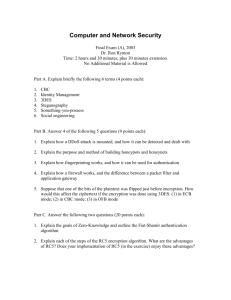
Neurofibromatosis By Nilesh Jambhekar
advertisement

Neurofibromatosis By Nilesh Jambhekar What is Neurofibromatosis? The basics: Autosomal-dominant genetic disorder. Is a type of cancer of the nervous system that can occur in all 3 germ layers and any organ system. Causes small (usually benign) tumors to start growing on neural crest cells (Schwann Cells, oligodendrocytes, melanocytes, etc.) 2 main types: -Neurofibromatosis 1(NF1) -Neurofibromatosis 2(NF2) [1] Neurofibromatosis 1: Caused gene. by a mutation on the NF1 (Neurofibromin1) -is on chromosome 17 on the long arm (q) at position 11.2 -has 60 exons and over 8500 base pairs -encodes for Neurofibromin NF1 is the more common form of the disease . Occurs in ~1/3000 live births (in the U.S.). [1] Is also called von Recklinghausen syndrome after Friedrich Daniel von Recklinghausen who discovered it in 1882. [2] Causes tumors to develop in the peripheral nervous system or along the optic nerve. [1] Diagnosing Neurofibromatosis 1 Must have at least 2 of the following: Six or more café-au-lait spots 1.5 cm or larger in postpubertal individuals, 0.5 cm or larger in pre-pubertal individuals Two or more neurofibromas of any type or one or more plexiform neurofibroma Freckling in the axilla or groin Optic glioma (tumor of the optic pathway) Two or more Lisch nodules (benign iris hamartomas) A distinctive bony lesion: dysplasia of the sphenoid bone or dysplasia or thinning of long bone cortex A first-degree relative with NF1[1] A young boy café-au-lait spots Source: www.understandingnf1.org Neurofibromin (NF1): Is produced by many cells in the nervous system (nerve cells as well Schwann cells and oligodendrocytes). Acts as a GTPase activating protein (GAP) that specifically regulates the activity of RAS, a family of GTPases . Acts as a tumor suppressor. Any one of hundreds of possible mutations in NF1 incapacitate Neurofibromin causing nerve cells to proliferate unchecked (tumors). Because the NF1 gene is so large, mutations are relatively frequent but not always detrimental. Neurofibromin is a very large protein (2839 amino acids). The cellular role of Neurofibromin is still not known. [2][4] RAS: RAS is a family of genes that encode small GTPases such as H-RAS. RAS has a molecular switch with 2 modes: on and off. In its “on” mode, RAS is bound to GTP and interacts with a growth activator called proto oncogene c-RAF. RAS activates intrinsic properties within c-RAF activating it. This activates a pathway of kinases leading to cell growth. [6][8] Neurofibromin mechanism: Turns off the growth-promoting function of the RAS family by hydrolyzing the GTP bound to them. Normally, RAS is active while it slowly cleaves off a terminal phosphate using the time to initiate various kinase pathways that lead to cell growth and proliferation. Neurofibromin essentially catalyzes this reaction. Neurofibromin is also known to have effects on cAMP signaling in other pathways, but most of these connections aren’t well understood.[7] Fig 2 There are many known mutations of Neurofibromin but the most serious involve the mutations of the above 3 residues (Glutamic acid, Lysine, and especially Arganine). The Arganine Finger The Arganine finger (residue 1276) is the single most important part of the GAP domain in terms of catalyzing the removal of the gamma (terminal) phosphate. Replacement of this residue by any other will result in a several fold decrease in complex stability and up to a 8000 fold decrease in the catalytic ability of Neurofibromin. Replacement of K1423 and E1437 will also decrease the stability of the above complex as well. [11] General ( very simplified) NF1 Pathway: Fig. 3: Neurofibromatosis 2: Caused by a mutation in the NF2 gene. -Is on Chromosome 22 at location q 11-13.1. -Encodes a protein called MERLIN (Moesin-Ezrin-Radixin-Like Protein) Causes tumors to develop in the CNS, especially in cranial nerve VIII connecting the inner ear with the brain. - Causes a variety of symptoms related to the ear: deafness, ear ringing, and difficulty keeping balance. - Less common form of NF1 with an occurrence of ~1/(30000-40000) births in the U.S.[1] Is MERLIN: 595 amino acids long: Residues 1-302->N-terminal region, residues 303-478->alpha-helix region, residues 479-595-> C-terminal region. Is a membrane-cytoskeleton scaffolding protein which binds actin filaments to the cell surface glycoproteins. Resides in cellular (adherens) junctions and membrane ruffles in isolated cells where it acts as a tumor suppressor by means of contact-mediated growth inhibition. Merlin has a closed form in which it is active and an open form in which it is not. Without a functional MERLIN, cells cannot recognize each other when the contact and continue to grow even when they have no space.[3] MERLIN’s Intramolecular Associations: Like other members of the ERM family (Ezrin, Radixin, and Moesin), MERLIN’s interactions with itself are crucial to its function. 2 main types of interactions: N-terminus/N-terminus and N-terminus/C-terminus. The N/N-terminus interactions are necessary for the N/C-terminus interactions. The N/C-interactions also require residues 302-308 and an intact exon 17 ( residues 580-595). [5] 4 5 MERLIN’s Possible Mechanisms: The full scope of Merlin’s f tumor suppression isn’t known. Most of MERLIN’s tumors suppression abilities come from its ability to inhibit the activity of RAS GTPases. RAS also inhibits MERLIN by initiating a pathway ending with the phosphorylation of Serine 518 by PAK-1 which causes MERLIN to become open and switch off. There are other such feedback loops. Recent studies show that another possible mechanism by which Merlin acts is binding to E3 ubiquitin ligase-CRL4DCAF1 complex(which is crucial in ribosome genesis) in the cell nucleus and suppressing its activity.[3][10] The Activation of RAS Fig 6 : Receptor Tyrosine Kinases and RAS. The pathway involves the GRB2, a key target for MERLIN. Source: www.ncbi.nlm.nih.gov Complete (simplified) MERLIN-RAS pathway: Fig. 7: Fig : The MERLIN-RAS pathway is filled with chains of Kinases and feedback loops. Fig 8: The all-important RAS: • The RAS family is at the heart of both forms of Neurofibromatosis. • In general, there seems to be a trend in cancers involving mutations upstream that lead to protein kinases proliferating cell growth. This chain of kinases begins with a member of the RAS family such as H-RAS (right). As such, RAS is a topic of interest for researchers trying to cure all forms of cancer, not just neurofibromatosis. [3][5][8] Fig 9 : H-RAS In complex with GCP (an analog of GDP) The Financial Costs of Neurofibromatosis: The costs associated with both forms of neurofibromatosis depends greatly upon how severe the disease is. Patients with more severe forms may require expensive medical procedures such as surgery. According to the British Journal of Dermatology, the average patient with Neurofibromatosis (1) has about £810 ($1215) in medical costs. Medical costs are probably higher, though there seems to be no such study performed in the US. The direct overall costs in the US are probably around $200 million, given the above estimate holds true for the U.S. How Neurofibromatosis Effects the Body: Source: www.NFINC.org Meet Yvonne Foong: When Yvonne was 16 years old, she was diagnosed with Neurofibromatosis 2. The disease took an overwhelming toll on the young athlete, who used to practice karate, ballet, figure skating, and even singing in her school choir. Soon she lost her ability to hear and walk properly. MRI scans showed a large brain tumor growing in her inner ear affecting her hearing and several smaller ones in her spine affecting motor function. Source: yvonnefoong.com Since Then: Yvonne has undergone 1 spine surgery and 3 separate brain surgeries. To help defray the costs, Yvonne has written 2 books outlining her struggles with the disease and her experiences through it all. Her story came out in the October 08’ issue of Marie Claire magazine. Through all this Yvonne is optimistic: “fear not. I am excited and anticipating my next surgery and the wonders it would lead to.” Source: yvonnefoong.com Hope for a cure? As of now, the methods to deal with any form of neurofibromatosis target the symptom and not the disease mechanism itself. BAY 43-9006 (Sorafenib), a new drug being developed by Onyx Pharmaceuticals in conjunction with Bayer Pharmaceutical Group targets cRAF and could potentially treat both forms of neurofibromatosis. So far the drug is in Phase I of clinical trials, so it won’t be available any time soon. [12] Source: Clinicaltrials.gov How BAY 43-9006 (Sorafenib) works: Sorafenib seems to cause the phosphorylation of serines on a variety of kinases (particularly RAF-1) inhibiting their activity. It also dephosphorylates serines 75 & 99 on an apoptotic protein called BAD turning it on. Similarly it activates BAK and BAX. Together these cells increase the rate of cellular apoptosis. Sorafenib also causes a reduction in the mitochondrial membrane potential inhibiting respiration. [12] References: 1. 2. 3. 4. U.S. National Library of Medicine. “Neurofibromatosis. “Genetics Home Reference. National Institute of Health, March 2007. Web. 5 April 2010. Davis, Ronald. “Neurobiology: Neurofibromin Progress on the Fly.”Nature 403 (2000): 846-847. 1 April 2010. JY Lim, Kim H, Jeun SS, Kang SG, Lee KJ. “Merlin inhibits growth hormone-regulated Raf-ERKs pathways by binding to Grb2 protein.” Biochemical and Biophysical Research Communications 340.4 (2006): 1151-1157. 3 April 2010. Scheffzek K, Ahmadian MR, Wiesmüller L, Kabsch W, Stege P, Schmitz F, Wittinghofer A. “Structural analysis of the GAP-related domain from neurofibromin and its implications.” EMBO J.17.15 More References: 5.) Li, Wei, Liru You. “Merlin/NF2 Suppresses Tumorigenesis by Inhibiting the E3 Ubiquitin Ligase CRL4DCAF1 in the Nucleus.”Cell 140.4 (2010): 477-90. 29 March 2010. 6.) Klose, Anja, M. Rheza Ahmadian. “Selective disactivation of neurofibromin GAP activity in neurofibromatosis type 1 (NF1).” Oxford University Press 7.8 (1998): 1261-1268. 29 March 2010. 7.) Dasgupta, Bislab, Laura Dugan. “The Neurofibromatosis 1 Gene Product Neurofibromin Regulates Pituitary Adenylate Cyclase-Activating Polypeptide-Mediated Signaling in Astrocytes.”The Journal of Neuroscience 23.26 (2003): 89498954. 29 March 2010. 8.) Guha, A, N. Lau. “Ras-GTP levels are elevated in human NF1 peripheral nerve tumors.”Oncogene 12.3 (1996): 507-13. 30 March 2010. Even More References: 9.) Fraz A. Ismat, Junwang Xu, Min Min Lu and Jonathan A. Epstein. ”The Neurofibromin GAP-related Domain Rescues Endothelial But Not Neural Crest Development in Nf1–/– mice.” J. Clin. Invest. 116.9 (2006): 2378-2384. 12 April 2010. 10.) NCBI. Molecular Cell Biology. Baltimore: W. H. Freeman and Company, 2000. Print. 11.) Rob te Biesebeke,‡ Ivo M. Krab,§ and Andrea Parmeggian. “The Arginine Finger Loop of Yeast and Human GAP Is a Determinant for the Specificity toward Ras GTPase.” Biochemistry.40.25 (2001): 7474–7479. 3 April 2010. 12.) David J. Panka1, Wei Wang2, Michael B. Atkins1 and James W. Mier1. “The Raf Inhibitor BAY 43-9006 (Sorafenib) Induces CaspaseIndependent Apoptosis in Melanoma Cells.” Cancer Research 66 (2006) 1611-19. 13 April 2010.