Chapter 25 *Lecture Outline FlexArt PowerPoint figures and tables pre-inserted into PowerPoint
advertisement

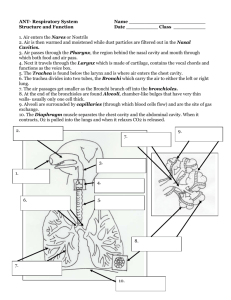
Chapter 25 *Lecture Outline *See separate FlexArt PowerPoint slides for all figures and tables pre-inserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Chapter 25 Outline • General Organization and Functions of the Respiratory System • Upper Respiratory Tract • Lower Respiratory Tract • Lungs • Pulmonary Ventilation • Thoracic Wall Dimensional Changes During External Respiration • Innervation of the Respiratory System • Aging and the Respiratory System • Development of the Respiratory System Figure 25.1 Respiratory System Functions • • • • • The main function of the respiratory system is breathing. This involves both inhalation and exhalation. Some of the other functions are: Gas conditioning Sound production Olfaction Defense Division of the Respiratory System • Anatomically, the system can be divided into upper and lower respiratory tracts. • Functionally, the system can be divided into conducting and respiratory portions. Upper Respiratory Tract The upper respiratory tract is comprised of the following: • nose and nasal cavities • paranasal sinuses • pharynx These are all part of the conducting portion of the respiratory system. Upper Respiratory System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Paranasal sinuses Nasal cavity Frontal sinus Sphenoidal sinus Superior nasal concha Middle nasal concha Inferior nasal concha Vestibule Nostril Hard palate Oral cavity Tongue Superior meatus Middle meatus Nasal Inferior meatus cavity Choanae Pharyngeal tonsil Opening of auditory tube Soft palate Uvula Nasopharynx Oropharynx Laryngopharynx Palatine tonsil Lingual tonsil Epiglottis Larynx Thyroid cartilage Cricoid cartilage Figure 25.2 Esophagus Trachea Pharynx Nose • The nose is the main conducting airway for inhaled air. • It is supported by paired nasal bones superiorly that form the bridge of the nose. • It is supported anteroinferiorly from the bridge by the fleshy, cartilaginous dorsum nasi. Nasal Cavity • The nasal cavity begins as the internal component of the nose and ends as openings to the nasopharynx known as choanae. • The nasal septum divides the nasal cavity into right and left portions and forms the medial wall of each cavity. • The superior, middle and inferior nasal conchae form the lateral wall for each cavity. • The conchae condition the air within the nasal cavity. Paranasal Sinuses Four bones of the skull contain paired air spaces called paranasal sinuses. These spaces make the bones lighter in weight and are named after the bones in which they reside: • frontal • ethmoidal • sphenoidal • maxillary Paranasal Sinuses Figure 25.3 Pharynx One of the few areas of the body that is shared by two organ systems (digestive and respiratory). The pharynx is divided into three regions: • nasopharynx • oropharynx • laryngopharynx Nasopharynx • Continuous with the nasal cavity and superior to the soft palate • Opening of the auditory tubes found in the lateral walls • Posterior nasopharynx wall houses a single pharyngeal tonsil (adenoids) Upper Respiratory System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Paranasal sinuses Nasal cavity Frontal sinus Sphenoidal sinus Superior nasal concha Middle nasal concha Inferior nasal concha Vestibule Nostril Hard palate Oral cavity Tongue Superior meatus Middle meatus Nasal Inferior meatus cavity Choanae Pharyngeal tonsil Opening of auditory tube Soft palate Uvula Nasopharynx Oropharynx Laryngopharynx Palatine tonsil Lingual tonsil Epiglottis Larynx Thyroid cartilage Cricoid cartilage Figure 25.2 Esophagus Trachea Pharynx Oropharynx • Begins at the end of the soft palate and ends at the level of the hyoid bone • The opening of the oral cavity into the oropharynx is the fauces, defined by two pair of muscular arches on the lateral walls of the fauces • The palatine tonsils are embedded in the lateral wall between the arches • The lingual tonsils are at the base of the tongue Laryngopharynx • Starts inferior to hyoid bone and is continuous with the larynx and esophagus Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Paranasal sinuses Nasal cavity Frontal sinus Sphenoidal sinus Superior nasal concha Middle nasal concha Inferior nasal concha Vestibule Nostril Hard palate Oral cavity Tongue Superior meatus Middle meatus Nasal Inferior meatus cavity Choanae Pharyngeal tonsil Opening of auditory tube Soft palate Uvula Nasopharynx Oropharynx Laryngopharynx Palatine tonsil Lingual tonsil Epiglottis Larynx Figure 25.2 Thyroid cartilage Cricoid cartilage Esophagus Trachea Pharynx Regions of the Pharynx Regions of the Pharynx Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Frontal sinus Paranasal sinuses Sphenoidal sinus Superior meatus Superior nasal concha Middle meatus Middle nasal concha Nasal cavity Nasal cavity Inferior meatus Inferior nasal concha Choanae Vestibule Pharyngeal tonsil Nostril Hard palate Opening of auditory tube Oral cavity Nasopharynx Oropharynx Soft palate Uvula Tongue Pharynx Laryngopharynx Palatine tonsil Lingual tonsil Epiglottis Larynx Esophagus Thyroid cartilage Trachea Cricoid cartilage Pharynx: Nasopharynx Oropharynx Laryngopharynx Ethmoidal sinuses Sphenoidal sinus Superior nasal concha Superior meatus Middle nasal concha (b) Regions of pharynx Middle meatus Inferior nasal concha Inferior meatus Vestibule Nasopharynx Hard palate Soft palate Uvula Tongue Oral cavity Oropharynx Dentures Lingual tonsil Laryngopharynx Epiglottis Thyroid cartilage Esophagus Cricoid cartilage Figure 25.2 (a) Sagittal section a: © The McGraw- Hill Companies, Inc./Photo and Dissection by Christine Eckel Lower Respiratory Tract (Conducting Portion) The lower respiratory tract is comprised of the following : • larynx • trachea • bronchi • bronchioles Lower Respiratory Tract (Respiratory Portion) The lower respiratory tract is comprised of the following : • respiratory bronchioles • alveolar ducts • alveoli Lower Respiratory Tract Larynx • • • • Connects pharynx to trachea Also called the voice box Supported by a framework of cartilages, ligaments, and muscles The three major cartilages are: 1. Thyroid cartilage 2. Cricoid cartilage 3. Epiglottis Major Cartilages of the Larynx Figure 25.4 Thyroid Cartilage • • • • Largest cartilage Has an anterior and lateral wall No posterior wall V-shaped anterior projection is called the laryngeal prominence (Adam’s apple) • Usually larger in males than in females because of testosterone influence on growth of cartilage Cricoid Cartilage • Just inferior to the thyroid cartilage • Complete ring-shaped cartilage Figure 25.4 Epiglottis • Spoon-shaped cartilage that projects superiorly into pharynx • Swallowing causes the epiglottis to close the opening to the larynx thus preventing materials from entering the lower respiratory tract Minor Cartilages of the Larynx Although smaller than the three major cartilages, these paired cartilages play an important role in sound production. They are: • arytenoid cartilages • corniculate cartilages • cuneiform cartilages Minor Cartilages of the Larynx Figure 25.5 Sound Production • Vocal folds are found in the larynx and are comprised of vocal ligaments covered by a mucous membrane. • The opening between the vocal folds is the rima glottidis. • The vocal folds plus the rima glottidis are collectively known as the glottis. • When air is forced through the rima glottidis, it causes vibration of the vocal folds, which results in the production of sound. Minor Cartilages of the Larynx Figure 25.5 Trachea • Inferior to the larynx, superior to the primary bronchi, and anterior to the esophagus • 2.5 cm in diameter and 12–14 cm in length • Supported by C-shaped tracheal cartilages Trachea Figure 25.5 Trachea • Posteriorly, the ends of the tracheal cartilages are connected by the trachealis muscle. • The mucosa is lined with pseudostratified columnar epithelium and mucin-secreting goblet cells. Trachea Figure 25.7 Bronchiole Tree • The bronchial tree is a highly branched system of air-conducting passages that begin with the primary bronchi and end with the terminal bronchi. • These passages belong to the conducting portion of the respiratory system. • They reside within the substance of the lungs. Bronchial Tree Figure 25.8 Bronchial Tree • The trachea branches into left and right primary bronchi. • The right primary bronchus is wider and more vertical and foreign particles are more likely to get lodged in this bronchus. • The right primary bronchus divides into three secondary bronchi. • The left primary bronchus divides into two secondary bronchi. • The secondary bronchi divide into 8–10 tertiary bronchi (segmental bronchi). Bronchial Tree As branching continues and the bronchioles become smaller, the following is observed: • Incomplete rings of cartilage become smaller and less numerous • All bronchi are lined with pseudostratified columnar epithelium • Bronchi branch into bronchioles, which lack rings of cartilage and are lined not with pseudostratified columnar epithelium, but simple columnar or simple squamous epithelium Bronchioles • Bronchioles are less than 1 mm in diameter. • Their walls are composed of a relatively thick layer of smooth muscle. • Contraction of the smooth muscle results in a narrowing of the bronchioles called bronchoconstriction. • Relaxation of the smooth muscle results in a widening of the bronchioles called bronchodilation. • Bronchioles branch into terminal bronchioles, which are the last portions of the conduction portion of the respiratory system. Respiratory Portion of the Respiratory System The respiratory portion of the respiratory system consists of: • respiratory bronchioles • alveolar ducts • pulmonary alveoli Bronchioles and Alveoli Figure 25.9 Respiratory Portion of the Respiratory System • Terminal bronchioles branch into respiratory bronchioles. • Respiratory bronchioles branch into alveolar ducts. • Alveolar ducts end with small saccular outpocketings called alveoli. • The thin wall of the alveolus is the structure where respiratory gases (oxygen and carbon dioxide) diffuse between the blood and the air in the lungs. Bronchioles and Alveoli Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Branch of pulmonary artery Bronchiole Terminal bronchiole Respiratory bronchiole Branch of pulmonary vein Arteriole Capillary beds Alveolar duct Alveoli Connective tissue (a) Terminal bronchiole Respiratory bronchiole Alveolar sac Alveolar ducts Alveoli Alveolar duct Alveoli Respiratory bronchiole Figure 25.9 LM 60x (b) SEM 180x (c) b: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser; c: © Dr. David Phillips/Visuals Unlimited Alveolus The alveolar wall is formed from two types of cells: 1. Alveolar type I cells—simple squamous epithelial cells promote rapid diffusion of gases 2. Alveolar type II cells—almost cuboidal in shape and produce pulmonary surfactant, which decreases surface tension within the alveolus and prevents the collapse of alveoli Alveolus Figure 25.10 Respiratory Membrane It is the diffusion barrier across which respiratory gases are exchanged between the blood and the air in the alveoli. It consists of the following: • plasma membrane of the type I alveolar cell • plasma membrane of the capillary cell • fused basement membrane of both cells Respiratory Membrane Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Alveolar Nucleus of capillary connective Nucleus endothelial cell tissue of alveolar Erythrocyte type I cell Diffusion of CO2 Alveolus Respiratory membrane Figure 25.10 Diffusion of O2 Alveolar epithelium Fused basement membranes of the alveolar epithelium and the capillary endothelium Capillary endothelium (b) Capillary Alveolar Macrophages • The alveolar macrophage (dust cell), engulfs any microorganism or particulate matter that makes its way into the alveolus. Lungs and Pleura • Located in pleural cavities on the lateral sides of the thorax and separated by the mediastinum • The pleural cavities and the outer surface of the lung are lined with a serous membrane called pleura • Visceral pleura tightly adheres to the outside of the lung • Parietal pleura lines the pleural cavity itself • These two pleuras are continuous with each other and the space between them is called the pleural cavity Lungs Figure 25.11 Lungs • Conical in shape, has a base inferiorly that rests on the diaphragm and an apex that is the superior most portion of the lung • The apex projects just slightly superior and posterior to the clavicle • The costal surface comes in contact with the ribs and the slightly concave mediastinal surface faces medially toward the mediastinum Lungs Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Apex Superior lobe Horizontal fissure Oblique fissure Oblique fissure Middle lobe Cardiac notch Lingula Inferior lobe Base Right lung Left lung (a) Lateral views Apex Superior lobe Oblique fissure Oblique fissure Pulmonary arteries Hilum Hilum Primary bronchi Horizontal fissure Middle lobe Pulmonary veins Cardiac impression Inferior lobe Oblique fissure Cardiac notch Oblique fissure Base Figure 25.12 Right lung Left lung (b) Medial views Lungs • The mediastinal surface houses a concave region called the hilum. • Bronchi, pulmonary vessels, lymphatic vessels, and nerves pass into and out of the lungs in this region. • Collectively, all structures within the hilum are termed the root of the lung. Left Lung • Slightly smaller than right lung because heart projects slightly to the left of midline • Heart makes a medial surface indentation called the cardiac impression • Has an anterior indented region called the cardiac notch • Has an oblique fissure that divides the lung into two lobes (superior and inferior lobes) • The lingula is homologous to the middle lobe of the right lung Lungs Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Apex Superior lobe Horizontal fissure Oblique fissure Oblique fissure Middle lobe Cardiac notch Lingula Inferior lobe Base Right lung Left lung (a) Lateral views Apex Superior lobe Oblique fissure Oblique fissure Pulmonary arteries Hilum Hilum Primary bronchi Horizontal fissure Middle lobe Pulmonary veins Cardiac impression Inferior lobe Oblique fissure Cardiac notch Oblique fissure Base Figure 25.12 Right lung Left lung (b) Medial views Right Lung • Has two fissures, oblique and horizontal fissures that divide the lung into three lobes (superior, middle and inferior lobes) Bronchopulmonary Segments • There are 10 bronchopulmonary segments in the right lung and 8–10 in the left lung. • Each segment is supplied by its own tertiary bronchus and a branch of a pulmonary artery and vein. • Each segment is surrounded by and isolated from other segments by connective tissue. Bronchopulmonary Segments Figure 25.13 Blood Supply to and from the Lungs • • The pulmonary circulation (see figure 23.22) conducts blood to and from the gas exchange surfaces of the lungs. The bronchial circulation is a component of the systemic circulation that delivers blood directly to and from the bronchi and bronchioles. Lymphatic Drainage • Lymph nodes and vessels are located within the lungs and around the bronchi and pleura. • Lymph nodes collect particulate matter. • Lymph first goes to the pulmonary lymph nodes within the lungs. • Lymph then goes to the bronchopulmonary lymph nodes at the hilum of the lung. • Lymph then goes to the tracheobronchial lymph nodes and then into the left and right bronchomediastinal trunks (see Chapter 24). Lymphatic Drainage Figure 25.14 Pulmonary Ventilation • Breathing, also known as pulmonary ventilation, is the movement of air into and out of the respiratory system. • Movement of gases follows Boyle’s law. • During inhalation, the volume of the thoracic cavity increases, intrapulmonary pressure decreases, and air flows into the lungs. • During exhalation, the opposite is true. Thoracic Wall Dimensional Changes During Respiration During inhalation and exhalation, the thoracic cavity changes in all three dimensions: • Vertical—movement of the diaphragm • Lateral—muscles attached to ribs • Anterior/Posterior—muscles attached to ribs Muscles attached to ribs that aid in lateral and anterior/posterior changes of the ribs are as follows: • Scalene=Forced inhalation •Pectoralis minor=Forced inhalation •Sternocleidomastoid=Forced inhalation • External intercostal=normal inhalation • Internal intercostal=Forced exhalation • Transverse thoracis=normal exhalation • Serratus posterior superior=normal inhalation • Serratus posterior inferior=normal exhalation •Abdominals=active exhalation Thoracic Wall Dimensional Changes During Respiration Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Inhalation Exhalation Thoracic cavity Thoracic cavity Vertical changes Diaphragm contracts; vertical dimensions of thoracic cavity increase. Diaphragm relaxes; vertical dimensions of thoracic cavity narrow. Lateral changes Ribs are elevated and thoracic cavity widens. Ribs are depressed and thoracic cavity narrows. Anterior-posterior changes Figure 25.15 Inferior portion of sternum moves anteriorly. Inferior portion of sternum moves posteriorly. Muscles Involved in External Respiration Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. (a) Inhalation Scalene muscles elevate 1st and 2nd ribs External intercostal muscles elevate ribs Inferior part of sternum moves anteriorly Diaphragm moves inferiorly during contraction (b) Exhalation Transversus thoracis depresses ribs Internal intercostal muscles depress ribs Inferior part of sternum moves posteriorly Diaphragm moves superiorly as it relaxes a(2)-b(2): © SIU/Visuals Unlimited Figure 25.16 Innervation of the Respiratory System • The larynx, trachea, bronchial tree, and lungs are under autonomic control. • Sympathetic and parasympathetic fibers form the pulmonary plexus, which is a weblike network of nerve fibers that surrounds the primary bronchi and enter the lungs at the hilum. • Sympathetic stimulation results in bronchodilation. • Parasympathetic stimulation results in bronchoconstriction. Respiratory Control Centers in the Brainstem • The respiratory rhythmicity center in the medulla oblongata controls the rate and depth of breathing. • The dorsal respiratory group (DRG) controls inhalation by stimulating muscles of inspiration. • The ventral respiratory group (VRG) controls forced exhalation. Respiratory Control Centers in the Brainstem Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Stimulation Inhibition Pneumotaxic center Pons Apneustic center Respiratory rhythmicity center Ventral respiratory group (VRG) Dorsal respiratory group (DRG) Medulla oblongata Internal intercostal muscles Figure 25.17 External intercostal muscles Diaphragm Respiratory Control Centers in the Brainstem • The pons houses the apneustic center and the pneumotaxic center. • Both centers influence the breathing rate by modifying the activity of the respiratory rhythmicity center. • The pneumotaxic center is inhibitory to both respiration and the apneustic center. • The apneustic center stimulates the inspiratory center in the medulla. Smoking, Emphysema, and Lung Cancer Part 1 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Dilated, nonfunctional air spaces (a) Dilated, nonfunctional alveoli LM 15x (b) a: © CNRI/Photo Researchers, Inc.; b: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser Smoking, Emphysema, and Lung Cancer Part 2 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Squamous cell carcinoma © Dr. E. Walker/ Photo Researchers, Inc. Small-cell carcinoma © Javier Domingo/Phototake a: © CNRI/Photo Researchers, Inc.; b: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser Development of the Respiratory System Figure 25.18 Summary of Respiratory System Development