAP General imaging guidelines place the x-ray tube as far as possible from the patient place the II as close as possible to the patient n use magnification modes sparingly n n n Adherence to these guidelines reduces patient entrance skin exposure increases spatial resolution n decreases scatter, but only when collimation is used n n Entrance Skin Field Size (cm 2 ) Scatter Use optimal imaging chain geometry n Use DAP rate as a guide to estimate scatter ESER 25 26 X-Ray Tube Positioning ESER (mGy/min): DAP rate 22 18 Image Intensifier Positioning (Gy-cm2/min): 4.8 4.8 4.3 (mGy/hr): 6.3 6.1 5.2 Scatter rate ESER 36 18 20 (Gy-cm2/min): 5.3 4.6 2.9 (mGy/hr): 6.6 6.5 3.6 (mGy/min): 18 DAP rate Scatter rate 27 Magnification Mode Selection 28 Radiation Safety: Operator n Use movable shielding devices ceiling-suspended shield tableside shield n undertable shield n n ESER 20-cm FOV 28-cm FOV 28-cm FOV 35 18 20 (Gy-cm2/min): 4.5 4.6 2.7 (mGy/hr): 6.4 6.5 3.8 (mGy/min): DAP rate Scatter rate Beth Schueler, AAPM Annual Meeting 2003 29 30 5 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Scatter Levels without Shielding Scatter Levels with Undertable Shielding 180 180 60 60 90 120 150 Distance From Central Ray (cm) 0 30 60 90 120 150 n 90 90 60 60 30 30 0 31 30 60 90 120 Distance From Central Ray (cm) 60 90 120 150 30 180 150 0 180 32 Distance from Central Ray (cm) Occupational Exposure Reduction n 120 4.0 Distance from Central Ray (cm) n 120 1.0 mGy/hr 2.0 30 30 180 0 180 Distance from FromFloor Floor(cm) (cm) Distance 90 90 4.0 150 0.5 120 120 2.0 150 0.25 Distance From Floor (cm) Distance from Floor (cm) 0.5 1.0 mGy/hr 60 180 150 150 0.25 30 180 Radiation Safety: Assisting Personnel What can operators do? What can assisting personnel do? What can medical physicists do? n Make sure you are aware of beam-on cues n Increase your distance from the patient when possible Use movable shielding devices n n warning lights, audio warnings 33 Average-Size Patient Radiation Safety: Operator and Assisting Personnel 180 180 Be aware that scatter is significantly higher for large patients as compared to small patients 150 150 0.25 120 120 entrance skin exposure rate and kVp increases, resulting in higher scatter rates n image quality decreases, beam on-time may also increase n 0.5 24 cm 1.0 mGy/hr 90 90 2.0 60 60 30 60 90 120 150 30 30 180 150 0 180 Distance From Central Ray (cm) 0 35 Beth Schueler, AAPM Annual Meeting 2003 Distance From Floor (cm) Distance from Floor (cm) n 34 30 60 90 120 Distance from Central Ray (cm) 36 6 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Moderately Large-Size Patient Large-Size Patient 180 180 180 180 0.25 150 150 120 120 2.0 90 90 4.0 60 60 30 60 90 120 150 Distance From Central Ray (cm) 0 30 60 90 0.5 120 150 120 120 34 cm 0 180 60 60 8.0 30 60 90 120 150 30 30 180 150 0 180 Distance From Central Ray (cm) 0 37 30 60 90 120 Distance from Central Ray (cm) 38 Personal Shielding Devices Select appropriate personal shielding devices n 90 90 2.0 Radiation Safety: Operator and Assisting Personnel n 1.0 mGy/hr 4.0 30 30 180 Distance from Central Ray (cm) Distance From Floor (cm) Distance from Floor (cm) 0.5 1.0 mGy/hr 29 cm 150 150 Distance From Floor (cm) Distance from Floor (cm) 0.25 n Proper fit is critical n Protective aprons lead equivalent thickness of 0.5 mm recommended, required in some states n wrap-around style needed if side or back faces exposed patient volume n light-weight lead replacements (composites of materials such as barium, tungsten) reduce total weight by 20-30% n n n if 2 layers are needed to meet 0.5 mm leadequivalent requirement, make sure overlap is sufficient arm holes should not be too wide neck line should not fall too low 39 40 Personal Shielding Devices n Personal Shielding Devices Thyroid shields n use recommended if monthly collar badge reading exceeds 4 mSv n significantly reduces effective dose with minimal inconvenience n n Leaded glasses n use recommended if monthly collar badge reading exceeds 4 mSv n side shields needed since user does not typically face the exposed patient volume n 41 Beth Schueler, AAPM Annual Meeting 2003 Leaded gloves 0.5 mm lead equivalent shielding recommended if hands must be in the primary beam n leaded surgical gloves provide partial shielding (3040% attenuation) if hands are in high scatter area n provide minimal protection if hands are in the primary beam: ABC drives up dose rate, protection on one side only 42 7 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Radiation Safety: Physicist Occupational Exposure Reduction n n n What can operators do? What can assisting personnel do? What can medical physicists do? n When constructing or remodeling a fluoroscopic suite, ensure appropriate room design features are incorporated ample procedure room size ample control room size n large viewing windows n intercom system between procedure room and control room n patient table and control area positioned so that no straight-line scatter reaches n n 43 44 Room Design Features n n Operator should be able to view all procedure room entrances from expected operating position Adequate structural shielding in walls, doors, and windows n n Radiation Safety: Physicist n n consider structural shielding in procedure rooms where mobile C-arms are used routinely Movable shielding devices n Ensure fluoroscopic equipment radiation safety design features are considered when specifying a system for purchase ceiling-mounted shields should be included with fluoroscopic equipment installation R&F systems: undertable x-ray tube configuration results in lower personnel exposure as compared to an overtable x-ray tube configuration (for nonremote applications) 45 R&F System: Undertable X-Ray Tube 46 R&F System: Overtable X-Ray Tube 180 180 180 150 150 150 4.0 Distance From Floor (cm) Distance from Floor (cm) 0.5 8.0 2.0 120 120 1.0 mGy/hr 2.0 4.0 90 90 60 120 1.0 mGy/hr 90 60 0.5 60 30 30 0 30 60 60 90 120 Distance From Central Ray (cm) 90 120 Distance from Central Ray (cm) 150 30 180 150 0 180 Distance from Floor (cm) 0.25 30 0.25 47 Beth Schueler, AAPM Annual Meeting 2003 0 30 60 90 120 Distance from Central Ray (cm) 150 0 180 48 8 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Equipment Design Features n n Equipment Design Features Undertable x-ray tube R&F systems (with lead II tower drapes attached) are preferable to C-arm configurations For biplane systems, a lateral C-arm that can be positioned with the II toward the operator is desirable n Imaging chain components that allow positioning for optimal geometry II can be moved close to the patient eliminate spot-film device if not needed n x-ray tube located far from the patient n n n n n Removable or retractable grid Last-image hold and fluoroscopy frame grab Graphic collimator and wedge filter position indicators on last-image hold 49 50 Equipment Design Features n Equipment Design Features Low dose fluoroscopy settings available n pulsed fluoroscopy at 15, 7.5 and lower frames per second n image processing: video frame averaging n use of spectral beam filtration n n n n n n Variable rate digital image acquisition available Patient dose indication available to the operator Digital acquisition zoom Low attenuation tabletop and pad Visible exposure warning lights Method to disable the fluoroscopy foot pedal to eliminate inadvertent exposure during patient removal or prep 51 52 Learning Objectives Radiation Safety: Physicist n Implement and maintain a comprehensive quality control program n work with vendor representatives and operators to find optimal image processing and dose settings to meet clinical imaging needs n perform regular fluoroscopic equipment performance and radiation safety evaluation n perform personal protection device evaluation n n n 53 Beth Schueler, AAPM Annual Meeting 2003 What is the nature of stray radiation in fluoroscopic procedures? What can be done to reduce occupational exposure? What regulations must be followed regarding personnel radiation exposure? 54 9 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 Maximum Permissible Doses n Personal Dosimetry Effective dose (whole body) n Annual: 50 mSv n Cumulative: 10 mSv ´ age in years n n n n Equivalent dose (partial body) n n n Single- and dual-monitor methods single: above protective apron at collar level dual: n n Lens of eye: 150 mSv Skin, hands, feet: 500 mSv n Embryo-fetus: 0.5 mSv/month Monitor 1. above protective apron at collar level Monitor 2. under protective apron at waist level For the dual-monitor method, badges can easily be inadvertently switched n color coding of badges is helpful 55 56 Dose Assignment n n Dose Assignment Individual state regulations vary CRCPD Suggested State Regulations: n for single-monitor, HE = collar reading, or if single-monitor reading > 25% of the dose limit, HE = 0.3 ´ collar reading, or n for dual-monitor, HE = 1.5 ´ waist reading + 0.04 ´ collar reading n n n NCRP Report No. 122 “Use of Personal Monitors to Estimate Effective Dose Equivalent and Effective Dose to Workers for External Exposure to Low-LET Radiation” 1995 n n for single-monitor, E = deep dose reading/21 for dual-monitor, E = 0.5 ´ waist reading + 0.025 ´ collar reading n HE = effective dose equivalent E = effective dose 57 58 Pregnant Workers n n Dose limits apply only after written declaration of pregnancy Conceptus dose assignment method n n n Pregnant Workers n n varies with individual state regulations common method is to wear a monitor under the apron at the waist level estimate projected conceptus dose as 10% of collar badge for 0.5 mm lead-equivalent apron n n if pregnancy planned, monitor under-apron abdominal exposure prior to pregnancy Protection 0.5 mm lead-equivalent aprons are sufficient wrap-around styles critical if back may face radiation source n specially-designed maternity aprons available n n Prediction of conceptus dose n Prediction of conceptus dose Reference: Wagner and Hayman, Radiology 1982: 145: 559 59 Beth Schueler, AAPM Annual Meeting 2003 60 10 CE: Quality Assurance Fluoroscopy 4, TH-B24A-1 References · American Association of Physicists in Medicine, “Managing the Use of Fluoroscopy in Medical Institutions.” AAPM Report No. 58. Madison, WI: Medical Physics Publishing, 1998. · Balter, S. Interventional Fluoroscopy. John Wiley and Sons (2001). · Balter S. “Staff Safety in the Interventional Fluoroscopic Laboratory” in Intravascular Brachytherapy – Fluoroscopically Guided Interventions. Stephen Balter, Rosanna C. Chan, Thomas B. Shope, Jr (eds.). AAPM Monograph No. 28. Proceedings of the 2002 Summer School. Madison, WI: Medical Physics Publishing, pp. 137-163, 2002. · Brateman L. “Radiation safety considerations for diagnostic radiology personnel.” Radiographics 1999; 19:1037-1055. · Geise RA and Hunter DW. “Personnel exposure during fluoroscopy procedures.” Postgraduate Radiology 1988; 8:162-173. · International Commission on Radiological Protection. Avoidance of Radiation Injuries from Medical Interventional Procedures. ICRP Publication 85. Ann ICRP 2000; 20(2). · Marshall NW and Faulkner K. “The dependence of the scattered radiation dose to personnel on technique factors in diagnostic radiology.” Med Phys 1996; 23:1271-1276. · National Council on Radiological Protection and Measurements (NCRP). NCRP Report No. 105. “Radiation Protection for Medical and Allied Health Personnel.” Bethesda, MD: NCRP, 1989. · National Council on Radiological Protection and Measurements (NCRP). NCRP Report No. 122. “Use of Personal Monitors to Estimate Effective Dose Equivalent and Effective Dose to Workers for External Exposure to Low-LET Radiation.” Bethesda, MD: NCRP, 1995. · Wagner LK and Archer BA. Minimizing Risks from Fluoroscopic X-rays – Bioeffects, Instrumentation and Examination (2nd ed.). Houston, TX: Partners in Radiation Management (1998). · Wagner LK and Hayman LA. “Pregnancy and women radiologists.” Radiology 1982; 145:559-562. · World Health Organization. Efficacy and Radiation Safety in Interventional Radiology. Geneva (2000). Beth Schueler, AAPM Annual Meeting 2003